HL7 FHIR in Practice: Healthcare Data Integration
advertisement

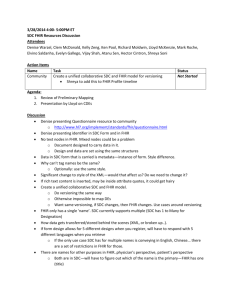
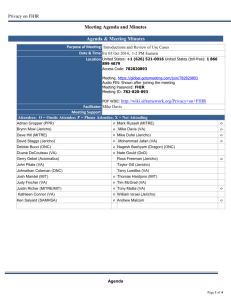
HL7 FHIR - IN PRACTICE Kevin Mayfield 19/6/2014 Background (Referral) • Health and Social Care Bill 2012-2013, The Scottish Government • NHS eHealth strategy - must contribute to care integration and support people with long term conditions • Replace shared assessment system with an Interagency Portal. • Build upon existing clinical portal Assessment - Me • 1996-2009 EMIS (GP Systems) – 300 baud drug ordering system – MOD 'GPtoGP' late 90’s – Defence Medical Information Capability Programme (DMICP), live streaming of clinical resources to/from operations in Iraq and Afghanistan • 2010- NHS & Council roles (SQL) – Community, Mental Health and Acute. – 2012 First HL7 interface Assessment - NHS Team • Using SCIXML and NHS Scotland Data Standards • Many bespoke interfaces and multiple integration engines. • Minimal exposure to HL7 standards. • Steep learning curve to HL7v3 and CDA. • RESTful? • Community care focused around documents (questionnaires/forms) Assessment - Social Services • 4 councils • HL7v2 capable (x1) • NHS (England) ITK and CDA interfaces. Keen to use FHIR (x2) • Bespoke (x1) • Organisation using a Care Plan model (x3) • RESTful Building The 'Care' Plan • IHE XDS, BPPC and PIX patterns. • Mostly UML focused (seen as too technical, flow charts preferred.) • Use cases very useful but a tendency to go for solution early. • FHIR and RESTful/CRUD used as model for technical discussions. • IHE and FHIR proved to be resistant to project changes (mostly consent and alerts) and change of supplier. Goals • Centralised recording of patients and consent • Document sharing with central index • Portal fed data by a variety of methods, mostly web services (HL7 FHIR preferred). Activities/Interventions (NHS) • Document Index using FHIR DocumentReference – Documents returned from many (NHS) sources using FHIR Binary – DocumentReference doubled up as a document notification system. • Questionnaires and other unstructured data using FHIR Questionnaires • Encounters, Care Plan, Orders, Appointments, Alert/Observation and Condition resources (NHS only). • Patient with consent extension and HL7v2 A28/31/40 Progress Notes • Naturally aligning with IHE profiles • Too many new things – FHIR being a major step towards HL7 CDA and IHE profiles – RESTful interfaces scaled down – Standard coding (SNOMED) premature • FHIR 80/20 rule nearly always correct • Resistance due to DSTU status – ReferralRequest – Consent – Appointments Review • Patient identity and consent first – Information Governance • Too much IT focus but the information model FHIR uses, especially the CarePlan resource, showed the way. • DocumentReference/Binary allowed the adoption of an XDS pattern and get the metadata correct – Path to HL7 CDA? • Questionnaires useful but need to used only when other resource not available (tended to capture the 20 in the 80/20) • Only suitable for NHS trusts/social services with EPR systems, PAS systems could stick with HL7v2 • SCRUM worked! FHIR allows sprints Questions?