Powerpoint - Families USA
advertisement
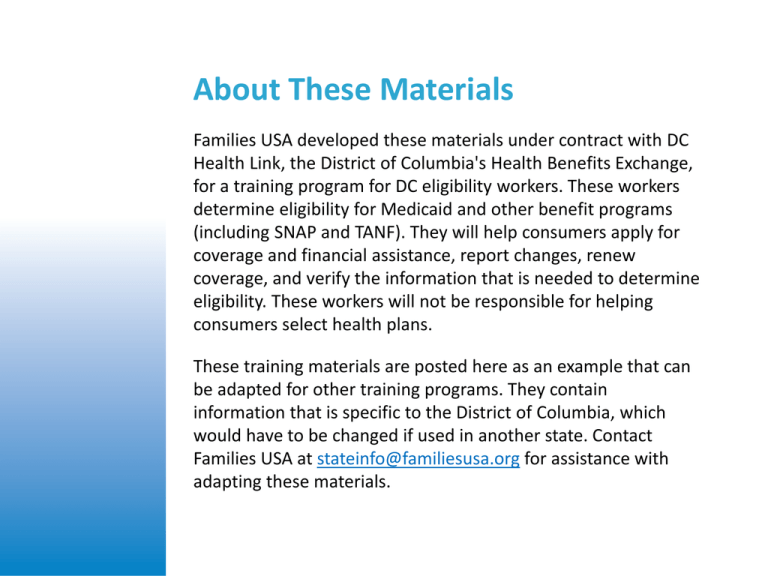
About These Materials Families USA developed these materials under contract with DC Health Link, the District of Columbia's Health Benefits Exchange, for a training program for DC eligibility workers. These workers determine eligibility for Medicaid and other benefit programs (including SNAP and TANF). They will help consumers apply for coverage and financial assistance, report changes, renew coverage, and verify the information that is needed to determine eligibility. These workers will not be responsible for helping consumers select health plans. These training materials are posted here as an example that can be adapted for other training programs. They contain information that is specific to the District of Columbia, which would have to be changed if used in another state. Contact Families USA at stateinfo@familiesusa.org for assistance with adapting these materials. ESA Policy Training Day 1 Overview • Why is the Affordable Care Act changing Medicaid and private insurance? • How is Medicaid changing in DC? • What is DC Health Link? • How do premium tax credits and cost-sharing reductions work? • What happens if income changes? Prepared by Families USA for use in the District of Columbia Background on the Affordable Care Act Prepared by Families USA for use in the District of Columbia Why is the Affordable Care Act changing Medicaid and private insurance? • Many people are currently uninsured • Antiquated eligibility systems are hard for workers and consumers to use • Private insurance is expensive • Consumer protections are limited • Pre-existing conditions lead to denials of coverage Families USA 2013 Prepared by Families USA for use in the District of Columbia The District of Columbia DC is a leader in coverage, but nearly 7% are still uninsured. • DC covers adults up to 200% of poverty and kids up to 300% • Unlike most states, DC already covers childless adults But there is still work to do . . . • Total Uninsured Population: U.S. - 15.1% DC - 6.9% • Number of Uninsured People in DC, 2011: 42,007 Source: CBPP analysis of Census Bureau data from the American Community Survey 2011 Prepared by Families USA for use in the District of Columbia New Affordable Care Act Protections: 2014 • Those who do not qualify for Medicaid (due to income or five-year bar) can get new premium tax credits • Low-income adults will newly qualify for Medicaid in many states (but they are already covered in DC) • People can apply online and verify information electronically • Private insurers cannot deny people coverage or charge them more because they are sick Prepared by Families USA for use in the District of Columbia DC Medicaid and the Affordable Care Act Prepared by Families USA for use in the District of Columbia Medicaid Will Stay the Same for Most People • DC is preserving its good coverage levels • DC is modernizing applications, eligibility determinations, and renewals Prepared by Families USA for use in the District of Columbia Modernizing Eligibility Determinations • Most applications can be done online • Numerous eligibility categories not necessary • Electronic verification will be used when possible • New application will determine eligibility for Medicaid and premium tax credits Prepared by Families USA for use in the District of Columbia MAGI and Non-MAGI Eligibility Eligibility for most Medicaid recipients will be determined using new system • New MAGI (Modified Adjusted Gross Income) rules • Used for parents/caretaker relatives, children, pregnant women, and childless adults aged 21-64 Prepared by Families USA for use in the District of Columbia MAGI and Non-MAGI Eligibility (cont’d) Eligibility for some will still be done by ESA for now • Used for those who are aged, blind, disabled, or need long-term care services • We call this the “Non-MAGI” population Prepared by Families USA for use in the District of Columbia MAGI Income • Based on how IRS calculates tax income • Example: Instead of subtracting income disregards and deductions from income like we do today, take away adjustments to income • New system will calculate all of this for you Prepared by Families USA for use in the District of Columbia MAGI Household Composition • New way of defining household based on who is on the same tax return (if family files taxes) • Some exceptions in Medicaid • Different rules for families that do not file taxes • New system will determine household composition for you Prepared by Families USA for use in the District of Columbia Introduction to DC Health Link Prepared by Families USA for use in the District of Columbia How DC Health Link Works New marketplace for private insurance for individuals, families, and small businesses • Provides clear, comparative information about plans from different insurance companies • Some will get help paying premiums for these plans • Includes only plans that meet quality standards Prepared by Families USA for use in the District of Columbia What is your role in DC Health Link? • ESA workers will help DC residents apply for coverage • New system uses one application for: • Medicaid • Premium tax credits for DC Health Link plans Prepared by Families USA for use in the District of Columbia Overview 1. What are DC Health Link plans like, and how will DC residents be able to compare plans? 2. What type of assistance is available to people buying DC Health Link plans? Prepared by Families USA for use in the District of Columbia What will DC Health Link plans cover? • Coverage similar to that offered by most employers • All plans must cover a minimum benefits package, called Essential Health Benefits (EHB) Essential Health Benefits (EHB) 1. Outpatient services 6. Prescription drugs 2. Emergency services 7. Rehabilitative and habilitative services 3. Hospitalizations 8. Laboratory services 4. Maternity and newborn care 9. Preventive services 5. Mental health and substance use disorder services (no day or visit limits in DC) 10. Pediatric services (includes oral and vision care) Prepared by Families USA for use in the District of Columbia Medicaid Benefits Differ from DC Health Link Benefits Medicaid covers more than the Essential Health Benefits and does not charge enrollees premiums, so it is important to help people who qualify get Medicaid instead. All applicants to DC Health Link will be assessed for Medicaid eligibility. Medicaid covers the 10 Essential Health Benefits, PLUS: EPSDT (Early and Periodic Screening, Diagnostic, and Treatment) services to children under 21 Access to federally qualified health centers Family planning services Emergency and non-emergency transportation to medical care Prepared by Families USA for use in the District of Columbia Different Levels of DC Health Link Plans Plans offered in four metal levels: Metal Level Generosity Platinum (highest monthly premiums) Covers about 90% of medical care costs Gold Covers about 80% of medical care costs Silver Covers about 70% of medical care costs Bronze (lowest monthly premiums) Covers about 60% of medical care costs Note: Measured based on total cost of covered benefits for a typical population Prepared by Families USA for use in the District of Columbia Understanding Metal Levels • Platinum plan: Premiums cost the most, but plan pays more (and patient pays less) for health care services • Bronze plan: Premiums cost the least, but plan pays less (and patient pays more) for health care services • Silver and gold plans: Somewhere in between Prepared by Families USA for use in the District of Columbia Hypothetical Plans Metal Level Full Premium Price at Age 40 Deductible Patient Co-Pay for Sick Care Doctor Visit Platinum $460 $0 $20/primary $40/specialty Gold $370 $0 $30/primary $50/specialty Silver $295 $2000 $45/primary $65/specialty Bronze $230 $5000 $60/primary $70/specialty Prepared by Families USA for use in the District of Columbia Why are we talking about these costs? We’ll come back to these plan levels when we talk about premium tax credits and cost-sharing reductions. People who get premium tax credits will also have to choose a metal level plan. Prepared by Families USA for use in the District of Columbia Premium Tax Credits Prepared by Families USA for use in the District of Columbia Premium Tax Credits: The Basics • Premium tax credits help people pay for health insurance if they do not have job-based coverage, Medicaid, or Medicare • Premium tax credits pay a certain amount of monthly premiums, based on income • Through DC Health Link, people can get tax credits monthly based on expected annual income • At tax time, premium tax credits are adjusted based on actual annual income Prepared by Families USA for use in the District of Columbia Example: Lower Monthly Premiums Latisha, age 55, has a small catering business. A health plan charges her $420/month in premiums, which is a huge portion of her income of $34,000/year. She applies to DC Health Link and is found eligible to enroll in a plan with premium tax credits. With the tax credits, she pays $265/month for a silver plan. Prepared by Families USA for use in the District of Columbia Lower Incomes, More Help The less income someone has, the less he or she has to pay. Example: With income at 100% of the poverty level ($11,490 for an individual), a person pays 2% of income for a silver plan’s premiums. With income at three times the poverty level ($34,470), a person pays 9.5% of income for the same silver plan’s premiums. Prepared by Families USA for use in the District of Columbia The Amount People Pay Depends on the Plan They Choose • Premium tax credit amounts are based on the cost of a silver plan. If a person or family wants more comprehensive coverage, they can buy a gold or platinum plan and pay the difference. • Those who want lower premiums can buy a bronze plan, but they would face higher costs for medical care. Prepared by Families USA for use in the District of Columbia Example • A silver plan costs $400. Keisha’s tax credit is: $400 (full cost) - $120 (expected contribution) = $280 credit. • A bronze plan costs $300. Keisha can use her tax credit for this, and her monthly premium would be only $20 ($300 - $280 = $20), but she’ll have higher copayments or a higher deductible in this plan. Prepared by Families USA for use in the District of Columbia Income Changes • People can report their income changes to get premium tax credits and cost-sharing reductions adjusted • If someone’s annual income is higher than projected, he or she may have to pay back excess premium tax credits up to a cap (this is called “reconciliation”) • If someone’s income is lower than projected, he or she will get more in premium tax credits at the end of the year • Cost-sharing reductions do not need to be paid back Prepared by Families USA for use in the District of Columbia Review: Question #1 TRUE or FALSE: If a person receiving premium tax credits has an increase in income and does not report it, she may end up owing some of her premium tax credit back at the end of the year. Prepared by Families USA for use in the District of Columbia Answer: Question #1 TRUE Not reporting an increase in income could mean that a person needs to pay back some of her premium tax credit. Prepared by Families USA for use in the District of Columbia Prepared Review: Question #2 QUESTION: A person has found out she is eligible for a $100 premium tax credit. Will she pay more in premiums for a gold plan or a silver plan offered by the same company? Prepared by Families USA for use in the District of Columbia Answer: Question #2 ANSWER: The gold plan The gold plan will cost the person more in premiums because it is a more expensive plan. The government pays the same premium tax credit no matter which plan the person picks. Prepared by Families USA for use in the District of Columbia DC Coverage Assistance Options in 2014 Approximate Income Levels as a Percent of Poverty Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions: The Basics People with incomes below 250% of poverty will get extra help paying for medical services in certain plans • This will reduce the maximum amount that a sick person would pay out of pocket • It could reduce the deductible, co-insurance, or copayments in a silver plan, making it more like a gold or platinum plan Prepared by Families USA for use in the District of Columbia What is cost-sharing? Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions (Individual) Income as % of Poverty Level (Shown for a Family of One) Out-of-Pocket Maximum Cost-Sharing for an Individual (Double for a Family) Co-Pays/ Co-Insurance/ Deductibles Are Similar to This Metal Level Plan 100-150% $2,250 Platinum 150-200% $2,250 Gold 200-250% $5,200 Silver In DC, most people in these income brackets will be getting Medicaid. A small population may be in private DC Health Link plans with cost-sharing reductions. Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions: Question #1 Maria is very sick, and she is not eligible for Medicaid because she is under a five-year bar. Maria’s income is about 180% of poverty. She pays all of her medical expenses until she reaches her plan’s deductible, and then she pays copayments for drugs and doctors. QUESTION: At what point will her plan stop charging her copayments? Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions: Answer #1 ANSWER: When her medical out-of-pocket medical expenses for the year reach $2,250, excluding premiums Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions: Question #2 QUESTION: Richard does not qualify for Medicaid because his income is 220% of poverty. At what point will his plan stop charging copayments? Prepared by Families USA for use in the District of Columbia Cost-Sharing Reductions: Answer #2 ANSWER: When his out-of-pocket medical expenses for the year reach $5,200 Prepared by Families USA for use in the District of Columbia Things to Remember • You will play an important role in helping people apply for help with their coverage • The new system will do much of the work for you • This training is designed to help you understand why the new system works the way it does • You will be able to refer applicants to additional sources of help Prepared by Families USA for use in the District of Columbia Applications Prepared by Families USA for use in the District of Columbia What’s changing? • New application for MAGI-based Medicaid and premium tax credits • Many ways to apply • Easier eligibility determination Prepared by Families USA for use in the District of Columbia New Applications • Two online applications: • Full application for financial assistance • • MAGI Medicaid Premium tax credits and cost-sharing reductions • Shortened application to buy a full-cost DC Health Link plan • You can help encourage people to fill out the full application, since new help is available Prepared by Families USA for use in the District of Columbia Which groups use other applications? • Medicare assistance programs (SLMB, QMB, Low-Income Subsidy) • “Non-MAGI” Medicaid for elderly, blind, disabled, people who need long-term care, medically needy • DC Alliance • Other benefits, such as SNAP and TANF Prepared by Families USA for use in the District of Columbia Ways to Apply • • • • Online By phone In person By mail In-person interviews are not required! Prepared by Families USA for use in the District of Columbia The Advantages of Using the Online Application • Application is easy to read • Help by phone available 24/7 • Some information will be pre-populated • Allows for real-time verification • Application is dynamic • Applicant gets information on whether or not eligibility has been determined at the end Prepared by Families USA for use in the District of Columbia People Will Still Want In-Person Help • Trusted government agencies • In-Person Assisters (IPAs)/Navigators (new) • Other groups, like community clinics and hospitals Prepared by Families USA for use in the District of Columbia In-Person Assisters • Funded by DC Health Benefit Authority • Conduct outreach and education in the community • Trained to help with application and plan selection • Provide help in other languages and assistance for people with disabilities • Give impartial information Prepared by Families USA for use in the District of Columbia Certified Application Counselors • Another type of assister trained to help with application and plan selection • May be staff in community health clinics, hospitals, schools, or other community organizations • Registered with DC Health Link, but not funded • Focused on helping people who come through their doors, rather than conducting active outreach Prepared by Families USA for use in the District of Columbia Accessibility • Applications and forms must be accessible for people with limited English proficiency and people with disabilities • Application will be available in English, Spanish, and, later in 2014, Amharic Prepared by Families USA for use in the District of Columbia What does the application ask about? • Household • Income • Citizenship and immigration status • Residency • Pregnancy • Other coverage Prepared by Families USA for use in the District of Columbia Applicants and Non-Applicants • Some household members may be non-applicants • Important to list all household members to get full benefits • For instance, a large household with income of $45,000 may be entitled to more benefits than a smaller household with the same income • People DO NOT have to list Social Security numbers or immigration status for non-applicants Prepared by Families USA for use in the District of Columbia Example: Tania Tania is applying for health coverage. She and her husband have children. Her husband does not want health coverage, but he agrees that the rest of the family should apply. What can you tell Tania? Prepared by Families USA for use in the District of Columbia Answer: What to Tell Tania ANSWER: Tania can list her husband as a non-applicant and does not need to provide his Social Security number. The computer may not be able to electronically verify household income without the Social Security number, but she can provide paper documentation of her husband’s income. Prepared by Families USA for use in the District of Columbia Getting an Authorized Representative • Consumer can designate authorized representative (power of attorney, authorized representative form, etc.) • May also be assigned through a court order • Can be designated at any time: • Online through “My Account” • By mailing a request to a service center • In person at a service center • Can be changed at any time Prepared by Families USA for use in the District of Columbia What Authorized Representatives Will Do • Authorized representatives will receive: • Copies of notices sent to the consumer • Other communications on behalf of consumer • Authorized representatives will be able to: • File an application and renew coverage • Provide information and documentation • Explain rights and responsibilities • Provide representation in an interview or hearing Prepared by Families USA for use in the District of Columbia Verification • New system uses electronic data sources first • Will accept attestation for some things (for example, pregnancy and household composition) • Will need documentation of income, citizenship, and immigration status if no electronic data is available • Some differences between attestation and electronic data sources will need to be resolved and some will not • System will check electronic data sources for you and tell you when documentation is needed Prepared by Families USA for use in the District of Columbia Processing Applications • Outside time limits for processing Medicaid applications remain the same • • 45 days 90 days for people applying on basis of disability • Some eligibility determinations will happen right away • System will automatically send notices to: • • Applicant Applicant’s employer, if necessary Prepared by Families USA for use in the District of Columbia Open Enrollment • Time to enroll in DC Health Link plans that can be purchased with premium tax credits • First open enrollment season: October 1, 2013 to March 31, 2014 • Future years’ open enrollment seasons: October 15 to December 7 (enroll in 2014 for coverage to be effective Jan 1, 2015, for example) • People can still apply for and enroll in Medicaid at any time Prepared by Families USA for use in the District of Columbia What will happen to people in non-MAGI Medicaid? • Screening questions in application will identify people who might qualify • Because determinations (for example, disability) take longer, applicants can enroll in what their income qualifies them for while they wait Prepared by Families USA for use in the District of Columbia Review: Question #1 QUESTION: Which of the following groups will have their Medicaid eligibility determined through the new online application? • Pregnant women • Parents • Adults under age 65 without children • Adults over age 65 • People with disabilities Prepared by Families USA for use in the District of Columbia Answer: Question #1 ANSWER: • Pregnant women • Parents • Adults under age 65 without children Prepared by Families USA for use in the District of Columbia Review: Question #2 QUESTION: Starting in October, people will be able to apply in which of the following ways: a. By phone b. By mail c. In person d. Online e. All of the above Prepared by Families USA for use in the District of Columbia Answer: Question #2 ANSWER: E – All of the above People will be able to apply by phone, by mail, in person, and online. Prepared by Families USA for use in the District of Columbia Individual Responsibility Prepared by Families USA for use in the District of Columbia Why is this requirement part of the law? • To encourage people to get coverage now, rather than wait until they are sick • To keep insurance affordable Prepared by Families USA for use in the District of Columbia Individual Responsibility Starting in 2014, each individual, including children and seniors, must: 1. Have minimum essential coverage (which we’ll explain in a minute); OR 2. Qualify for an exemption; OR 3. Make a payment when filing his or her federal tax return. This payment is the “individual shared responsibility” payment. Prepared by Families USA for use in the District of Columbia What is “minimum essential coverage”? • A basic set of benefits and financial protections that a plan must have to be considered adequate health coverage • Most people in the U.S. already have minimum essential coverage through: • An employer (their own employer or employer of spouse or parent) • A government program, such as Medicaid, Medicare, or Tricare • Health insurance purchased by an individual or family Prepared by Families USA for use in the District of Columbia What is not minimum essential coverage? • A “limited benefit” plan that covers only a particular condition, such as a cancer-only policy • Self-funded student plans are minimum essential coverage • A medical discount plan • A plan that pays a fixed amount per day (example: a policy that pays $250 for each day someone is sick, but nothing else) • DC Alliance Prepared by Families USA for use in the District of Columbia Exemptions from the Individual Responsibility Requirement • Some people are exempt from individual responsibility, but many will need to get a certificate from HHS showing that they are exempt • Others will claim their exemption when they file taxes • Exemptions are time-limited Prepared by Families USA for use in the District of Columbia Who is exempt from the individual responsibility requirement? 1. People with a coverage gap of less than three months 2. People with certified financial hardships 3. People with incomes below the minimum tax filing threshold 4. People whose premiums would be more than 8% of their income 5. Those who are incarcerated 6. Those who are not lawfully present in the United States 7. Religious sects opposed to accepting insurance benefits 8. Members of recognized health care sharing ministry 9. Federally recognized Indian Tribes Prepared by Families USA for use in the District of Columbia Penalties for Going without Coverage (If Not Exempt) In 2014: • $95/adult, $47.50/child • Up to $285 per family or 1% of family income, whichever is greater In 2016: • $2,085/family or 2.5% of family income Prepared by Families USA for use in the District of Columbia Handling Questions about Individual Responsibility Refer to consumers to the HHS call center if they have questions about the individual responsibility requirement. Prepared by Families USA for use in the District of Columbia Milestone Dates for DC Health Link • Enrollment starts October 1, 2013 • Coverage begins as early as January 2014 Prepared by Families USA for use in the District of Columbia