Laurel Lee, VP of Member and Community
advertisement

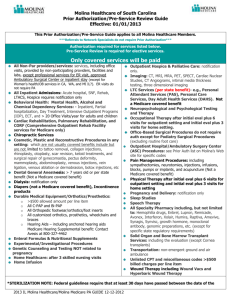
Innovative Funding Streams Driving Health Laurel Lee - Vice President, Member & Community Engagement State of Reform January 8, 2015 Agenda • Who is Molina – a brief overview • How Molina is Partnering to improve Health and further the Triple Aim • • • • • • Patient Engagement Aligned incentives (Risk Sharing not Risk Shedding) Delivering Community Based Care Coordination Transparent Data Sharing Innovation in Service delivery Behavioral Health Integration - “Whole Person” care Who is Molina Healthcare? From a single clinic in Long Beach, CA… “I hope that no one ever forgets that it all began with a single clinic.” C. David Molina, MD, MPH, Founder Confidential & Proprietary Who is Molina Healthcare? 4 …To a multi-state Health Company State Health Plans • California • Florida • Illinois • Michigan • New Mexico • Ohio • South Carolina • Texas • Utah • Washington • Wisconsin Clinics - Care Delivery MMIS – Molina Medicaid Solutions – Managed Medicaid Information System Our Markets (3Q 2014) Who is Molina Healthcare? 5 …The largest Medicaid Health Plan in Washington 2015 Medicaid Service Area - Washington 473,000 Members* *(3Q 2014) Partnering to Improve Health - Patient Engagement • Member Rewards/Incentives for Healthy behaviors • Case Management & Disease Management • Community Outreach During the first three quarters of 2014 Molina created or participated in more than 750 member facing events. 6 Partnering to Improve Health – Aligned Incentives Accountable Care Continuum Programs that meet providers where they are… • Providers as Partners • Risk Sharing; Not Risk Shedding • Focused Outcomes: Triple Aim Pay-forPerformance Bonus 7 Primary Care Capitation “ACE” Accountable Care Entity Cost & Quality Program Total Cost of Care Capitation Partnering to Improve Health – Care Coordination Molina’s Community Connector Program • Community Health Worker model launched in 2012 • Face to Face, community based care coordination and connections to community resources, health providers, and clinical teams. • Molina Staff or Strategic partnerships with Community Based Care Coordination 8 Partnering to Improve Health – Data Transparency Care Management – Near “real time” Emergency and Hospital Admission data sharing with Providers & Community Based Care Coordinators Cost & Utilization Management – Data and analytics to help drive Right Care, In The Right Place, At The Right Time, In The Right Way 9 Partnering to Improve Health – Innovation in Service Delivery Telemedicine – Partnering with an Integrated Delivery System to offer Virtual urgent care telemedicine visits with an MD – Go live, Q1 2015 – Exploring Telepsychiatry – increasing access to appropriate high quality mental health care through direct delivery of care (Telepsych) and through consultation with PCPs to enhance community based management of psychotropic medications. Expanding Access; Changing the Models of Care 10 Partnering to Improve Health – Whole Person Care Behavioral Health Integration Partnerships: • RSN Data Sharing – 2-way Data Share with King County RSN Go Live Jan 2015 • Care Coordination Collaboration Pilots – Partnering with IDS and another MCO to jointly fund a licensed clinical social worker at a high volume Primary Care Clinic – Co-locating Molina Community Connector and case management staff at high volume Primary Care Clinics Better understanding the Social Determinants of Health 11 Molina Healthcare Service Delivery Innovation Delivering Community Based Care Coordination Transparent Data Sharing Aligned incentives Patient Engagement 12 Behavioral Health Integration