UTI prevention in Older Patients with Foley Catheters
advertisement
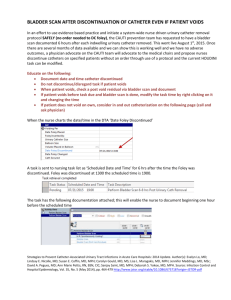
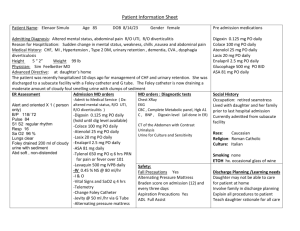
UTI Prevention in Patients with Foley Catheters Lourdes Health Network 2011 Background UTIs account for over 6 million patient visits to physicians per year in the United States. UTIs are the most common hospital acquired (HA) infection 80% of HA-UTI are attributable to indwelling urethral catheters. 12-16% of hospitalized patients will get a Foley and half of them do NOT have a valid indication. Risk of UTI increases 3-7% for every day with Foley Relevance UTIs increase a patient’s length of stay an average of 0.5 -1 day The estimated cost per Catheter Associated UTI (CAUTI) ranges $500$3000 If not documented upon admission (CAUTI), then hospital cannot code for higher reimbursement DRG for Medicare patients in some hospitals Urinary Tract Infections Definition of UTI a microbial infection (typically bacterial) of the urethra, bladder, ureters, or kidneys. Most common is Escheria coli UTI Definition continued… Symptomatic more typical presentation (burning with urination, urinary frequency, low fever, cloudy urine (possibly), foul odor to urine, pressure or cramping in lower abdomen Asymptomatic bacteriuria a significant number of bacteria in the urine that occurs without usual symptoms such as burning during urination or frequent urination. Those with urinary catheters will more likely have this condition. 3 Primary Routes of Infection 1. Catheter-meatal junction 2. Catheter manipulation 3. More often in females (shorter urethra) Example: allowing drainage spout to touch the ground or contaminating the catheter tubing while placing a new drainage bag. Retrograde bacterial migration Example: lifting bag above level of bladder during transport or repositioning More about indwelling catheters…. They are uncomfortable for patients Can be unnecessary for patient treatment plan (41-58% in place found to be not indicated) Can be associated with negative outcomes Urethral inflammation Urethral strictures Mechanical trauma to urethra/bladder Can DECREASE mobility (because the patient does not have to get out of bed to urinate) which may impede recovery or contribute to complications like pressure ulcers, pneumonia, and/or DVT Appropriate Indications For Foley Catheters per LHN Protocol Criteria for Continuing Foley Catheter Strict I & O or aggressive treatment with diuretics or fluids Chronic urinary retention or bladder outlet obstruction Critically ill patient – hemodynamic instability Renal failure Recent renal/urology procedure Acute neurogenic bladder History of chronic, prolonged catherization or suprapubic catheter Hematuria Chemical sedation or paralyzation Terminally ill or palliative care patient Epidural catheter Pelvic or hip fracture Stage 3 or greater pressure ulceration on coccyx or buttocks Urinary Catheters are NOT Indicated for: Immobility or poor mobility General incontinence Skin excoriation Obtaining urine specimens Patient request Nurse convenience What is a Nurse Initiated Foley Removal? A policy developed in keeping with national best practice standards which ensures that Foley catheters are used appropriately. Facilitates nursing assessment for approved indications for the use of a Foley catheters Nurses are empowered to remove unnecessary catheters (those not meeting an approved criteria) without a doctors order. Enables catheters to be removed earlier! Decreases potential for hospital acquired UTIs in our patients!!! This policy has been supported and approved by MEC! Foley Removal Assessment & Documentation on Meditech Foley Removal Assessment & Documentation on Meditech continued . . . . Look up for continuing Foley If the patient does not meet any of the criteria for continuing the Foley catheter, REMOVE THE CATHETER! Post catheter removal Educate patient about what to expect (e.g. to notify nursing with the first voided specimen, measuring urine, getting help if needed to go to the BR, etc.) Document due to void time(5 – 8 hours post catheter removal) and communicate this with the oncoming shift! Scan patients bladder and notify physician of inability to void if the patient is unable to void post removal. Documentation of removal & due to void time (DTV) Document Output - Post Catheter Removal If Urinary Catheterization continues to be appropriate. . . . Use aseptic technique during subsequent catheter insertion and care Properly manage the system and components Keep closed drainage system Keep bag below level of the bladder Prevent excessive manipulation of the catheter Keep bag off of the floor Secure catheter to leg Provide catheter care daily and after bowel movements Continue to educate and advocate for the prompt removal of the Foley catheter References Institute for Healthcare Improvement-Preventing CAUTI http://www.ihi.org/IHI/Programs/ImprovementMap/PreventCatheterAssoc iatedUrinaryTractInfections.htm Lo, E., Nicolle, L, Classen, D., et al. (2008). Strategies to prevent catheterassociated urinary tract infections in acute care hospitals. Infection control and hospital epidimiology. October, Vol 29, Supplement 1. (Supplement article: SHEA/IDSA practice recommendations) Nazarko, Linda (2008). Reducing the risk of catheter-related urinary tract infection. British Journal of Nursing, Vol 17, No 16. Gotelli, J., Merryman, P., Carr, C., McElveen, Epperson, C., & Bynum, D. (2008). A quality improvement project to reduce the complications associated with indwelling urinary catheters. (Society of Urologic Nurses and Associates) Urologic Nursing. pp.465-473. Vieira, Fabricia (2009). Nursing actions to prevent urinary tract infection associated with long-standing bladder catheter. A Literature Review. Einstein; 7 (3 part 1): 372-5. References continued . . . . Centers for Disease Control and Prevention National Healthcare Safety Network (NHSN) Association for Professional Infection Control and Epidimiology (APIC) Busuttil Leaver, Rachel (2007).The evidence for urethral meatal cleansing. Nursing Standard. June, vol 21, no 41. 2009 NACNS National Conference Abstracts (March 5-7, 2009), St. Louis, Missouri.Creating a foley free zone by preventing and removing unnecessary urinary catheters. www.cconline.org. Clinical Nurses finding evidence for practice: reducing catheter-associated urinary tract infections. Critical Care Nurse. April, 29 (2)