In the name of god
advertisement

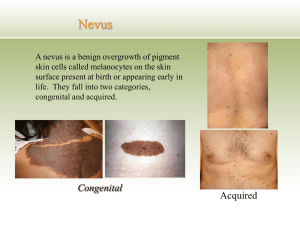
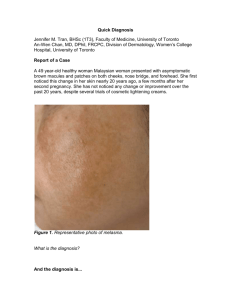
Dr Anahita Vali Dermatologist & venereologist Melasma, sometimes called chloasma (which means green skin), appears as a symmetrical blotchy, brownish pigmentation on the face. The pigmentation is due to overproduction of melanin by the pigment cells, melanocytes. It can lead to considerable embarrassment and distress. Melasma is a very common patchy brown, tan, or blue-gray facial skin discoloration, almost entirely seen in women in the reproductive years. It typically appears on the upper cheeks, upper lip, forehead, and chin of women 20-50 years of age. Although possible, it is uncommon in males. Over 90% of those with melasma are women. primarily related to external sun exposure, external hormones like birth control pills, and internal hormonal changes as seen in pregnancy. Most people with melasma have a history of daily or intermittent sun exposure, although heat is also suspected to be an underlying factor. Melasma is most common among pregnant women, especially those of Latin and Asian descents. People with olive or darker skin, like Hispanic, Asian, and Middle Eastern individuals, have higher incidences of melasma. Melasma is most common in women 20-50 years of age. Melasma looks like brown, tan, or blue-gray spots on the face (hyperpigmentation). Melasma is characterized by three location patterns (central face, cheekbone, and jawline). Melasma is caused partly by sun, genetic predisposition, and hormonal changes. The most common treatment is topical creams containing hydroquinone. Melasma prevention requires sun avoidance and sun protection with hats and sunscreen. An estimated 6 million women are living in the U.S. with melasma and 45-50 million women worldwide live with melasma. Prevention is primarily aimed at facial sun protection and sun avoidance. Treatment requires regular sunscreen application, medications such as 4% hydroquinone and fading creams. unknown. The exact cause of melasma remains triggered by several factors, including pregnancy, birth control pills, hormone replacement therapy (HRT and progesterone), family history of melasma, race, antiseizure medications, and other medications that make the skin more prone to pigmentation after exposure to ultraviolet (UV) light. Uncontrolled sunlight exposure is considered the leading cause of melasma, especially in individuals with a genetic predisposition. individuals typically develop melasma in the summer months,. In the winter, the hyperpigmentation in melasma tends to be less visible. Heat, such as that experienced in a bakery or factory. When melasma occurs during pregnancy, it is also called chloasma, or "the mask of pregnancy." Pregnant women experience increased estrogen, progesterone, and melanocyte-stimulating hormone (MSH) levels during the second and third trimesters of pregnancy. Melanocytes are the cells in the skin that deposit pigment. However, it is thought that pregnancy-related melasma is caused by the presence of increased levels of progesterone and not due to estrogen and MSH. postmenopausal women who receive progesterone hormone replacement therapy are more likely to develop melasma. Postmenopausal women receiving estrogen alone seem less likely to develop melasma. products or treatments that irritate the skin may cause an increase in melanin production and accelerate melasma symptoms. People with a genetic predisposition or known family history of melasma are at an increased risk of developing melasma. Important prevention methods for these individuals include sun avoidance and application of extra sunblock to avoid stimulating pigment production.. Four types of pigmentation patterns are diagnosed in melasma: epidermal, dermal, mixed, and an unnamed type found in dark-complexioned individuals. The epidermal type is identified by the presence of excess melanin in the superficial layers of skin. Dermal melasma is distinguished by the presence of melanophages (cells that ingest melanin) throughout the dermis. The mixed type includes both the epidermal and dermal type. In the fourth type, excess melanocytes are present in the skin of dark-skinned individuals. Occasionally, skin biopsy may be performed to confirm the diagnosis. Histology varies with the type of melasma. But some degree of each of the following features is usually found. Melanin deposited in basal Highly dendritic (branched) and suprabasal keratinocytes deeply pigmented melanocytes Melanin in the dermis within melanophages Solar elastosis and elastic fibre fragmentation The extent and severity of melasma can be described using the Melasma Area and Severity Index (MASI). Melasma is usually readily diagnosed by recognizing the typical appearance of brown skin patches on the face. Dermatologists are physicians who specialize in skin disorders and often diagnose melasma by visually examining the skin. A black light or Wood's light (340-400 nm) can assist in diagnosing melasma, although is not essential for diagnosis. In most cases, mixed melasma is diagnosed, which means the discoloration is due to pigment in the dermis and epidermis. Rarely, a skin biopsy may be necessary to help exclude other causes of this local skin hyperpigmentation Melasma is characterized by discoloration or hyperpigmentation primarily on the face. Three types of common facial patterns have been identified in melasma, including centrofacial (center of the face), malar (cheekbones), and mandibular (jawbone). The centrofacial pattern is the most prevalent form of melasma and includes the forehead, cheeks, upper lip, nose, and chin. The malar pattern includes the upper cheeks. The mandibular pattern is specific to the jaw. The upper sides of the neck may less commonly be involved in melasma. Rarely, melasma may occur on other body parts like the forearms. One study confirmed the occurrence of melasma on the forearms of people being given progesterone. This was a unique pattern seen in a Native American study. Type of melasma Clinical features Epidermal Well-defined border Dark brown colour Appears more obvious under black light Responds well to treatment Dermal The most common type Ill-defined border Light brown or bluish in colour Unchanged under black light Responds poorly to treatment Mixed Combination of bluish, light and dark brown patches Mixed pattern seen under black light Partial improvement with treatment Postinflammatory pigmentation Solar lentigines and other forms of lentigo Drug-induced pigmentation, e.g. due to minocycline Lichen planus Naevus of Ota. Scented or deodorant soaps, toiletries and cosmetics may cause a phototoxic reaction triggering melasma that may then persist long-term. A phototoxic reaction to certain medications may also trigger melasma. Melasma has been associated with hypothyroidism (low levels of thyroid hormone). Scented or deodorant soaps, toiletries and cosmetics may cause a phototoxic reaction triggering melasma that may then persist long-term. The most common melasma therapies include 2% hydroquinone (HQ) creams like the over-thecounter products Esoterica and Porcelana and prescription-strength 4% creams like Obagi Clear, TriLuma, NeoCutis Blanche, and 4% hydroquinone. Certain sunscreens also contain 4% hydroquinone, such as Glytone Clarifying Skin Bleaching Sunvanish SPF 23 and Obagi's Sunfader sunscreen. Products with HQ concentrations above 2% sometimes require a prescription or are dispensed through physician's practices. Clinical studies show that creams containing 2% HQ can be effective in lightening the skin and are less irritating than higher concentrations of HQ for melasma. These creams are usually applied to the brown patches twice a day. Sunscreen should be applied over the hydroquinone cream every morning. There are treatments for all types of melasma, but the epidermal type responds better to treatment than the others because the pigment is closer to the skin Hydroquinone is the compound most frequently used in skin whitening products. Due to concerns about its side effects, it was almost banned by the FDA in 2006, as there were medical issues of carcinogenicity and reports of disfiguring ochronosis. In the European Union Hydroquinone has been banned in cosmetic creams since 2000. Symptoms include: yellow-brown, banana-shaped fibers caviar-like papules brown-grey or blueblack hyperpigmentation The majority of the lesions will be seen on areas of the body that get the most sun. Long term use of creams containing this compound may lead to exogenous ochronotic lesions. The duration of the use is directly proportional to the risk of developing the condition with most cases being after years of use. Around 10-15 million skin lightening products are sold annually, with Japan being the major buyer Exogenous ochronosis can be caused from long term usage of certain ‘’skin lightening products’’, even if the hydroquinone is in amounts as small as 2%. Skin lightening products are still prevalent in many parts of the world.Reasons for this may be due to aesthetic or social standing reasons, in areas where a lighter skin tone is considered to be a sign of wealth or beauty.As well, skinlightening creams containing compounds such as hydroquinone are commonly used to help with hyperpigmentation disorders such as melasma Hydroquinone-induced exogenous ochronosis is an avoidable dermatosis that is exceedingly difficult to treat. However, some studies show that treatment may be possible with a Q- switched alexandrite (755 nm) laser. It is recommended that individuals with this disorder stop using hydroquinone containing compounds.It is important to be aware of this as dermatologists may think the symptoms a patient is exhibiting are a melasma, and prescribe a hydroquinone containing cream. Ochronosis is the syndrome caused by the accumulation of homogentisic acid in connective tissues. The phenomenon was first described by Rudolf Virchow in 1865.The condition was named after the yellowish (ocher-like) discoloration of the tissue seen on microscopic examination. However, macroscopically the affected tissues appear bluish grey because of a light scattering phenomenon known as the Tyndall effect. The condition is most often associated with alkaptonuria but can occur from exogenous administration of phenol complexes like hydroquinone. THERE ARE THREE CLINICAL STAGES OF EXOGENOUS OCHRONOSIS: ERYTHEMA AND MILD HYPERPIGMENTATION HYPERGIMENTATION AND ‘’CAVIAR-LIKE’’ LESIONS PAPULO-NODULAR LESIONS temporary skin irritation. People who use HQ treatment in very high concentrations for prolonged periods (usually several months to years) are at risk of developing a side effect called ochronosis. Hydroquinone-induced ochronosis is a permanent skin discoloration that is thought to result from use of hydroquinone concentrations above 4%. Although ochronosis is fairly uncommon in the U.S., it is more common in areas like Africa where hydroquinone concentrations upward of 10%-20% may be used to treat skin discoloration like melasma. Regardless of the potential side effects, HQ remains the most widely used and successful fading cream for treating melasma worldwide. HQ should be discontinued at the first signs of ochronosis Melasma can be very slow to respond to treatment, so patience is necessary. Start gently, especially if you have sensitive skin. Harsh treatments may result in an irritant contact dermatitis, and this can result in postinflammatory pigmentation. Generally a combination of the following measures is helpful. General measures Discontinue hormonal contraception. Year-round sun protection. Use broad-spectrum very high protection factor sunscreen of reflectant type and apply it to the whole face every day. Reapply every 2 hours if outdoors during the summer months. Alternatively or as well, use a make-up that contains sunscreen. Wear a broad-brimmed hat. Use a mild cleanser, and if the skin is dry, a light moisturiser. This may not be suitable for those with acne. Cosmetic camouflage (make-up) is invaluable to disguise the pigment. Tyrosinase inhibitors are the mainstay of treatment. The aim is to prevent new pigment formation by inhibiting formation of melanin by the melanocytes. Hydroquinone 2-4% as cream or lotion, applied accurately to pigmented areas at night for 2 to 4 months. This may cause contact dermatitis (stinging and redness in 25%). It should not be used in higher concentration or for prolonged courses as it has been associated with ochronosis (a bluish grey discolouration). Azelaic acid cream, lotion or gel can be used longterm, and is safe even in pregnancy. This may also sting. Kojic acid is often included in formulations as they interact with copper, required by LDOPA (a cofactor of tyrosinase). Kojic acid can cause irritant contact dermatitis and less commonly, allergic contact dermatitis. Ascorbic acid (vitamin C) acts through copper to inhibit pigment production. It is well tolerated but highly unstable, so is usually combined with other agents. New agents under investigation include mequinol, arbutin and deoxyarbutin (from berries), licorice extract, rucinol, resveratrol, 4-hydroxy-anisole, 2,5-dimethyl-4-hydroxy3(2H)-furanone and/or N-acetyl glucosamine Topical corticosteroids such as hydrocortisone, work quickly to fade the colour and reduce the likelihood of a contact dermatitis caused by other agents. Soybean extract, which is thought to reduce the transfer of pigment from melanocytes to skin cells (keratinocytes) and inhibit receptors. Tranexamic acid is a lysine analogue that inhibits plasmin (this drug is usually used to stop bleeding) and reduces production of prostaglandins (the precursors of tyrosine). Tranexamic acid has been used experimentally for melasma as a cream or injected into the skin (mesotherapy), showing some benefit. It may cause allergy or irritation. Superficial or epidermal pigment can be peeled off. Peeling can also allow tyrosinase inhibitors to penetrate more effectively. Agents to achieve this include: Topical alpha hydroxyacids including glycolic acid and lactic acid, as creams or as repeated superficial chemical peels, not only remove the surface skin but their low pH inhibits the activity of tyrosinase. Topical retinoids, such as tretinoin are prescription medicines. They can be hard to tolerate and sometimes cause contact dermatitis. Do not use during pregnancy. Salicylic acid , a common peeling ingredient in skin creams and can also be used for chemical peels but it is not very effective in melasma. Currently, the most successful formulation has been a combination of hydroquinone, tretinoin, and moderate potency topical steroid, which has been found to result in improvement or clearance in up to 60-80% of those treated. Many other combinations of topical agents are in common use, as they are more effective than any one alone. However, these products are often expensive. In order to treat melasma, combination or specially formulated creams with hydroquinone, a phenolic hypopigmenting agent, azelaic acid, and retinoic acid (tretinoin), nonphenolic bleaching agents, and/or kojic acid may be prescribed. For severe cases of melasma, creams with a higher concentration of HQ or combining HQ with other ingredients such as tretinoin, corticosteroids, or glycolic acid may be effective in lightening the skin. Azelaic acid 15%-20% (Azelex, Finacea) Retinoic acid 0.025%-0.1% (tretinoin) Tazarotene 0.5%-0.1% (Tazorac cream or gel) Adapalene 0.1%-0.3% (Differin gel) Kojic acid Lactic acid lotions 12% (Lac-Hydrin or Am-Lactin) Glycolic acid 10%-20% creams (Citrix cream, NeoStrata) Glycolic acid peels 10%-70% Other proprietary ingredients and mixtures of ingredients as in Elure, Lumixyl, and SkinMedica's Lytera products 1) Light, circadian rhythms and melatonin: (1) UV or visible light from the sun is sensed by the retina, which signals the suprachiasmatic nucleus (SCN) region of the brain, enabling entrainment of circadian rhythms throughout the body; (2) UV light induces skin damage. Both melatonin and Vitamin D3 have protective effects against this damage, through the inhibition of reactive oxygen species (ROS) formation as well as other mechanisms; (3) UVB light exposure can cause disruption of the circadian rhythms in normal skin, but also has the protective effect of producing Vitamin D3; and (4) in addition to its protective effects against UVB skin damage, melatonin also plays a role in the regulation of circadian rhythms, through its inhibition of the HDAC SIRT1 Although UV exposure is detrimental to skin health and key to the carcinogenesis process, it does not explain all skin cancers, including the increase in melanoma incidences of indoor workers. There has been speculation to tie this in with vitamin D production and/or the breakdown of vitamin D stores within the skin which is more common in indoor workers. With all the lifestyle changes we have seen over the past century, there has also been an increase in the incidences of many cancers. Many variables could contribute to the causes of these increases. However, the role that changes in environmental stressors play cannot be ignored. Further understanding of circadian regulations is needed to develop novel strategies towards circadian related conditions and diseases which encompass a wide range from behavioral conditions Melatonin was first discovered in connection to the mechanism by which some amphibians and reptiles change the color of their skin. discovered that feeding extract of the pineal glands of cows lightened tadpole skin by contracting the dark epidermal melanophores. dermatology professor Aaron B. Lerner and colleagues at Yale University, in the hope that a substance from the pineal might be useful in treating skin diseases, isolated the hormone from bovine pineal gland extracts and named it melatonin. production of melatonin exhibits a circadian rhythm in human pineal glands. The discovery that melatonin is an antioxidant was made in 1993.The first patent for its use as a low dose sleep aid was granted to Richard Wurtman at MIT in 1995. Around the same time, the hormone got a lot of press as a possible treatment for many illnesses.The New England Journal of Medicine editorialized in 2000: "The hype and the claims of the so-called miraculous powers of melatonin several years ago did a great disservice to a scientific field of real importance to human health. With these recent careful and precise observations in blind persons, the true potential of melatonin is becoming evident, and the importance of the timing of treatment is becoming clear. Our 24hour society, with its chaotic time cues and lack of natural light, may yet reap substantial benefits." Many biological effects of melatonin are produced through activation of melatonin receptors, while others are due to its role as a pervasive and powerful antioxidant, with a particular role in the protection of nuclear and mitochondrial DNA. Melatonin is categorized by the US Food and Drug Administration (FDA) as a dietary supplement and is not regulated as a pharmaceutical drug. In mammals, melatonin is biosynthesized in four enzymatic steps from the essential dietary amino acid tryptophan, with serotonin produced at the third step. Melatonin is secreted into the blood by the pineal gland in the brain. Known as the "hormone of darkness," it is secreted in darkness in both day-active (diurnal) and nightactive (nocturnal) animals. It may also be produced by a variety of peripheral cells such as bone marrow cellslymphocytes, and epithelial cells. Usually, the melatonin concentration in these cells is much higher than that found in the blood, but it does not seem to be regulated by the photoperiod. Melatonin has been identified in many plants including feverfew (Tanacetum parthenium), St John's wort (Hypericum perforatum), rice, corn, tomato and other edible fruits. The physiological roles of melatonin in plants involve regulation of their response to photoperiod, defense against harsh environments, and the function of an antioxidant. Melatonin also regulates plant growth by its ability to slow root formation, while promoting above ground growth. Melatonin has been reported in foodstuffs including cherries to about 0.17– 13.46 ng/g,bananas and grapes, rice and cereals, herbs, olive oil, wineand beer. When birds ingest melatonin-rich plant feed, such as rice, the melatonin binds to melatonin receptors in their brains. When humans consume foods rich in melatonin such as banana, pineapple and orange the blood levels of melatonin significantly increase. Pomegranate Fruit Extract Inhibits UVB-induced Inflammation and Proliferation by Modulating NFκB and MAPK Signaling Pathways in Mouse Skin Solar UV radiation, particularly its UVB component (280–320 nm), causes adverse cellular and molecular events leading to skin cancer. Therefore, additional approaches are needed to define novel agents to prevent skin cancer which results as a consequence of UVB exposure. In this study, we investigated the photochemopreventive effects of pomegranate fruit extract (PFE) after multiple UVB irradiations to the skin of SKH-1 hairless mice. Our data show that PFE consumption afforded protection to mouse skin by inhibiting UVB-induced inflammation and proliferation via modulation of nuclear factor kappa B and mitogen-activated protein kinases pathways. This study suggests the potential efficacy of PFE as a photochemopreventive agent for skin cancer Oral medications for melasma are under investigation, including tranexamic acid (a prescription medicine in New Zealand). None can be recommended at this time. Oral vit c,e antioidants Machines can be used to remove epidermal pigmentation but with caution – over-treatment may cause postinflammatory pigmentation. Fractional lasers are preferred and have been approved by the FDA for treating melasma. Patients should be pretreated with a tyrosinase inhibitor . The ideal treatment for a quick result is just to destroy the pigment, while leaving the cells alone. Intense pulsed light (IPL) appears to be the most effective light therapy investigated so far. The topicals described above should also be used before and after treatment. Pigmentation may recur. Several treatments may be necessary and postinflammatory hyperpigmentation may complicate recovery. Conventional carbon dioxide or erbium:YAG resurfacing lasers and pigment lasers (Q-switched ruby and Alexandrite devices) are sometimes used, but they have a high risk of making melasma worse. Dermabrasion and microdermabrasion are not recommended, as they may also cause postinflammatory hyperpigmentation. Intense pulse light IPL was developed in the late 1990s and involves the use of a xenon-chloride lamp that emits light that is non-coherent not collimated and has a wide spectrum (500– 1200 nm). The advantage of IPL lies in the flexibility of parameters. The wavelength, fluence, number, duration, and delay of pulses can be changed for each patient to effectively target chromophore. Hence, it can be used for the treatment of a variety of conditions like vascular lesions, hair removal, and melanocytic lesions. However, there are very few studies on the treatment of melasma with IPL. Rebound hyperpigmentation treated five Chinese patients with melasma with laser toning. There was no significant improvement in melasma and all five patients developed laser-induced depigmentation. Possible pathogenic mechanisms for this depigmentation could be high fluences causing direct phototoxicity and cellular destruction of melanocyte, subthreshold additive effect of multiple doses, intrinsic unevenness of skin pigmentation, and non-uniform laser energy output.Several other side effects mentioned in the literature include rebound hyperpigmentation, physical urticaria, acneiform eruption, petechiae, and herpes simplex reactivation. Rebound hyperpigmentation could be due to the multiple subthreshold exposures that can stimulate melanogenesis in some areas. Results take time and the above measures are rarely completely successful. About 30% of patients can achieve complete clearance with a prescription agent that contains a combination of hydroquinone, tretinoin and a topical corticosteroid. Unfortunately, even in those that get a good result from treatment, pigmentation may reappear on exposure to summer sun and/or because of hormonal factors. New topical and oral agents are being studied and offer hope for effective treatments in the future. Topical alpha hydroxyacids including glycolic acid and lactic acid, as creams or as repeated superficial chemical peels, not only remove the surface skin but their low pH inhibits the activity of tyrosinase. Tri-Luma is a combination prescription cream containing fluocinolone acetonide 0.01%, hydroquinone 4%, and tretinoin 0.05%. It is used to treat melasma and other skin discoloration. Results may be seen in usually about six to eight weeks from starting treatment. Tri-Luma should not be used for prolonged periods exceeding eight weeks without your doctor's recommendation. It should not be used by pregnant or breastfeeding women unless specifically instructed by your physicianit must also be refrigerated. Other combination creams include the Kligman formula which is a triple cream including a retinoid, a hydroquinone, and a topical steroid (for example, fluocinolone acetonide 0.01%, hydroquinone 8%, and tretinoin 0.1%). These triple combination creams may be compounded in different strengths by specialty pharmacists according to a physician's prescription. Triple creams are highly effective for melasma. It has been suggested that taking an oral proanthocyanidin (a class of flavonols) along with a vitamin regimen may significantly reduce pigmentation. At this time, the mechanism for this treatment method is not fully understood. Significantly more study is necessary before this method of treatment could be deemed effective. One major benefit to this mode, however, is that the use of proanthocyanidin is a natural treatment method, and it is a safe alternative in patients who exhibit a moderate or severe adverse reaction to a topical treatment.[25] In an attempt to search for a new treatment for melasma, Wu et al studied oral administration of tranexamic acid (TA) in Chinese patients. Tranexamic acid tablets were prescribed to 74 patients at a dosage of 250 mg twice daily for 6 months. At follow-up, more than half of patients (54%) showed good results. This treatment may be effective for some patients, but further study is needed.[26] Communication between the nervous system and epidermal melanocytes has been proven . The observation that epidermal melanocytes molecularly differ from dermal melanocytes seems to support the hypothesis about double origin of skin melanocytes Thus, melanocytes in the skin either derive directly from NCC populating the skin via a dorsolateral migratory pathway or arise from ventrally migrating precursors forming the myelin around the cutaneous nerves . Sometimes melasma may be preventable by avoiding facial sun exposure. In most cases, prevention is difficult. Individuals who have a family history of melasma must take extra precautions to prevent melasma. The most important way to prevent the onset of melasma and premature aging is to avoid the sun. If exposure to sunlight cannot be avoided, then hats, sunglasses, and sunblock with physical blockers should be worn. A daily sun protection factor (SPF) of at least 15 that contains physical blockers, such as zinc oxide and titanium dioxide, is recommended to block UV rays, but it is important to have a sunblock that also covers for UVA protection. Chemical blockers may not fully block both types of UVA and UV-B as effectively as zinc or titanium. The regular use of sun protection enhances the effectiveness of melasma treatments Although melasma tends to be a chronic disorder with periodic ups and downs, the prognosis for most cases is good. Just as melasma develops slowly, clearance also tends to be slow. The gradual disappearance of dark spots is based on establishing the right treatment combination for each individual skin type. Melasma cases that do not successfully respond to treatment are due to excessive sun exposure. After 30 years of age 10-20% of epidermal melanocytes are lost every decade . In the older people, apart from a decreased number of melanocytes morphology is changed (melanocytes are larger, more dendritic) and tyrosinase activity is reduced. The relationships between ageing and the proliferative activity of melanocytes have been observed. In vitro, adult melanocytes proliferate less times than fetal and neonatal melanocytes . Also, melanocytes from patients with a premature ageing disorder have reduced proliferative potential Melanoblasts migrate over very long distances throughout the embryo, proliferate and promote their own survival. Thus, melanoblast development is a highly dynamic process, which requires rapid activation of different signaling pathways. Recent developmental studies using model organisms and lineage tracing have been able to trace melanocytes arising from migration of a multipotent precursor cell along nerve projections. With great probability there could be cells with stem cell's properties located in the cutaneous nerves, but if only ? These cells are retained in a stem cell-like state until the signal sent by the end of the cutaneous nerve promotes these cells to differentiate into melanocytes . But there are also observations that some melanoblasts from the dorsal way of NCC migration stay in the dermis after the end of epidermis inoculation, up to the second trimester during fetal time a, Haematoxylin and eosin stain of normal human skin. Cells of the upper layer of the epidermis (keratinocytes) contain large nuclei, which stain blue, and the dermis appears pink as a result of staining of its abundant protein, collagen (muscle and nerve fibres may also stain pink). Normal melanocytes (arrows) have smaller nuclei and inconspicuous cytoplasm compared with the surrounding keratinocytes. Melanocytes are typically located in the basal layer of the epidermis, at the junction with the dermis. Differences in human pigmentation reflect variations in the number of melanosomes in keratinocytes and different melanin granule phenotype (depending on the eumelanin/pheomelanin ratio) rather than variation in the number of melanocytes. (Image courtesy of S. R. Granter, Brigham and Women's Hospital, Massachusetts.) b, Immunohistochemical analysis of the same human tissue as shown in a identifies melanocytes by using the immunohistochemical marker D5, which stains the MITF transcription factor located in their nuclei (Image courtesy of S. R. Granter.) c, Medaka goldfish are valuable in pigmentation studies. The wild type, B/B, is the lower of the two. Compared with this, b/b (top), which is bred for its golden colour, lacks melanin except in the eyes. The b locus is highly homologous with the locus for oculocutaneous albinism 4 (OCA-4) in humans, MATP or AIM1. MATP seems to be involved in melanocyte differentiation and melanosome formation. (Image reprinted, with permission, from ref. 82.) d, The yellow pigmentation in golden labradors is recessively inherited and results from an amino-acid substitution in Mc1r that produces a premature stop codon6. The same pigmentation can be seen in mice (Mc1re/e), horses and cats with hypomorphic Mc1r variants. (Image courtesy of Terra Nova.) e, Furred animals such as mice lack epidermal melanocytes (except in non-hair-bearing sites such as the ear, nose and paws). f, Polar bears have hollow unpigmented fur to blend in with the environment but, unlike other furred animals, have a high density of epidermal melanocytes, which aid in heat retention and produce black skin most notable in non-furred areas. (Image courtesy of First People.) In the human skin, melanocytes are present in the epidermis and hair follicles. The basic features of these cells are the ability to melanin production and the origin from neural crest cells. This last element is important because there are other cells able to produce melanin but of different embryonic origin (pigmented epithelium of retina, some neurons, adipocytes). The life cycle of melanocyte consists of several steps including differentiation of melanocyte lineage/s from neural crest, migration and proliferation of melanoblasts, differentiation of melanoblasts into melanocytes, proliferation and maturation of melanocytes at the target places (activity of melanogenic enzymes, melanosome formation and transport to keratinocytes) and eventual cell death (hair melanocytes). Melanocytes of the epidermis and hair are cells sharing some common features but in general they form biologically different populations living in unique niches of the skin. Melanocytes form a heterogeneous group of cells in the human body. Although all of them have ability to produce melanin and originate from embryonic cells named neural crest cells (NCC), their particular functions in all target places are much wider than the melanin synthesis only [1]. In the human body melanocytes’ presence does not confirm only epidermis, hair and iris where they give a color of these structures. Melanocytes have been also found in the inner ear, nervous system, heart and probably it is not the end of a list where these cells exist [2, 3]. It is necessary to stress that not only melanocytes have ability to produce melanin but also other cells e.g. cells of pigmented epithelium of retina, epithelia of iris and ciliary body of the eye, some neurons, adipocytes The life cycle of melanocytes consists of several steps including lineage specification from embryonic neural crest cells (melanoblasts), migration and proliferation of melanoblasts, differentiation of melanoblasts into melanocytes, maturation of melanocytes (melanin production in special organelles – melanosomes, dendritic morphology), transport of mature melanosomes to keratinocytes and eventual cell death. Several populations of neural crest cells (cranial, dorsal trunk, ventral trunk) give melanocytes of the skin. The embryonic origin of epidermal and hair melanocytes is the same but development is different [6, 7]. The problem of melanocyte stem cells’ localization in the adult skin is still a matter of debate. The first such place was a hair bulge, but if only…? [8]. Experimental data clearly show that the trunk NCC migrating through a ventral pathway could remain in a myelin sheath of the cutaneous nerves and in particular situations give melanoblasts [9, 10]. The embryonic development of melanocytes give an opportunity to better understand the skin diseases e.g. melanoma and its heterogeneity, vitiligo. Thus, in this review the epidermal and hair melanocytes’ biology and development are characterized. Abstract Biologically, light including ultraviolet (UV) radiation is vital for life. However, UV exposure does not come without risk, as it is a major factor in the development of skin cancer. Natural protections against UV damage may have been affected by lifestyle changes over the past century, including changes in our sun exposure due to working environments, and the use of sunscreens. In addition, extended “day time” through the use of artificial light may contribute to the disruption of our circadian rhythms; the daily cycles of changes in critical bio-factors including gene expression. Circadian disruption has been implicated in many health conditions, including cardiovascular, metabolic and psychiatric diseases, as well as many cancers. Interestingly, the pineal hormone melatonin plays a role in both circadian regulation as well as protection from UV skin damage, and is therefore an important factor to consider when studying the impact of UV light. This review discusses the beneficial and deleterious effects of solar exposure, including UV skin damage, Vitamin D production, circadian rhythm disruption and the impact of melatonin. Understanding these benefits and risks is critical for the development of protective strategies against solar radiation. Introduction The electromagnetic solar spectrum, which includes visible light and ultraviolet (UV) radiation among other radiation, plays a significant role in a variety of biological functions within a living system. In earth’s natural environment, we are exposed to the solar radiation in a regular 24 h cycle which varies according to the season. This radiation may have beneficial as well as harmful effects to living organisms. For example, UV radiation has many effects on the environment and the organisms inhabiting the planet. The most beneficial impact of UV light in humans is its essential role in the production of Vitamin D3 in the skin. Calcitriol, the active form of vitamin D3, participates in a variety of the body’s protective functions, including DNA damage repair and immune function. However, excessive exposure to UV radiation can have a variety of adverse effects on the skin, including cancers of the skin. Studies have suggested that solar radiations are important regulators of “circadian rhythms,” which by definition are physical, mental and behavioral changes that follow a ∼ 24 h cycle that primarily responds to light and dark in an organism’s environment Unfortunately, the lifestyle factors of the modern era such as the widespread use of artificial lights to extend our “daylight” time contribute adversely to the biological processes leading to unwanted conditions and responses. For example, excessive UV exposure to skin can cause skin aging, precancerous skin conditions and melanoma and nonmelanoma skin cancers. The modern research is suggesting that circadian rhythms may be involved in the development and/or progression of cancer because it is believed that ∼10% of the genes oscillate according to the body’s circadian clock. Their functions are widely varied but are connected with the normal cell cycle, metabolic functions and DNA damage repair. Normal circadian rhythms are therefore essential for the body’s natural defense against diseases such as cancer. It is believed that a deregulation of oscillatory expression and function of circadian rhythm regulatory genes over the 24 h period enhances the risk of carcinogenesis. Light and dark cycles influence the circadian clock and the daily oscillations of the genes controlled by the circadian rhythms. Although artificial light can also contribute to the circadian network, solar light is its major regulator. With increased exposure to artificial light, there is an increase in the probability of disrupting these rhythms, as circadian rhythm gene expression has been shown to be lower in artificial light relative to natural light. Altered circadian rhythm disrupts the DNA damage responses and cell cycle regulations as well as the expression of the pineal hormone melatonin. Like other circadian factors, the circadian control of melatonin secretion is regulated by the circadian clock machinery which depends on a network of genes and their rhythmic oscillations driven by the circadian timing system located in the suprachiasmatic nucleus (SCN) of the hypothalamus as well as peripheral oscillators located in cells. Dysregulated circadian control of melatonin can contribute to the adverse effects of UV radiation on the skin, as melatonin has been shown to have a protective role against UVB skin damage. Further, melatonin is a strong antioxidant and can attenuate UV radiation mediated oxidative stress. Indeed, low levels of melatonin have been associated with increased risk or shown to play a role in the development of several cancers Choosing the appropriate laser and the correct settings is vital in the treatment of melasma. The use of latter should be restricted to cases unresponsive to topical therapy or chemical peels. Appropriate maintenance therapy should be selected to avoid relapse of melasma. A selective window for targeting melanin lies between 630 and 1100 nm, where there is good skin penetration and preferential absorption of melanin over oxyhaemoglobin.[2] Absorption for melanin decreases as the wavelength increases, but a longer wavelength allows deeper skin penetration. Shorter wavelengths (<600 nm) damage pigmented cells with lower energy fluencies, while longer wavelengths (>600 nm) penetrate deeper but need more energy to cause melanosome damage. Besides wavelength, pigment specificity of lasers also depends on pulse width.[2] With an estimated TRT of 250– 1000 ns, melanosomes require submicrosecond laser pulses (<1 μs) for their selective destruction, but longer pulse durations in the millisecond domain do not appear to cause specific melanosome damage.[ Laser was compared with pre- or posttreatment TCC. The authors found that pre-treatment with TCCs was more effective as this decreases melanin production before laser injury, hence chances of PIH are reduced and the melasma is improved. If TCC is used after laser treatment, melanin is being produced at full capacity, hence increasing chances of PIH and slowing improvement of melasma. Hence, the authors recommend medical treatment for hyperpigmentation for at least 8 weeks before laser treatment to achieve optimal results. This technique used in the above studies has recently been referred to as “laser toning” or “laser facial” and has become increasingly popular. It is widely used in Asian countries for skin rejuvenation and melasma. Laser toning involves the use of a large spot size (6–8 mm), low fluence (1.6–3.5 J/cm2), multiple passed QS 1064 nm Nd:YAG laser performed every 1-2 weeks for several weeks.[ Rebound hyperpigmentation treated five Chinese patients with melasma with laser toning. There was no significant improvement in melasma and all five patients developed laser-induced depigmentation. Possible pathogenic mechanisms for this depigmentation could be high fluences causing direct phototoxicity and cellular destruction of melanocyte, subthreshold additive effect of multiple doses, intrinsic unevenness of skin pigmentation, and non-uniform laser energy output.Several other side effects mentioned in the literature include rebound hyperpigmentation, physical urticaria, acneiform eruption, petechiae, and herpes simplex reactivation. Rebound hyperpigmentation could be due to the multiple subthreshold exposures that can stimulate melanogenesis in some areas. They found that only 532 and 1064 nm at threshold and suprathreshold dose produced permanent leukotrichia. At subthreshold exposure, none of these wavelengths caused hypopigmentation but they accelerated melanogenesis. To avoid serious side effects, it is recommended that too many (>6-10) or too frequent (every week) laser sessions with QS Nd:YAG should be avoided. Hypopigmentation should be looked for after every session and further treatments should be stopped. The PIH could be due to the inflammatory dermal reaction induced by laser that stimulated the activity of melanocytes in treated skin. The occurrence of PIH limits the use of this laser for recalcitrant melasma. Moreover, there are hardly any studies documenting its efficacy in melasma. FRACTIONAL LASERS Fractional phtothermolysis is a new concept in laser therapy in which multiple microscopic zones of thermal damage are created leaving the majority of the skin intact. The latter serves as a reservoir for healing. These multiple columns of thermal damage are called microthermal treatment zones (MTZ) and lead to extrusion of microscopic epidermal necrotic debris (MENDs) that includes pigment in the basal layer. The viable keratinocytes at the wound margins facilitate the migration of MENDs. The depth and diameter of MTZ are determined by the energy levels used. 6 mJ/MTZ corresponds to a diameter of 80 μm and depth of 360 μm in each MTZ.[6] The density used and the number of passes determine the proportion of surface area treated. IPL and melanocytic lesions, treated two patients with epidermal melasma and achieved 76–100% clearance with fluence of 34 J/cm2, pulse width of 3.8 ms, double mode, and pulse delay of 20 ms.[52] However, three patients with mixed melasma showed less than 25% clearance with 615 nm filter, fluence 38 J/cm2, pulse width of 4.5 ms, double mode, and delay of 20 ms. Patients developed PIH. The only RCT done in this domain is that by Wang et al. in which patients with refractory melasma were treated with IPL and hydroquinone and compared with hydroquinone alone.[50] 570 nm cutoff filter was used in the first session and 590–615 nm filters for subsequent sessions to target deeper melanin. Fluence used varied from 26 to 33 J/cm2, double mode and pulse length of 3–4 and 4–5 ms, respectively. However, in this study the authors preferred to use long delay between pulses (30–35 ms) which is higher compared to other studies. The IPL group achieved a significant response (39.8% clearance) compared to control group (11.6% clearance). Treatment efficacy did not correlate with any variables, such as age, duration of melasma, or skin phototype. Also, there was recurrence 6 months after therapy indicating the need for additional treatments to maintain results. The laser settings play an important role in the treatment. 500–550 nm filters can be used initially and for epidermal lesions, whereas higher wavelength filters can be used to target deeper melanin hence patients with dermal/mixed melasma. The fluence can be modulated in relation to the anatomic sites. Higher fluence can be used for cheek and zygoma, whereas perioral region and neck need lower fluencies. Higher fluencies are useful for deeper lesions but cause PIH in dark skinned patients. Therefore, for darker skin, lower fluence should be used. Single pulses heat pigment well, but double or triple pulses should be used as they reduce the thermal damage by allowing the epidermis to cool while the target stays warm. The pulse duration used in the studies varied from 3 to 5 ms. Average pulse delay used was 10–20 ms. However, Wang et al. used long delay between pulses (30–35 ms) with good results.[50] It is important that delay time between pulses should not be below 10 ms as this increases the risk of thermal damage as the targeted tissue cannot reduce its temperature within that time. Average number of sessions used in these studies was 2–5 at an interval of 4–8 weeks. However, more number of sessions is required for maintenance and it decreases the chances of recurrence. It is a good approach to do a pre-test session before starting treatment to assess the efficacy of settings and look for any cutaneous hyper-reactivity. The studies show that IPL is effective for epidermal melasma. Dermal or mixed or refractory melasma can be targeted with higher fluencies though the risk of PIH should be kept in mind in darker skin. It is a good approach to use low fluences and long delay between pulses in such cases as done by Wang et al.[50] Also, sun protection and hydroquinone should be used throughout treatment and thereafter. Patients treated in these studies also had additional benefits of brighter skin colour, smoother skin texture, and uniform pigmentation.[ Zoccali and colleagues used dermoscopy to assess the area immediately after treatment session to choose the correct parameters: a transient hyperpigmentation (colour change to grey) indicating a correct IPL setting.[51] Postdermoscopy is helpful in evaluating the IPL efficacy and healing process. Post IPL dermoscopic finding can be classified into three patterns: (1) spotty/small dotted, (2) reticulated, and (3) complex (clumped). These clinical patterns represent clinical pictures of microcrust formed during the process.[ Kono and colleagues conducted a prospective direct comparison study of fractional resurfacing using different fluences and densities for skin rejuvenation and found that greater density was more likely to produce erythema, swelling, and hyperpigmentation.[ In order to treat melasma, combination or specially formulated creams with hydroquinone, a phenolic hypopigmenting agent, azelaic acid, and retinoic acid (tretinoin), nonphenolic bleaching agents, and/or kojic acid may be prescribed. For severe cases of melasma, creams with a higher concentration of HQ or combining HQ with other ingredients such as tretinoin, corticosteroids, or glycolic acid may be effective in lightening the skin. Azelaic acid 15%-20% (Azelex, Finacea) Retinoic acid 0.025%-0.1% (tretinoin) Tazarotene 0.5%-0.1% (Tazorac cream or gel) Adapalene 0.1%-0.3% (Differin gel) Kojic acid Lactic acid lotions 12% (Lac-Hydrin or Am-Lactin) Glycolic acid 10%-20% creams (Citrix cream, NeoStrata) Glycolic acid peels 10%-70% Other proprietary ingredients and mixtures of ingredients as in Elure, Lumixyl, and SkinMedica's Lytera products In conjunction with home cream applications, in-office treatments include chemical peels (chemical exfoliation), microdermabrasion (mechanical exfoliation), and laser therapy. These additional treatments may be useful for some cases of melasma, although laser still has issues with reproducibility. Many types and strengths of chemical peels are available for different skin types. The type of peel should be tailored for each individual and selected by the physician. In treating melasma, 30%-70% glycolic acid peels are very common. Various combinations, including a mix of 10% glycolic acid and 2% HQ, can be used to treat melasma. Microdermabrasion utilizes vacuum suction and an abrasive material like fine diamond chips or aluminum oxide crystals to exfoliate the top layers of the skin. The vacuum pressure is adjusted depending on the sensitivity and tolerance of the skin. Typical microdermabrasion sessions can last anywhere from a few minutes to one hour. Minimal to no recovery time is needed after microdermabrasion. Microdermabrasion techniques can improve melasma, but dramatic results are not generally seen or expected after one or two treatments. Multiple treatments in combination with sunscreen and other creams yield best results. There is no guarantee that melasma will be improved with these procedures. In some cases, if treatments are too harsh or abrasive, melasma can be induced or worsen. Additionally, these procedures are almost always considered cosmetic and may not be covered by medical insurance providers. Lasers may be used in melasma, but they generally produce only temporary results. Laser therapy is not the primary choice to treat melasma as studies reveal little to no improvement in the hyperpigmentation for most patients. Lasers may actually worsen some types of melasma and should be used with caution. Multiple laser treatments may be necessary to see results, as treatments are most effective when they are repeated. To ensure that treatment doesn't fail, people must minimize sun exposure. People who treat their melasma report a better quality of life because they feel better about themselves. As with any treatment, people should consult their physician. Pregnant women or mothers breastfeeding may need to wait to treat melasma. Many melasma creams need to be discontinued in pregnancy and breastfeeding because of possible risks to the developing fetus and newborn. These people may consider cosmetics to temporarily conceal the skin discoloration. Researchers believe that the hydroxyphenolic chemical (HQ) blocks a step in a specific enzymatic pathway that involves tyrosinase. Tyrosinase is the enzyme that converts dopamine to melanin. Melanin gives skin its color. Azelaic acid is a non-hydroquinone cream that can be used to treat melasma. Studies have reported that 15%-20% azelaic acid was very effective and safe in melasma, although the overall results are significantly less impressive than 4% hydroquinone. There are no major complications reported with azelaic acid. Possible minor side effects include itching (pruritus), redness (erythema), scaling (dry patches), and a temporary burning sensation that tends to improve after 14-30 days of use. Tretinoin cream (Retin A, Renova, Retin A Micro) is a non-hydroquinone cream used to treat melasma. Most often, tretinoin is used in combination with other creams like azelaic acid or hydroquinone. Mild localized side effects are fairly common and include peeling, dry skin, and irritation. Overall, melasma may respond slower to treatment with tretinoin alone than with hydroquinone. The Obagi system combines tretinoin with Obagi Blender. Other retinoid creams include tazaratone and adapelene. These are prescription creams used much like tretinoin (Retin A). [19] In fact, the only topical ointment currently approved by the US Food and Drug Administration (FDA) for the treatment of melasma is the Triple Combination Cream, a composite of hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01%. Comparative studies of the effectiveness of the Triple Combination cream vs topical HQ suggest that the combination cream is faster and more effective at reducing melasma pigmentation, but it does carry a slightly increased risk of an adverse reaction.[20] This is consistent with the theory of selective photothermolysis, which states that the pulse duration of an emitted laser wavelength must be less than the thermal relaxation time of the targeted object. A typical 1-µm melanosome has a thermal relaxation time of 0.5-1 microseconds. Tissue repair following laser-induced melanosomal disruption demonstrates a 2staged initial transient cutaneous depigmentation followed by subsequent repigmentation weeks later. Black guinea pig skin irradiated with 40-nanosecond Q-switched ruby pulses at a radiant exposure of 0.4 J/cm2 or greater whitens immediately, fades in 20 minutes, depigments 7-10 days later, and then repigments 4-8 weeks after treatment. The repigmented guinea pig skin displays a persistent leukotrichia, which can last up to 4 months after laser irradiation. Guinea pig skin exposed to a radiant exposure of less than that of the threshold exposure (< 0.3 J/cm2) undergoes paradoxical melanogenesis. This may be due to either a sublethal change in the melanosome (interfering with the normal feedback inhibition of melanogenesis) or simply postinflammatory hyperpigmentation. Further studies are required to evaluate the therapeutic implications of this paradoxical reaction. More recent guidelines advise against lasering "benign pigmented lesions" in tattoos, as 13 cases of melanoma have been reported at such sites. Thus, one must remove tattoos with pigmented lesions underneath with extreme caution.[82]