Child Neurology Through Case Histories by Vinay Puri, MD
advertisement

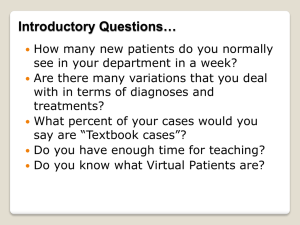
Learning Child Neurology Through Case Histories Vinay Puri MBBS, FAAN Professor in Neurology and Pediatrics Director and Founder Division of Child Neurology University of Louisville Neurologist in chief Kosair children’s hospital Division of Child Neurology Physicians: Anna Ehret Darren Farber Mike Sowell Karen Skjei - Epilepsy Vinay Puri Martin Brown - Neuromuscular Disorders Suma D* Greg Barnes* - Epilepsy & Autism Research Nurse Practitioners Paula Hartmann Angela Bishop Britt Schloemer Vanessa Rupee Staci Crocker Stephanie Sims Kristin Schircliff Nurse Clinicians Terra Cummins Lindsey Reed Email:v0puri01@louisville.edu Office:601 S Floyd # 500 Louisville – KY 40205 Tel: 502-5898033 Fax: 502-5898233 My Assistant : Miranda Der Ohanian Miranda.derohanian@ulp.org Office manager:Heather Ball BS, MS h0ball01@ulp.org Our Service Locations: Louisville- All patients Commission Clinics:* Louisville* Elizabethtown* Owensboro* Paducah* Bowling Green* Specialty Services: MDA/Neuromuscular Clinic Spasticity Clinic Brain Tumor Clinic- 5025831697 New Onset seizure Clinic Neurogenetics Clinic Stroke Clinic Tuberose Sclerosis & NF Clinic Ketogenic Diet Clinic Our Goals Quality Timely Patient centered services Easy access Presentation will consist of cases and a collection of representative videos: The session will be highly interactive Listen Carefully to the parent Help jog memory, be specific in asking questions No shortcuts All aspects of history to be leveraged Vital signs General examination- head size, dysmorphic, skin exam Neurological examination- walking !! Lab testing Imaging Assessment Recommendations Staring spells in my 9 year old child: Describe the spells to me Imitate a spell Do you have it on video Examine the child Maybe EEG What are the causes of staring spells Pitfalls My baby is having jerking of his legs and arms: Describe the events to me Do not interrupt the parent when they are describing the spells Do you have a video of the spells Awake/asleep or both May need an EEG or a video EEG Common Pitfalls My child is not athletic and is lazy: What do you mean exactly How long Family history Examine the child what specifically will you look for Common Pitfalls My child is developmentally delayed: Explain it to me Motor, Language, Cognitive and Social To what degree and what combination of delay Specific considerations Work up: Neuroimaging, Genetic & Metabolic My child is having abnormal movements Describe it to me Detailed history, age of onset, when, effect of sleep, movement, medications etc Look at videos if any Careful examination of child • For localization of lesion in CNS, history is as important as PE. First step is to localize the lesion to an anatomical site. ANATOMICAL DIAGNOSIS • Is the lesion UMN/LMN • If it is UMN lesion, is the lesion in the brain/Spinal cord • If the lesion is in the brain, is it in cortex, subcortex (corona radiata), basal ganglia, internal capsule, midbrain, pons, medulla or cerebellum. • If the lesion is in the spinal cord, which level of spinal cord is involved. • If it is a LMN lesion, which structure is involved, anterior horn cell, radicles, peripheral nerve, NMJ or muscle. Etiological diagnosis: • Acute – stroke, demyelination, infection • Subacute- infection, inflammation • Insidious- Tumors, degenerative diseases. • • • • • Progression Congenital – CP, not progressive Vascular – maximum deficit at onset(with in about 72 hours of onset) and then child gradually recovers. Demyelinating – GBS(progresses for sometime and then recovers partially or completely), MS(waxing and waning or intermittent progression) Degenerative- gradual progression. Neoplastic – gradual progression. Common Co Morbidities and concerns in Child Neurology: Sleep disorders Mood disorders ADHD Learning disabilities Common questions to consider & teaching points: Does my child have Cerebral Palsy Was it a seizure Missed diagnosis of tics Is my child weak MRI or CT Always sleep deprived EEG In Conclusion: • • • • • • • Listen carefully Keep an open mind Leverage all information and data Examination can be quick and thorough Must examine fundus in headache patients See the child walk Have child get up from ground if any concerns about weakness at all • A normal test does not always exclude diagnosis • An abnormal test does not rule in diagnosis QUESTIONS PLEASE?