Ebola and Inequality
advertisement
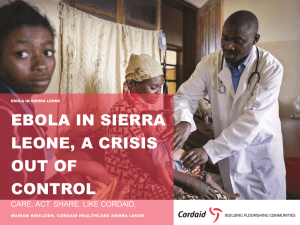
By: Calen Dehen “Ebola is a hemorrhagic fever of the filovirus family with a 50-90% fatality rate. There is no effective treatment for Ebola except for the euphemistically labeled “supportive therapy.” The virus is spread through contact with infected fluids, typically blood, and once it has infected a new patient, it rapidly attacks the internal organs and connective tissue, causes severe bleeding, vomiting, aches, mental impairments and dementia, and in severe cases, grand mal seizures. The typical cause of death is multi-organ system failure” (Jones, 2011). “Despite media attentions, the fear surrounding Ebola is in many ways overstated. The virus is indeed incredibly lethal- if you are infected. But in the course of over 30 years since its initial appearance, only 1,500 people have died in total. For comparison, twice as many children die of malaria each day” (Jones, 2011) The initial outbreak in 1976 received virtually no media coverage, and Western concern regarding the disease was very low. However, “In 1989, Ebola was detected in a shipment of crab-eating macaque monkeys to a laboratory in Reston, Virginia, and media frenzy ensued” (Jones, 2011). How does the media portray Ebola today? Why might it be different todaythan it was 30 years ago? “Ebola did not merely emerge; it emerged from Africa. This connection between African culture and Ebola is more than mere rhetorical racialization of the disease. Culture itself is reconstituted as a “risk factor” for infection in light of assumptions about African “Otherness.” In both popular and official accounts, African “beliefs”- often about disease etiology and transmission- are represented as ignorant and backwards, supposedly hindering or counteracting more enlightened epidemic control efforts” (Jones, 2011). Examples: Bushmeat Hypothesis- eating infected monkey or gorilla meat is main cause of virus’ spread to new populations Rejection of biomedicine- resorting to traditional healing and sorcery Ritual contact with the deceased How might the stereotype of African “Otherness” affect Americans’ willingness to help or donate to the cause of eradicating Ebola in Africa? “Many depictions of Ebola victims invoke the idea of African “traditionalists,” but a large number of those affected by Ebola live in cities, accept the biomedical model of disease, and are amenable to epidemic control efforts” (Jones, 2011). In fact, in the 1976 outbreak of Ebola in the Sudan, disease was spread rapidly by “substandard medical practices in a mission hospital. Apparently hospital staff had been giving patients injections with dirty needles” (Farmer, 1999). -5 needles used on 300-600 patients per day (Jones, 2011) Some people blame African culture as the reason for the Ebola outbreak. According to Farmer, in what ways do Americans use culture to contextualize the spread of disease s in America, such as HIV or tuberculosis, among the poor? “I joined the Red Cross when I was a child to work for humanity and to alleviate the suffering of the most vulnerable. I said, "I am from Kailahun. I must go to save my people.” When I reached Kailahun, it was like a war-torn country. My family was not happy; they were all scared and worrying. They called asking me to go back. My sister shed tears over the phone, but I reassured her. On average, we bury six bodies a day. The hardest part of the job is to take blood samples from the corpses. My guys are professionals now. Our personal protective equipment and a chlorine solution are our protection; they are our medication and they are our doctors. We maintain the ABC Rule: Avoid Body Contact. My last word of caution to them whenever we come from the field is: "Gentlemen, you have done safe work and I am confident you are safe in this moment. When you go home, be mindful of your personal activities until we meet again tomorrow.“ With this, no one has ever complained of even a simple headache. Thank God.” –Daniel James, burial leader (Bonifield, Christenson, and Wilson, 2014) How might Daniel’s perception of Ebola differ from that of an American? “The most well-demonstrated co-factors are social inequalities, which structure not only the contours of the AIDS pandemic but also the nature of outcomes once an individual is sick with complications of HIV infection. And a “cure,” though eminently desirable, will not change the prognosis for the vast majority of AIDS sufferers. The advent of more effective antiviral agents promises to heighten those disparities even further: a three-drug regimen including a protease inhibitor costs $12,000 to $16,000 a year. The formulators of health policy have already declared antiviral therapy to be “cost-ineffective” in the very regions in which HIV is most endemic” (Farmer, 1999). To what extent, if any, should cost be considered in determining who receives treatment for highly infectious diseases such as Ebola or HIV? “Simple laboratory test for Ebola are not available in local hospitals; blood or tissue specimens must be sent to special laboratories for definitive diagnosis. The patient usually dies within seven days of becoming symptomatic” (Hewlett and Bonnie, 2008). In regards to active tuberculosis: “Poverty and racism increase the likelihood of dire outcomes among the sick by restricting access to effective therapy or rendering it less effective if patients are malnourished or addicted. Poverty clearly decreases the ability of patients to “comply” with demanding, lengthy regimens. Indeed, the advent of truly effective therapies only brings into starker relief the centrality of social inequalities, when unequal access to these therapies heightens the inequalities of infection and reactivation already described” (Farmer, 1999). Inequality for the impoverished sick runs in a vicious cycle. Are there any solutions to this issue that would help these people in their lifetimes?