Vidhi Shah - School of Medicine
advertisement

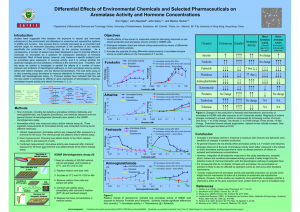
Frontal Fibrosing Alopecia as a result of medications and supplements Vidhi Shah, Colleen Reisz UMKC School of Medicine Introduction Frontal fibrosing alopecia (FFA) is a form of hair loss that affects the frontal hairline at menopause in white female patients. FFA is typically progressive and results in irreversible scarring and alopecia [1]. There is no reliable treatment of FFA but steroids, anti malarials and methotrexate have been tried [2]. The disease is considered progressive although there is a subset whose disease slows over time, regardless of treatment. We theorized that FFA is mediated by changes in local tissue aromatase activity affected by the use of medications and supplements in addition to the physiologic effects of age, body habitus, and hormonal status. Objectives FFA typically affects white women almost exclusively in the frontal hairline. The incidence of FFA is increasing [1]. The onset To collect biometric and pharmaceutical data in women with FFA for known factors that would alter aromatase. of FFA at menopause strongly implicates a hormonal effect although the exact mechanism is unknown [3]. To examine the effects of drug and supplement reduction (in Estrogen synthesis shifts from the gonad to peripheral fat tissue addition to diet and exercise) on FFA. starting in middle age, peripheral estrogen production is controlled by local transcription factors that regulate aromatase activity[ [4,6]. Aromatase exhibits regional and gender differences in the scalp, with women having a 6 fold increase in aromatase in the frontal scalp [5,6]. Methods Age, obesity, insulin resistance and drugs impact endocrine signaling pathways and have the capacity to up regulate aromatase [7]. Up regulation of aromatase leads to androgen depletion and the formation of harmful estrogen metabolites that affect fibroblasts and macrophages [5,8,9]. Data was collected on patients presenting to a private dermatology practice with FFA from 2011 to 2014. We collected biometric data, drug lists, including vitamins and supplements, Fitzpatrick phototyping and comorbid states. In addition to diet and exercise recommendations, vitamin and supplements were discontinued with the exception of vitamin D. Whenever possible, drugs known to increase insulin resistance were discontinued or modified to improve the insulin resistance profile. Response to therapy was defined as reduction in redness and scale at the follicular os and no further progression of alopecia. Patients were categorized as responders or non-responders. Results • 18 patients presented with FFA during the study interval. One patient was not accepting of therapy and one patient did not follow up. The remaining 16 patients are summarized in Table 1. • 9/18 patients who had medications adjusted along with discontinuation of vitamin and mineral supplements responded to therapy; 6 more have agreed to our suggestions on reduction • 1/2 patients who were not on medications known to affect insulin resistance or on vitamins/supplements improved with increase in vitamin D (pt 7) • 1 has had relentless progression and no response to treatment (pt 2) TABLE 1. Demographic, clinical and response characteristics of 16 women with FFA Patient No. Age/ age at onset of hair loss, y BMI Fitzpatrick Co-morbid conditions Xenobiotic Response/Reduction 1. 62 32.00 1 - Simvastatin, Metoprolol Lost to follow up 2. 62/59 28.30 1 Premature ovarian failure at 42 y - No response 3. 58/57 22.90 1 - V/S III Reduction in progress 4. 75/73 34.90 2 DM II Simvastatin + 5. 71/69 33.30 2 - V/S II + 6. 68/65 24.80 2 Morgellens disease see note V/S III + 7. 60/58 25.60 1 Multiple squamous cell carcinoma of the skin starting at menopause - + 8. 41/41 37.44 2 Preeclampsia II, Multiple Sclerosis Prednisone, Betaseron + 9. - - 1 Pharmacokinetic/photosensi tivity issues see note V/S III + 10. 73/73 26.07 2 - Atorvastatin, Metoprolol, Omeprazole, Losartan, Tramadol, Sertraline + 11. 65/56 25.09 1 - V/S II Simvastatin + 12. 39/39 21.48 4 Triathlete with special diet, creatine, whey, amino acids V/S III (10) Orsythia, Spironolactone + 13. 58/55 22.92 3 - V/S II Pravastatin, Lisinopril, Flax, Glucosamine Reduction in progress 14. 60/58 20.50 3 Raynauds,livedo, unclassified autoimmune disorder V/S II Switch from oral to patch estrogen Reduction in progress 15. 72/64 33.99 1 Hair loss temporally within one month of sertraline V/S III Atorvastatin, Sertraline, Mobic, Triamterene, Trazodone, Hydrocodone Reduction in progress 16. 56/55 18.56 2 - V/S III Sertraline, Evista, Triamterene Refused 17. 54/53 26.29 1 Gestational diabetes Prevacid Reduction in progress 18. 61/58 30.47 1 - V/S III Tamoxifen for 5 years, Resveretrol, Garcinia, Ubiquinol, Niacin, Coconut oil, Vitamin E, Fish oil, Reduction in progress *V/S I – 1-2 supplements, V/S II – 3-4 supplements, V/S III – Exuberant use of nutraceuticals. 5-6 supplements or more • 11/18 patients had a BMI greater than 25. • 11/18 patients were taking drugs known to negatively impact insulin resistance and increasing aromatase (most commonly a statin drug and/or sertraline). • 7/18 were on 5 or more supplements. Frontal fibrosing alopecia results from an inflammatory attack on the hair follicle in the frontal hairline in women at menopause. It occurs in women of Northern European ancestry and appears to be increasing in incidence [1,2]. We propose that women with FFA have difficulty navigating midlife changes in peripheral estrogen metabolism. The up regulation in aromatase may be physiologic and accompany age and menopause [6]. These changes may also be magnified by medications and supplements known to negatively affect insulin resistance and increase aromatase [8]. Physicians caring for women with FFA should include drug histories and drug stratification as part of their treatment plans. The prolific use of vitamins and supplements found in this series supports further investigation into the risks and benefits of this largely unregulated industry. References [1] Ladizinski B, et al. "Frontal Fibrosing Alopecia: A Retrospective Review of 19 Patients Seen at Duke University.” Journal of the American Academy of Dermatology. 2013; 68(5):749-755. [2] Otani C, et al. “Frontal fibrosing alopecia associated with lichen planus pigmentosum.” Journal of the American Academy of Dermatology. 2013; 68 (4): AB51 [3] Cutolo M, et al. "Estrogen Metabolism and Autoimmunity.” Autoimmunity Reviews. 2012; 11:A460-A464. [4] Inoue T, et al. "The Role of Estrogen-metabolizing Enzymes and Estrogen Receptors in Human Epidermis." Molecular and Cellular Immunology. 2011; 344: 34-40. [5] Cutolo M, et al "Oestrogens in Rheumatic Diseases: Friend or Foe?” Rheumatology (Oxford) 2008; 47: (Suppl, 3): iii 2-5 [6] Yip L, et al. "Gene-wide Association Study between the Aromatase Gene (CYP19A1) and Female Pattern Hair Loss." British Journal Dermatology.2009; 289-94. [7] Marino JS, Xu Y, Hll JW. Central Insulin and leptin-mediated autonomic control of glucose homeostasis. Trends Endocrinol Metab. 200;22:275-285. [8] Morris P, et al. "Inflammation and Increased Aromatase Expression Occur in the Breast Tissue of Obese Women with Breast Cancer." Cancer Prevention Research. 2011; 4(7):1021-1029. [9] Tamir S, et al. “The Effect of Oxidative Stress on ER alpha and ER beta Expression.” Journal of Steroid Biochemistry & Molecular Biology. 2002; 327-332. Special thank you to Dr. John Foxworth PharmD for paper review and advice. • 15/18 patients were Fitzpatrick level I and II, consistent with other studies showing a predominance in women of Northern European ancestry. The racial predominance seen in FFA implicates a genotypic basis for the disease. Fitzpatrick phototyping is a clinical tool for objectively assessing skin pigmentation which may also be a potential biomarker of vitamin D status and genotypic variation in the human aromatase complex. Discussion Pt 4-Baseline and one year after changing the statin from simvistatin to atorvastatin. The patient also started metformin which lowers aromatase