Introduction and Classification of Anaemia
PALI Haematology Session
3rd October 2012
Christopher Mullen
Overview of Presentation
•
•
•
•
•
•
•
•
Introduction
Classification
The Hypochromic Anaemias
Megaloblastic and other macrocytic anaemias
Haemolytic anaemias
Genetic disorders of haemoglobin
Investigation of the anaemic patient
Exam paper cases
Introduction
• Reduction in haemoglobin/red cell concentration in the blood
relative to the patient’s age and sex.
Age
Mean haemoglobin (g/dL)
1 month
140
6 months – 2 years
120
2 – 6 years
125
6 – 12 years
135
12 – 18 year old females
140
12 – 18 year old males
145
Adult females
140
Adult males
155
General Clinical Features
• Prevalent worldwide, especially among females
and children
• A reduction in the blood’s oxygen carrying
capacity leading to tissue hypoxia
• Clinical features relate to compensatory
mechanisms
– Cardiovascular: palpitations, chest pain, tachycardia,
intermittent claudication
– Skin: vasoconstriction and redistribution of blood flow
Classification
• Morphological classification
– Dependent on red cell indices i.e. MCV and
MCH/MCHC
– Macrocytic vs. normocytic vs. microcytic
– Hypochromia vs. normochromia
• Aetiological classification
– Haemorrhage
– Haemolytic
– Insufficient/ineffective haemopoiesis
The Hypochromic Anaemias
Differential Diagnosis
• Iron deficiency
– The most common cause of
anaemia worldwide
– Hypochromic, microcytic
anaemia (↓MCV, ↓MCHC)
•
•
•
•
Thalassaemia
Sideroblastic anaemia
Lead poisoning
Anaemia of chronic disease
(sometimes)
• Acronym - TAILS
Iron Deficiency Anaemia
Clinical Features
• Pallor of skin and
mucous membranes
• Painless glossitis
• Angular stomatitis
• Koilonychia
Aetiology
Aetiology
• Chronic blood loss – uterine
and gastrointestinal
• Dietary deficiency (rarely
alone)
• Increased demand –
pregnancy, lactation,
infancy etc.
• Gastrointestinal disease e.g.
coeliac, atrophic gastritis,
gastrectomy
• Helminth infections
Investigations
Iron deficiency anaemia is not
a diagnosis – an underlying
cause must be sought
• Blood film
• Iron studies – increased
total iron binding capacity
(TIBC), low serum ferritin
• Men and post-menopausal
women GI blood loss
occult blood testing,
endoscopy if suspicious
• Uncommon causes – CXR,
stool microscopy, cell
autoantibodies
Management
• Identify and treat underlying cause(s)
• Ferrous sulphate
• Parenteral iron where appropriate e.g. coeliac
disease, Crohn’s disease
Anaemia of Chronic Disease
• Associated with a
variety of malignant and
inflammatory diseases
• Normocytic and
normochromic (or
slightly microcytic
anaemia)
• Cytokines reduced red
cell lifespan and impair
haemopoesis
Macrocytic anaemias
• MCV abnormally large
(>98 fL)
–
–
–
–
–
–
–
–
Alcohol
Liver disease
Hypothyroidism
Myeloma and
paraproteinaemia
Myelodysplasia
Reticulocytosis
Pregnancy
Cytotoxic drugs e.g.
azothioprine
Megaloblastic anaemia
• Immature red cells
display delayed nucleus
maturation
• Due to defective DNA
synthesis
• Nearly always caused by
folate/B12 deficiency
B12 deficiency
• Absorbed in terminal
ileum (requires intrinsic
factor)
• Acts as a co-enzyme
• Deficiency takes 2 years
to develop
• Pernicious anaemia –
associated with
autoimmune diseases.
Autoimmune attack
against parietal
cells/intrinsic factor
Folate Deficiency
• Required for synthesis
of thymidine
monophosphate
(dTMP)
• Causes
– Poor diet
– Increased demand –
pregnancy (NTDs)
– Haematological disease
– Inflammatory disease
– Malabsorption
Clinical Features
• Lemon skin (jaundice and
pallor)
• Glossitis
• Subacute combined
degeneration of the cord in
severe B12 deficiency
• Macrocytic anaemia
• Mildly reduced WCC and
platelets
• Hypersegmented
neutrophils
• Raised unconjugated
bilirubin and LDH
Further Investigations
• Serum assays for folate
and B12
• Parietal cell and
intrinsic factor
antibodies
• Intestinal biopsy, antiTG if suspicious for
coeliac disease
Haemolytic anaemias
• Anaemia due to increased red cell destruction
• Can be hereditary or acquired
• Hereditary are due to intrinsic defects within red
cells
• Acquired are due to changes in red cell
environment
Classification
Hereditary
• Membrane defects
– Hereditary spherocytosis
– Hereditary elliptocytosis
• Enzyme defects
– Glucose-6-phosphate
dehydrogenase deficiency
– Pyruvate kinase deficiency
• Defects in haemoglobin
– Haemoglobin C, haemoglobin
S, unstable haemoglobin
Acquired
• Immune
–
–
–
–
Autoimmune warm
Autoimmune cold
Drug-associated
Transfusion-associated
• Infections
– Malaria
• Secondary to liver and renal
disease
• PNH
Clinical Features
• Pallor of mucous
membranes
• Jaundice
• Splenomegaly
• Damaged red cells on
blood film
• Erythroid hyperplasia of
bone marrow
• Bilirubinaemia and
increased urinary
urobilinogen
Chemical Features of
Intravascular Haemolysis
Intravascular Haemolysis
• Breakdown of red blood
cells in the circulation
• Haemoglobin is released
(haemoglobinaemia)
• Haptoglobins are saturated
• Haemoglobinuria
• Haemosiderinuria
• Methalbuminaemia
Extravascular Haemolysis
• Red cells are broken down
by macrophages or the
reticuloendothelial system
• Genetic disorder
• Reduced rate of synthesis of α
or β globin chains
• Common in Mediterranean
and South-East Asia
• Varies depending on number
of genes rendered inactive
• Marrow hyperplasia in βthalassaemia gives rise to
characteristic facies
• Diagnosed by haemoglobin
electrophoresis/high
performance liquid
chromatography
Genetic disorders of haemoglobin –
Sickle Cell Anaemia
• Inheritance of the sickle
β-globin gene
• Homozygotes (Hb SS) are
the most common
severely affected patients
• Severe haemolytic
anaemia associated with
“crises”
• Diagnosed via
haemoglobin
electrophoresis
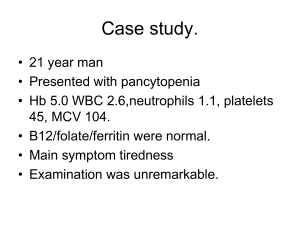
You are a GP trainee and Mrs J, a 24 year old lady, presents to the clinic. She has just
moved to your area, her notes haven’t arrived at the surgery, and she is complaining
of tiredness. She doesn’t wish to be fully examined but clinically you suspect
anaemia and you arrange a full blood count, results of which are shown below.
TEST
RESULT
REFERENCE RANGE
Hb
9.3g/dL
WCC
8.9 x 109/L
Platelets
304 x 109/L
150-400 x 109/L
MCV
104 Fls
80-96 Fls
11.5-13.5
4-11 x 109/L
She returns to health centre and this time you notice that she is also slightly icteric.
Urine analysis shows urobilinogen but no bilirubin. There is no glycosuria,
haematuria or pyuria. The serum bilirubin concentration is 65 Kmols/l (normal range
15 – 22 Kmols/litre).
1.
Apart from investigations for haemolysis, list two other investigations,
explaining your reason for doing the test to help elucidate the cause for
producing the increased MCV (2 marks)
2.
Apart from the results in the previous slide, list two biochemical or
haematological abnormalities that may occur in haemolysis
3. Explain in less than fifty words, why an
increase in serum bilirubin will not lead to
increased renal excretion of bilirubin. (2
marks)
4. List two defects in the red cells which can
cause haemolysis and give one example of
each (2 marks)
5. It transpires that Mrs J had a splenectomy for
this problem as a child and that she
subsequently had no follow-up or treatment
after this procedure. List two organisms you
would wish to vaccinate against. (2 marks)
6. List two pieces of advice you would wish to
instigate in patients following a splenectomy.
(2 marks)
• A 32 year old woman, who is a mother of four
children under aged 6 years, presents with increasing
fatigue and shortness of breath over recent months.
She has no significant past medical history. You find
her to be pale with: Hb 6.9 g/dl (Reference range 1113 g/dl), MCV 63fl (Reference range 78-96 fl), MCH
24 pg (Reference range 27-32pg)
1. What name is given to this blood picture? (2
marks)
– Microcytic hypochromic anaemia
2. What is the most likely haematological
disorder in this lady? (1 mark)
– Iron deficiency anaemia
3. List two possible significant factors
underlying in this patient. (2 marks)
4. What arterial PO2 would you expect? (1
mark)
5. You examine the blood report to find a
reticulocyte count? What are reticulocytes?
(1 mark)
6. What is the significance of a normal result?
(1 mark)
7. On further questioning, you discover this
patient’s ethnic background is South Asian.
8. What co-existing blood condition does this
patient have? How would you test for this? (2
marks)
• A 65-year-old lady presents
to her GP with a 3-month
history of vertigo, tinnitus
and visual disturbance. She
admits to feeling “a bit
down” and the GP decides
to carry out some routine
bloods. A week later she
returns and you note that
her blood results show a
raised high haemoglobin
and a raised pack cell
volume and red blood cell
count.
• A Burkitt’s Lymphoma
• B Chronic Lymphoid
Leukaemia
• C Chronic Myeloid
Leukaemia
• D Depression
• E Hodgkin’s Lymphoma
• F Pernicious Anaemia
• G Polycythaemia Vera
• H Sickle Cell Anaemia
• I Sideroblastic Anaemia
• J Thalassaemia
• A 12-year-old girl of
Nigerian descent and with a
known blood disorder
presents to A&E with a twoday history of dyspnoea,
cough and fever. You order
several investigations and
note that she has a Hb of
6g/dl (reference range 11.5
– 1.35 g/dl) and a chest Xray showing pulmonary
infiltrates.
• A Burkitt’s Lymphoma
• B Chronic Lymphoid
Leukaemia
• C Chronic Myeloid
Leukaemia
• D Depression
• E Hodgkin’s Lymphoma
• F Pernicious Anaemia
• G Polycythaemia Vera
• H Sickle Cell Anaemia
• I Sideroblastic Anaemia
• J Thalassaemia
• A 27-year-old man presents
with a two-month history of
pruritis, fatigue and weight
loss. On questioning he
admits that whenever he
drinks alcohol, he
experiences bone pain. On
examination he has a
rubbery non-tender
submandibular lymph node.
He has never had infectious
mononucleosis.
• A Burkitt’s Lymphoma
• B Chronic Lymphoid
Leukaemia
• C Chronic Myeloid
Leukaemia
• D Depression
• E Hodgkin’s Lymphoma
• F Pernicious Anaemia
• G Polycythaemia Vera
• H Sickle Cell Anaemia
• I Sideroblastic Anaemia
• J Thalassaemia
• A 68-year-old woman
presents with a history of
bruising, bone pain and
lymphadenopathy.
Unbeknownst to the
consultant, this patient has
a (t9,22) mutation known as
the Philadelphia
Chromosome. On
examination the consultant
finds a massively enlarged
spleen.
• A Burkitt’s Lymphoma
• B Chronic Lymphoid
Leukaemia
• C Chronic Myeloid
Leukaemia
• D Depression
• E Hodgkin’s Lymphoma
• F Pernicious Anaemia
• G Polycythaemia Vera
• H Sickle Cell Anaemia
• I Sideroblastic Anaemia
• J Thalassaemia
• A 37 year old lady with
known hypothyroidism
presents to you with
fatigue, dyspnoea and
palpitations. You note that
she is pale and tachycardic.
Routine bloods show a
macrocytic anaemia. You
suspect that this is caused
by her hypothyroidism. You
find a positive Schilling’s
test.
• A Burkitt’s Lymphoma
• B Chronic Lymphoid
Leukaemia
• C Chronic Myeloid
Leukaemia
• D Depression
• E Hodgkin’s Lymphoma
• F Pernicious Anaemia
• G Polycythaemia Vera
• H Sickle Cell Anaemia
• I Sideroblastic Anaemia
• J Thalassaemia
QUESTIONS?