Why the notion of ‘responsibility for
one's health' fails to direct priority
setting in Swedish health care
Paper to be presented at the Conference
"Priorities 2010. Priority Setting in Difficult Economic Times"
Boston, MA, 24 April 2010
Dr. Werner Schirmer
Department of Sociology
Uppsala University
Prof. Dimitris Michailakis
Department of Social Work and Psychology
Faculty of Health and Working Life
University of Gävle/Sweden
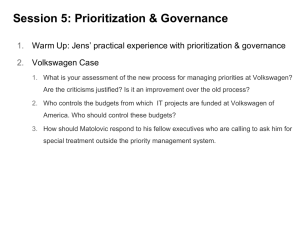
1 Introduction
Ethical Platform: Three Principles for priority-setting as
proposed in 1995
the human dignity principle
the principle of medical need and solidarity
the principle of cost-effectiveness
Evaluations from 2007 showed that these principles failed
they could neither provide guidance to physicians
nor did they contribute to save significant amounts of money
One potential solution suggested:
the notion of responsibility for one's health as a principle for
prioritization
1 Introduction
The aim of this paper:
Scrutinizing the responsibility principle
Theoretical framework:
Theory of society by German sociologist Niklas
Luhmann
2 Legitimacy
If it was for effectiveness only, ascriptive
social attributes (sex, age, class, ethnicity
etc.) would be a suitable ordering principle for
prioritization
However, modern society considers them as
illegitimate
Acceptable candidates for prioritization
criteria must comply with modern values such
as equality and human dignity
2 Legitimacy
3 Prioritization paradox?
The Ethical Platform considers the human
dignity principle as unconditional and
therefore superior other priority principles
This approach seems to be based on a logical
contradiction: unconditional equal value of
human beings contradicts the very idea of
prioritization
Setting priorities means selecting someone
instead of someone else, thus it means
treating supposedly equals as unequals
3 Prioritization paradox?
Prioritization criteria have to derive their
legitimacy in line with the human dignity
principle while factually running counter to
the idea of equal human value
These criteria have to compete with human
dignity – not in terms of legitimacy but of
practicality
What we, then, are looking for are reasonable
exemptions from the human dignity principle
3 Prioritization paradox?
4 Finding reasonable exemptions from
the human dignity principle
The criteria proposed in the Swedish debate on
prioritization can be sorted into two major groups
depending on whether their focus is on
ill/injured human bodies/minds needing treatment
or on a collectivity that has to pay or dispense
In other words, it is either medical rationality or
welfare-political rationality that sets the frame for
priority principles
5 Cause of the problems from 1995
Both the observational perspectives and the reference-
problems of medicine and politics are incompatible
Medicine
The reference is the (ill/injured) human body/mind
Medical communication centres on diseases, organisms,
treatments and healing
Politics
the reference is a collective (e.g. a national population)
Political communication centres on binding decisions and power
It depends on legitimacy and collective support
Therefore, the state is keen on satisfying moral needs such as
equality, solidarity, fair allocation of taxes, and provision of
services (security, education, infrastructure, or healthcare)
5 Cause of the problems from 1995
Since modern society lacks an "Archimedean"
standpoint that can objectively determine
what is more important and what is less,
medical needs are not per se more important
than solidarity and vice versa
Medical and welfare-political criteria cannot
outrank each other
Each can be legitimately rejected on the
grounds of the other
5 Cause of the problems from 1995
6 Solution?
The responsibility principle
A report by The Swedish National Centre for
Priority Setting from 2007 suggested
reactivating the "responsibility principle"
According to this principle, patients are held
responsible for their illness if they conduct an
unhealthy lifestyle (e.g. wrong diet, physical
inactivity, abuse of narcotics) and those who
fail to live up to these expectations can
legitimately be down-prioritized
Unhealthy Lifestyle
points out a scientifically established causal
relation of people's lifestyle and their health
condition
Can be treated as an objective fact and allows
hypothesis-like statements such as "physical
inactivity makes cancer likely"
Responsibility for one's health
Responsibility presupposes the attribution of
agency: has the patient a choice to act
differently, and can thereby be held
responsible, or is she just a victim of
circumstances beyond her control, and
thereby seen non-responsible?
For instance expressed by the statement
"being not physically active, it is your fault if
you become ill with cancer"
Scrutinizing the responsibility principle
The responsibility principle pretends to be a
medical selection but it is a political one
In a medical context, individuals are relevant
as bodies/minds but not as agents
The medical system can establish facts, but is
has no conception of responsibility
The moment of choice that enables the
attribution of responsibility in the causal
relation (lifestyle health outcome) is added
by the political system
Conclusion
The deadlock from 1995 cannot be overcome simply
by introducing a principle based on individual
responsibility for one's health
The connection of responsibility and lifestyle falsely
assumes a subordination of medicine under politics
Responsibility is a political notion building on the
contingent attribution of agency due to current
political interests, there is no corresponding concept
in medicine
(Un)healthy lifestyle assumes causal reasoning
about objectively measureable facts and cannot be
usurped by political logics
Viable solutions have to take seriously that medicine
and politics are each autonomous spheres with
incompatible rationalities