Using-EMR-Scribes-in-Primary-Care-Practice
advertisement

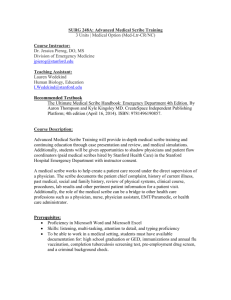
EHR Scribes A Post-Implementation Strategy Ann Murphy, MD -- Charles Kitzman CIO – Michaela Mangas Shasta Community Health Center, Redding CA Fast facts…. • • • • 30 FT Provider FQHC Live on since May 2007 130,000 encounters annually Multiple services • • • • • • Primary Care Pediatrics Primary Care Neuropsychiatry Urgent Care Homeless Van Various Specialties – Rheumatology, Podiatry, Neurology, etc and a partridge in a pear tree….. Live on EHR….so what’s the problem? Pilfered from thisisindexed.com Weighing the results Eh? Good stuff • • • • Legible charts ePrescribing Solid lab interfaces Flexible platform • • • • Enhancement process Individual practices Reduced access/capacity Flexible platform 2 areas to address…. Documentation/Quality • Organizational undercoding • Data capture could be better • Pt. Satisfaction surveys were critical of EHR processes Productivity • Very gradual decline in productivity • Increase in billable hours • Clinician burnout • Difficult recruitment • Primary care less popular than $pecialty care Big on ideas, short on cash…. Score! Grantor 3rd party Evaluator 4 month evaluation period* *Probably too short but more about that later Scribing Goes Way Back!! Applying old methodologies to newer processes Early on….setting the table • Clinician interest was quite low • Trust/Control Issues • Our method of “selling” the idea was flawed • “Barnum & Bailey – Get ‘em in the Tent” approach • Learned quickly that familiarity is best • Had to develop Training/Assessment Process • Michaela was a big help – ER experience • System/Clinical parts – Set guardrails • Develop standards for scribe candidates • College educated – Interest in medicine • “JV Residency” Scribe Profiles Lead Scribe Works with Clinician Train New Scribe Candidate Outline Preferences Train w/Clinician Document workflow Learns System Clinical Homework Shadow Lead Scribe Dev Training Tools Handoff Query for Common “Scribrary” • Dx – Meds - Ordering Sample Visits See 1 - Do 1 Go live Recruitment and Training Process Risks • CPOE numbers could be impacted • Clinicians could be left “stranded” if they don’t have a scribe • Gender issues may interfere with care • Learning/Training curve might negatively impact access • Scribes might be traumatized by our patients Sample Group & Criteria Control Group Surprises • “Saves at least an hour of work.” • “I enjoy the ability to focus on my patients.” • “My notes are actually better and contain more data.” • “It makes a difference in how my day goes.” • “I sure miss my scribe when she’s out sick!” Clinician Testimonials Case studies • First Case – MD Veteran Clinician • Documentation – Initial E/M coding 90% Chief Complaint 90% W/Scribe showed Moderate improvement. • Improved timeliness of notes • +108 Encounter over the same period the year prior • 1.09 Enc/Ttl Hours 1.32 Enc/Ttl Hours Case studies • Second Case– FNP With Practice 5 years • Documentation – Initial E/M coding 45% Chief Complaint 75% • W/Scribe showed good excellent improvement. • Decrease in getting notes done day of visit • Access - +2 encounters over same period year prior • 1.23 Enc/Ttl hours 1.42 Enc/Ttl hours Case studies • Second Case– MD Approaching Retirement • Documentation – It’s Better to actually show you. Conclusions Conclusions ? Clinician/Scribe Perspective Questions