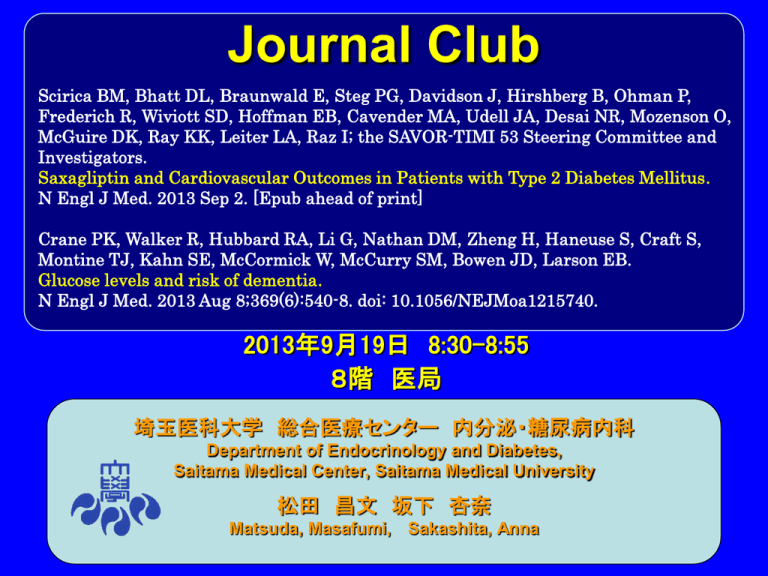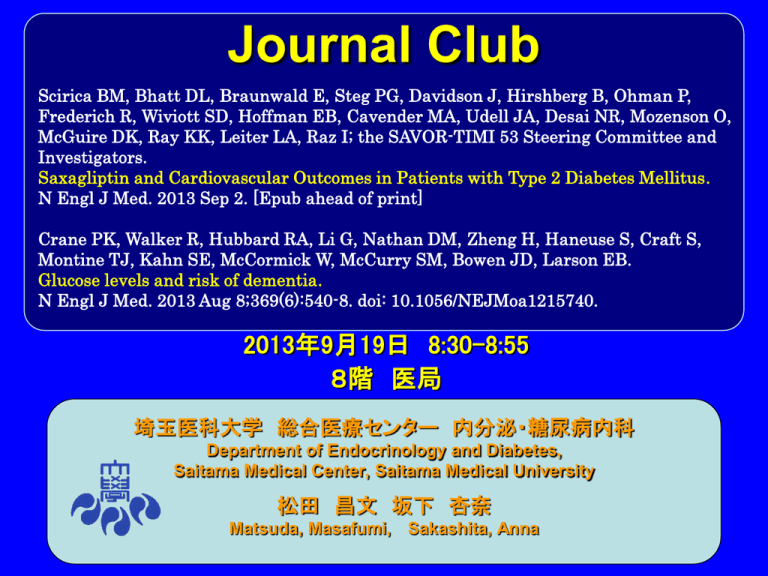
Journal Club
Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P,
Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mozenson O,
McGuire DK, Ray KK, Leiter LA, Raz I; the SAVOR-TIMI 53 Steering Committee and
Investigators.
Saxagliptin and Cardiovascular Outcomes in Patients with Type 2 Diabetes Mellitus.
N Engl J Med. 2013 Sep 2. [Epub ahead of print]
Crane PK, Walker R, Hubbard RA, Li G, Nathan DM, Zheng H, Haneuse S, Craft S,
Montine TJ, Kahn SE, McCormick W, McCurry SM, Bowen JD, Larson EB.
Glucose levels and risk of dementia.
N Engl J Med. 2013 Aug 8;369(6):540-8. doi: 10.1056/NEJMoa1215740.
2013年9月19日 8:30-8:55
8階 医局
埼玉医科大学 総合医療センター 内分泌・糖尿病内科
Department of Endocrinology and Diabetes,
Saitama Medical Center, Saitama Medical University
松田 昌文 坂下 杏奈
Matsuda, Masafumi, Sakashita, Anna
DPP-4阻害薬の心血管アウトカム試験
試験名
TECOS
EXAMINE
SAVOR-TIMI 53
CAROLINA
対象
2型糖尿病患者
急性冠症候群を合併 2型糖尿病患者
した2型糖尿病患者
2型糖尿病患者
薬剤名
シタグリプチン
アログリプチン
サクサグリプチン
リナグリプチン
対照薬
プラセボ
プラセボ
プラセボ
グリメピリド
登録例数
14,000例
5,400例
16,500例
6,000例
主要
エンドポイント
心血管死,非致死 心血管死,非致死的 心血管死,非致死
的心筋梗塞,非致 心筋梗塞,非致死的 的心筋梗塞,非致
死的脳卒中,不安 脳卒中の複合
死的虚血性脳卒中
狭心症による複合
の複合
心血管死,非致死
的心筋梗塞,非致
死的脳卒中,不安
狭心症による複合
観察期間
5年間
4.75年間
4年間
8.33年間
試験開始
2008年
2009年
2010年
2010年
試験終了予定
2014年12月
2013年12月
2013年7月
2018年9月
綿田裕孝(順天堂大学大学院代謝内分泌内科学)Pharma Medica ;30,8,157-164.2012.
clinicaltrials.gov(http://clinicaltrials.gov/)をもとに一部改変
the TIMI Study Group, Cardiovascular Division, Brigham and Women’s Hospital, and Harvard Medical
School (B.M.S., D.L.B., E.B., S.D.W., E.B.H., M.A.C., J.A.U., N.R.D.), and the VA Boston Healthcare System
(D.L.B.) — all in Boston; INSERM Unité 698, Université Paris-Diderot, and Département HospitaloUniversitaire FIRE, Hôpital Bichat, Assistance Publique–Hôpitaux de Paris, Paris (P.G.S.); the Divisions of
Endocrinology (J.D.) and Cardiovascular Medicine (D.K.M.), Department of Internal Medicine, University of
Texas Southwestern Medical Center, Dallas; AstraZeneca Research and Development, Wilmington, DE
(B.H., P.O.); Bristol-Myers Squibb, Princeton, NJ (R.F.); the Diabetes Unit, Department of Internal Medicine,
Hadassah University Hospital, Jerusalem (O.M., I.R.); the Cardiovascular Sciences Research Centre, St.
George’s University of London, London (K.K.R.); and the Division of Endocrinology and Metabolism,
Keenan Research Centre in the Li Ka Shing Knowledge Institute of St. Michael’s Hospital, University of
Toronto, Toronto (L.A.L.).
N Engl J Med 2013. DOI: 10.1056/NEJMoa1307684
Background
The cardiovascular safety and efficacy
of many current antihyperglycemic
agents, including saxagliptin, a
dipeptidyl peptidase 4 (DPP-4) inhibitor,
are unclear.
Methods
We randomly assigned 16,492 patients with
type 2 diabetes who had a history of, or
were at risk for, cardiovascular events to
receive saxagliptin or placebo and followed
them for a median of 2.1 years. Physicians
were permitted to adjust other medications,
including antihyperglycemic agents. The
primary end point was a composite of
cardiovascular death, myocardial infarction,
or ischemic stroke.
Figure 1. Kaplan–Meier Rates of the Primary and Secondary End Points. The
primary end point (Panel A) was a composite of death from cardiovascular
causes, myocardial infarction, or ischemic stroke.
Figure 1. Kaplan–Meier Rates of the Primary and Secondary End Points. The
secondary end point (Panel B) was a composite of death from cardiovascular
causes, myocardial infarction, ischemic stroke, hospitalization for unstable
angina, coronary revascularization, or heart failure.
Results
A primary end-point event occurred in 613 patients in the saxagliptin
group and in 609 patients in the placebo group (7.3% and 7.2%,
respectively, according to 2-year Kaplan–Meier estimates; hazard ratio
with saxagliptin, 1.00; 95% confidence interval [CI], 0.89 to 1.12; P =
0.99 for superiority; P<0.001 for noninferiority); the results were similar
in the “on-treatment” analysis (hazard ratio, 1.03; 95% CI, 0.91 to 1.17).
The major secondary end point of a composite of cardiovascular death,
myocardial infarction, stroke, hospitalization for unstable angina,
coronary revascularization, or heart failure occurred in 1059 patients in
the saxagliptin group and in 1034 patients in the placebo group (12.8%
and 12.4%, respectively, according to 2-year Kaplan–Meier estimates;
hazard ratio, 1.02; 95% CI, 0.94 to 1.11; P = 0.66). More patients in the
saxagliptin group than in the placebo group were hospitalized for heart
failure (3.5% vs. 2.8%; hazard ratio, 1.27; 95% CI, 1.07 to 1.51; P =
0.007). Rates of adjudicated cases of acute and chronic pancreatitis
were similar in the two groups (acute pancreatitis, 0.3% in the
saxagliptin group and 0.2% in the placebo group; chronic pancreatitis,
<0.1% and 0.1% in the two groups, respectively).
Conclusions
DPP-4 inhibition with saxagliptin did not
increase or decrease the rate of ischemic
events, though the rate of hospitalization for
heart failure was increased. Although
saxagliptin improves glycemic control, other
approaches are necessary to reduce
cardiovascular risk in patients with diabetes.
(Funded by AstraZeneca and Bristol- Myers
Squibb; SAVOR-TIMI 53 ClinicalTrials.gov
number, NCT01107886.)
Message
心血管イベント高リスクの2型糖尿病(DM)患者
1万6492人を対象に、DPP-4阻害薬saxagliptinの
効果を無作為化試験で評価(SAVOR-TIMI53試
験)。主要複合評価項目(心血管死、心筋梗
塞、虚血性脳卒中)はプラセボ群と同等だっ
た。心不全による入院はsaxagliptin群で多かっ
た(ハザード比1.27)
the Departments of Medicine (P.K.C., W.M., E.B.L.), Psychiatry and Behavioral Sciences
(G.L.), Pathology (T.J.M.), and Psychosocial and Community Health (S.M.M.), University of
Washington; the Group Health Research Institute (R.W., R.A.H., E.B.L.); the Department of
Medicine, VA Puget Sound Health Care System and University of Washington (S.E.K.); and
the Swedish Neuroscience Institute ( J.D.B.) — all in Seattle; the Diabetes Center and
Department of Medicine (D.M.N.) and the Biostatistics Center (H.Z.), Massachusetts General
Hospital and Harvard Medical School; and the Department of Biostatistics, Harvard School
of Public Health (S.H.) — all in Boston; and the Department of Internal Medicine, Wake
Forest School of Medicine, Winston-Salem, NC (S.C.).
N Engl J Med 2013;369:540-8. DOI: 10.1056/NEJMoa1215740
Background
Diabetes is a risk factor for dementia. It
is unknown whether higher glucose
levels increase the risk of dementia in
people without diabetes.
Methods
We used 35,264 clinical measurements of glucose levels
and 10,208 measurements of glycated hemoglobin
levels from 2067 participants without dementia to
examine the relationship between glucose levels and the
risk of dementia. Participants were from the Adult
Changes in Thought study and included 839 men and
1228 women whose mean age at baseline was 76
years; 232 participants had diabetes, and 1835 did not.
We fit Cox regression models, stratified according to
diabetes status and adjusted for age, sex, study cohort,
educational level, level of exercise, blood pressure, and
status with respect to coronary and cerebrovascular
diseases, atrial fibrillation, smoking, and treatment for
hypertension.
The sample for the current study was limited to 2067 participants who had at least one
follow-up visit, had been enrolled in Group Health for at least 5 years before study entry,
and had at least five measurements of glucose or glycated hemoglobin (measured as
hemoglobin A1c or as total glycated hemoglobin, with the latter measurement reflecting
an older hemoglobin assay) over the course of 2 or more years before study entry.
Identification of Dementia
Study participants were assessed for dementia every 2 years
with the use of the Cognitive Abilities Screening Instrument,
for which scores range from 0 to 100 and higher scores
indicate better cognitive functioning. Patients with scores of
85 or less underwent further clinical and psychometric
evaluation, including a battery of neuropsychological tests.
The results of these evaluations and laboratory testing and
imaging records were then reviewed in a consensus
conference. Diagnoses of dementia and of probable or
possible Alzheimer’s disease were made on the basis of
research criteria. Dementia-free participants continued with
scheduled follow-up visits. The incidence date for dementia
was recorded as the halfway point between the study visit at
which dementia was diagnosed and the previous visit.
Risk Factors Assessed
Glucose Levels
Diabetes
Apolipoprotein E Genotype
Other Risk Factors
exercise level
smoking status
blood pressure
atrial fibrillation
treatment of hypertension
obesity?
We transformed values for total glycated hemoglobin to
hemoglobin A1c values using this formula:
hemoglobin A1c = (0.6 × total glycated hemoglobin) + 1.7
We then transformed the calculated hemoglobin A1c values to
daily average glucose values with this formula:
daily average glucose = (28.7 × hemoglobin A1c) – 46.7
Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ. Translating the
A1C assay into estimated average glucose values. Diabetes Care 2008;31:1473-8.
[Erratum, Diabetes Care 2009;32:207.] (ref.10)
Figure S1. Glycemia distribution
throughout the study period.
Dementia, Alzheimer’s Disease, and Glycemia
Over a median follow-up period of 6.8 years, dementia developed in 524 of the
2067 participants (25.4%), including 450 of the 1724 participants who did not
have diabetes at the end of follow-up (26.1%) and 74 of the 343 participants
who had diabetes at the end of follow-up (21.6%). A total of 403 participants
(19.5%) had probable or possible Alzheimer’s disease at the end of follow-up,
55 (2.7%) had dementia from vascular disease, and 66 (3.2%) had dementia
from other causes.
Figure 1. Risk of Incident Dementia Associated with the Average Glucose Level
during the Preceding 5 Years, According to the Presence or Absence of Diabetes.
Solid curves represent estimates of the hazard ratios for the risk of incident dementia
across average glucose levels relative to a reference level of 100 mg per deciliter for
participants without diabetes (Panel A) and 160 mg per deciliter for participants with
diabetes (Panel B). The dashed lines represent pointwise 95% confidence intervals. To
convert the values for glucose to millimoles per liter, multiply by 0.05551.
We also found an inverse association
between glucose level and risk of
dementia among people with diabetes
who had relatively low levels of glucose,
although this association appeared to
be driven by glucose levels in three
participants with atypical courses of
type 2 diabetes.
This figure shows spline curves
for the relationship between
glycemia and dementia for
participants with diabetes,
stratified by age at study entry.
Ages at study entry range from
70 in the top left panel to 78 at
the bottom right panel (the
inter‐quartile range of age at
study entry for people with
diabetes). Higher risk
associated with both higher and
lower levels of glycemia appear
to be especially prominent
among people who were older
at study entry. We performed
these analyses for people with
diabetes because of the
suggestive p value for the age
at study entry interaction term
for all‐cause dementia among
people with diabetes (p=0.13).
Results
During a median follow-up of 6.8 years, dementia
developed in 524 participants (74 with diabetes and 450
without). Among participants without diabetes, higher
average glucose levels within the preceding 5 years
were related to an increased risk of dementia (P = 0.01);
with a glucose level of 115 mg per deciliter (6.4 mmol
per liter) as compared with 100 mg per deciliter (5.5
mmol per liter), the adjusted hazard ratio for dementia
was 1.18 (95% confidence interval [CI], 1.04 to 1.33).
Among participants with diabetes, higher average
glucose levels were also related to an increased risk of
dementia (P = 0.002); with a glucose level of 190 mg per
deciliter (10.5 mmol per liter) as compared with 160 mg
per deciliter (8.9 mmol per liter), the adjusted hazard
ratio was 1.40 (95% CI, 1.12 to 1.76).
Conclusions
Our results suggest that higher glucose
levels may be a risk factor for
dementia, even among persons without
diabetes.
(Funded by the National Institutes of
Health.)
Message
高齢者における機能変化を検討したAdult
Changes in Thought研究の参加者2067人
(平均年齢76歳)を対象に、血糖値と認知
症の関係を検討。非糖尿病者では過去5年の
平均血糖高値が認知症リスク増加と関連し
(P=0.01)、糖尿病(DM)患者でも平均血
圧高値がリスク増加と関連した
(P=0.002)。