presentation - Canadian Public Health Association
advertisement

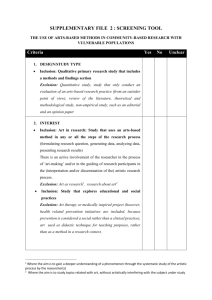
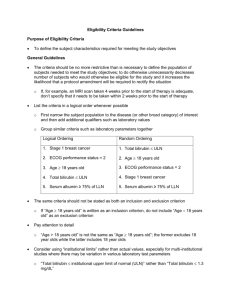
Addressing individual income as a social determinant of health in clinical settings: A realist systematic review CPHA May 28, 2014 Danyaal Raza1, Andrew D. Pinto2,3 1. Harvard School of Public Health, Harvard University 2. Department of Family and Community Medicine, St. Michael’s Hospital 3. Centre for Research on Inner City Health, St. Michael’s Hospital No specific financial conflict of interest. My research is funded by CIHR and the Ontario Ministry of Health and Long-Term Care. The premise of this discussion is working towards social justice and hence, a more healthy society. This is my objective as a physician, activist and public scholar. I bring a privileged world-view and set of experiences to this work. I do not bring the lived experience of being a member of a marginalized population. ROLE OF PRIMARY HEALTH CARE IN ADDRESSING HEALTH INEQUITY Social Determinants of Health • #SDOH • “the conditions in which people are born, grow, live, work and age. These circumstances are shaped by the distribution of money, power and resources at global, national and local levels” http://www.who.int/social_determinants/en/ Canadian Medical Association, 2013 http://healthcaretransformation.ca/infographic-social-determinants-of-health/ WHO 2008. Final Report of the Commission on the Social Determinants of Health. p.43. How do SDOH “get under our skin”? How do they work? WHO. World Health Report 2008. p. 43 http://www.who.int/whr/2008/08_chap3_en.pdf Opportunity for change as we move toward “people-centred” model WHO. World Health Report 2008. p. 43 http://www.who.int/whr/2008/08_chap3_en.pdf Features of PHC that are key to addressing health equity • • • • • • • First contact Accessible Longitudinal Person-focused Coordination and navigation Comprehensive BOTH preventive (future needs) and curative (immediate needs) • Existing and potential connections to other systems • Political/media focus • Highly resources Adapted from De Maeseneer et al. WHO 2007. http://www.who.int/social_determinants/resources/csdh_media/primary_health_care_2007_en.pdf St. Michael’s Hospital • Established a SDOH Committee within the DFCM • Ongoing projects: – Socio-demographic data collection – Income security health promotion – Medical-legal partnership – Childhood literacy (future) EVIDENCE: SYSTEMATIC REVIEW AND REALIST SYNTHESIS Search Strategy • Published in English • Search terms used included “income intervention”, “poverty intervention*,” “welfare advice,” “income supplement,” “social assistance,” “disability benefit,” “citizen* advice,” “counsel*” and “outreach” • With the assistance of an information specialist, nine databases were chosen: Applied Social Sciences Index and Abstracts, CINAHL, FRANCIS, International Bibliography of the Social Sciences, MEDLINE, PAIS International • January 1, 1990 to June 13, 2013 Inclusion/Exclusion Inclusion/Exclusion Potentially relevant articles identifies though electronic databases search 968 articles Independent title & abstract review with inclusion/exclusion criteria applied 933 articles excluded 35 articles included Independent full text review with inclusion/exclusion criteria applied 4 articles excluded 29 articles included Key Findings • Vast majority of studies from the UK (27 of 29) • Most focused on implementation of “Citizen Advice Bureau” workers within GP practices • Almost all interventions were focused on improving access to state benefits • Range of sample sizes (n=62-2484), but most around 200-300 • Vast majority were observational studies; one RCT (Mackintosh. BMC Public Health 2006) • Most reported income change outcomes, and very few reported health outcomes Key Findings • On average, approximately 25% of participants had an increase in benefits, typically on the order of £100-200/month • Most studies followed participants for 12 months • Typically took 3-6 months for benefit change to be implemented • Health outcomes focused on QOL measures. Found little difference before/after or between those who received benefits and those who did not. Key Findings • Interviews with those who received benefits: – Improved mental health – Less stress around bills, rent – Able to afford better food – Able to participate in social life Health care team universally supportive of benefits advice. Seen as saving money and time, and improving care for patients. Practical Tips • Requires support from health care team and significant education of providers • Many patients did not initially understand why referred to benefits advisor • Small % of participants were very complex and required a great deal of support and follow-up • Main groups that benefited were: – Elderly, particularly home-bound – New immigrants – People with mental illness Enabling characteristics Underlying mechanisms of income security intervention Context [economic, political, historical] Context [family, community, society] Health care setting Patient identification: in clinical encounter OR survey OR chart audit Patient Income Security Intervention Increase Income Benefits/ grants Engage other advocates Information & advice Admin support/as sist with forms Direct advocacy for patient Increase investm ents Reduce expenses Employ ment Cheaper housing Help job search & apply Improve financial literacy Support action to improve wages Retraining/Edu cation/Rehab Reduce other expenses Obtain free goods/s ervices Work accommodatio n for disability Improved Income Security Reduce debt & restructure debt Increase savings Set up bank account Budgeting Change spending habits Post-synthesis framework Context [family, community, society] Context [economic, political, historical] Patient Health care setting Patient identification: in clinical encounter OR survey OR chart audit Mechanisms Enabling Characteristics Patient Health Promoter Colocation Accessible Decreased stigma Health Setting Embedment Income Security Intervention Provider Benefits counsellorhealth care team relationship Trust Improved Income Security Pro-active advice High Impact Expert benefits advice Patienthealth provider relationship Income Security Health Promotion Interventions: 1. Increasing income • • • • Benefits/grants Taxes Employment Retraining 2. Reducing expenses 3. Improving financial literacy Phase I: Multi-institutional support Phase II: Data and triangulation Phase III: Meeting individual needs Phase IV: Community collaboration Phase V: Community leadership Thank You andrew.pinto@utoronto.ca @AndrewDPinto