Antibiotic-Awareness-Week-2014-Presentation-For-Use
advertisement
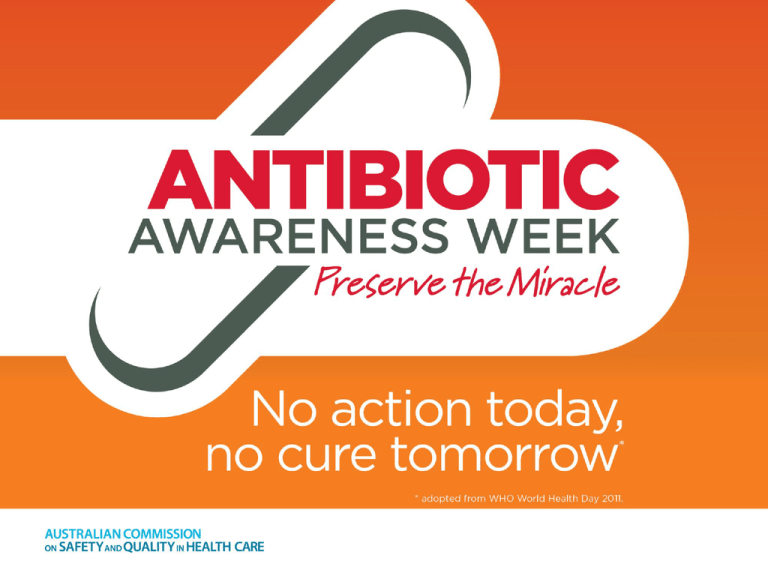
Overview • • • • • Antibiotic resistance – a global issue The link between antibiotic use and resistance Addressing antibiotic resistance The role of antimicrobial stewardship Actions for Antibiotic Awareness Week – 7 ways to improve antibiotic use Wherever they are used, antibiotics must be used responsibly The “miracle” of antibiotics • Discovery of penicillin revolutionised treatment of infectious disease • Increased life expectancy due to ability to prevent and treat infection Crude mortality rates for all causes, non infectious causes and infectious diseases over the period 1900-1996. 1. Armstrong GL et al, JAMA 1999;281(1):61-66 “Anne Miller, 90, first patient who was saved by penicillin” In 1999, the New York Times published an article about Anne Sheafe Miller…. “…who made medical history as the first patient ever saved by penicillin…died on May 27 in Salisbury, Conn. She was 90…..” • March 1942 - Mrs Miller was near death, suffering from a streptococcal infection. Doctors had tried everything available (sulfa drugs, blood transfusions, surgery). All treatments failed. •Desperate, doctors obtained a tiny amount of what was still an obscure, experimental drug and injected Mrs Miller with it. •Her hospital chart (now an exhibit at the Smithsonian Institution), registered a sharp overnight drop in temperature, and by the next day she was rapidly recovering. Mrs Miller's life was saved by antibiotics. •Penicillin also saved the lives of all those previously felled by bacterial infections with streptococci, staphylococci and pneumococci, and the lives of an untold number of servicemen and civilians wounded in World War II. 2. Saxon W, New York Times, June 9, 1999 Antibiotics continue to save lives, every day… • Ability to control infection is critical to other advances in medicine – – – – – – – Neonatal care Transplantation Chemotherapy Immunosuppression Complex and routine surgery Obstetric care Intensive care interventions But…….Antibiotics are a limited resource We have….. Growing rates of resistance Increased use of antibiotics Decreasing pipeline of new antibiotics 3. Spellberg, B. et al. Clinical Infectious Diseases 2008; 46 (2):155-64 Emergence of antibiotic resistance “It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body.” Sir Alexander Fleming, 1945 The issue of antibiotic resistance was recognised early in the ‘antibiotic era’. It threatens our ability to control infection. 4. Sir Alexander Fleming, Nobel Lecture, December 1945 Emergence of antibiotic resistance Antibiotic resistance threatens ability to control infection 5. Pray LA Insight Pharma Reports 2008, in Looke D ‘The Real Threat of Antibiotic Resistance’ 2012 Resistance spreads rapidly 6. Centers for Disease Control and Prevention http://www.cdc.gov/hai/ Impact of resistance • Increased morbidity/ mortality – Evidence across many pathogens • Untreatable infections – Now being encountered • Increased costs9 – $18-29,000 US/patient – Excess length of stay 6.4 – 12.7 days/patient Real people are affected 7. IDSA ‘Patient stories’ 2013 http://www.idsociety.org/Patient_Stories/ 8. Roberts RR et al. Clinical Infectious Diseases 2009; 49:1175-1184 AMR is a problem globally…… Key findings: • Very high rates of resistance observed for common bacteria that cause common health care associated and community acquired infections (for example urinary tract, pneumonia) in all WHO regions • Significant gaps in surveillance • Urgent need to strengthen collaboration on global surveillance as the foundation of global strategies to address AMR. 9. World Health Organization 2014 Antimicrobial Resistance: Global Report on surveillance. http://www.who.int/drugresistance/documents/surveillancereport/en/ Last accessed 21/9/14 ……a problem in our region….. China* ECOL: 54% KPNE: 41% India Thailand* ECOL: 78% ECOL: 55% KPNE: 64% KPNE: 50% Malaysia ECOL: 36% KPNE: 45% Korea ECOL: 37% KPNE: 40% Hong Kong ECOL: 46% KPNE: 23% Singapore ECOL: 21% KPNE: 32% Indonesia ECOL: 71% KPNE: 64% Resistance (%ESBL) in the Asia Pacific region 10. Mendes et al., Antimicrob. Agents Chemother. 2013 11. Xiao et al, Drug Resist Updat, 2011 (2009 data) 12. Chong et al., EJCMID, 2011 (2009 data) Japan† ECOL: 17% KPNE: 11% Philippines ECOL: 47% KPNE: 23% Australia ECOL: 12% KPNE: 15% Taiwan ECOL: 91% KPNE: 75% New Zealand ECOL: 11% KPNE: 10% ….and a problem here in Australia We need to act now!! 13. Turnidge J et al. MJA 2009: 191(7): 368-373 14. Looke DF, Gottlieb T, Jones CA, Paterson DL Med J Aust. 2013 Mar 18;198(5):243-4. Antibiotic resistance: in our health service • Which infections are we seeing ? • What are our susceptibility and resistance patterns ? – [Insert hospital data] – [Numbers of cases] – [Examples of cases] The link between antibiotic use and antibiotic resistance Countries with high penicillin consumption also have high rates of penicillin resistance in pneumococci Occurrence of penicillinnonsusceptible Streptococcus pneumoniae (PNSP) versus outpatient use of penicillins in 17 European countries. 15. van de Sande-Bruinsma N et al. Emerging Infectious Diseases 2008; 14(11):1722-1730 Antibiotic usage varies between hospitals Even within a county there is inter-hospital variation in antibiotic consumption e.g. Meropenem use – 10-fold variation across 64 Australian hospitals other carbapenems combined 80 70 National Antimicrobial Utilisation Surveillance Program (NAUSP) 2013-14 annual report14 60 50 40 30 20 10 0 M7 F3 K3 P6 W5 D8 V5 A9 J8 K7 T5 I7 H7 N5 G3 K4 O3 R3 D3 S3 G2 F8 H9 T4 L8 Z9 T3 M6 U2 W7 U6 R8 L5 G5 W6 E4 G9 O2 D5 Q8 K2 G6 Y6 O7 E7 L6 L3 D2 U7 B2 Q3 C5 W9 O5 L7 P8 C2 N9 R4 V4 F7 O4 Z6 P4 Antimicrobial usage rate (DDD per 1000 OBDs) meropenem Contributor code 16. South Australian Infection Control Service. National Antimicrobial Utilisation Surveillance Program (NAUSP) 2013-14 Annual Report. Adding to the problem …. Antibiotics are a limited resource • Few new antibiotics • Majority developed pre 1970 • 3 new classes in 20 years Global recognition that: • new antibiotics are urgently required • we need to conserve what we have The dwindling development of antibiotics… Number of US FDA Antibiotic approvals18 19 17: Adapted from Spellberg B et al. The epidemic of antibiotic resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Inf Dis 2008;48:155-64 A great deal of antibiotic use is inappropriate There is evidence to suggest that 25 - 50% of antibiotic prescribing in Australian Hospitals is inappropriate19 This includes; • Unnecessary prescription of antibiotics, such as for viral infections (colds) or for prolonged prophylaxis • Using broad-spectrum antibiotics (such as third generation cephalosporins, carbapenems) when narrowspectrum antibiotics are effective • Prescribing too low or too high a dose of antibiotic • Continuing treatment for longer than necessary • Not prescribing according to microbiology results • Omitting doses or delayed administration 19 . Duguid M and Cruickshank M. Antimicrobial Stewardship in Australian Hospitals . 2011 Antibiotic usage in our health service • Insert local usage data if available • Include information about local participation in the National Antimicrobial Prescribing Survey 2013/14 if participating, insert relevant results What can be done to address antimicrobial and antibiotic resistance ? Two complementary arms • Infection prevention and control • Antimicrobial stewardship Addressing Antibiotic Resistance in our health service. • Infection prevention and control – Hand hygiene – Standard and transmission based precautions – Environmental cleaning – Aseptic technique – Workforce immunisation • Antimicrobial stewardship NSQHS Standards, Standard 3: Antimicrobial Stewardship Criterion Actions required: 3.14.1 An AMS program is in place 3.14.2 The clinical workforce prescribing antimicrobials have access to endorsed Therapeutic Guidelines on antibiotic usage 3.14.3 Monitoring of antimicrobial usage & resistance is undertaken 3.14.4 Action is taken to improve effectiveness of your AMS program 20. National Safety & Quality Health Service Standards .Access at www.safetyandquality.gov.au/our-work/accreditation/nsqhss/ Antimicrobial stewardship (AMS) Optimising use of antibiotics • Aim to: – Maximise best outcomes – Minimise harm to the individual – Minimise ecologic harm to wider community • Requires team work at all levels: – Executive and clinical leadership – The clinical team (doctors, nurses, pharmacists, allied health) – Consumers Antimicrobial stewardship (AMS) • an inter-professional effort, across the continuum of care • timely and optimal selection, dose and duration of an antimicrobial • promotes best clinical outcome for the treatment or prevention of infection • minimal toxicity to the patient • minimal impact on resistance and other adverse events 21. Nathwani D and Sneddon J Practical Guide to Antimicrobial Stewardship Essential strategies for effective AMS Antimicrobial Stewardship in our Hospital • Local processes for stewardship – Include local processes for seeking ID/micro consults and pharmacy advice, guideline and formulary information, contacts, any other relevant information. Our Health service tools and activities to promote appropriate use of antibiotics • AMS committee (or other committee e.g. infection control, drug & therapeutics committees) to coordinate activity • Education – prescribing guidelines • Policy – Formulary with restrictions and approval • Access to expert prescribing advice – ID, Micro, Pharmacy • Audit and feedback • Who to contact? Therapeutic Guidelines: Antibiotic A quick note… • Current Version 14 being revised • Version 15 available November 2014 • http://www.tg.org.au Antibiotic Awareness Week 2014 • Coordinated by The Australian Commission on Safety and Quality in Health Care • National working group, “One Health” focus: – Australian Department of Agriculture, Australian Department of Health, State and Territory Health department representatives, NPS MedicineWise, Australian Veterinary Association • Supported by: – Australasian College for Infection Prevention and Control – Australasian Society for Infectious Diseases – Australian Society for Antimicrobials – Society of Hospital Pharmacists of Australia Australian Commission on Safety and Quality in Health Care No action today, no cure tomorrow* 7 Actions YOU can take 1. Obtain cultures before starting therapy 2. Use Therapeutic Guidelines: Antibiotic22 3. Document indication and review date 4. Review and reassess antibiotics at 48 hours 5. Consider IV to oral switch 6. Seek advice for complex cases 7. Educate consumers about antibiotic use What else can you do to improve antibiotic use ? 22. Therapeutic Guidelines: Antibiotic. Version 14. 2010 *adopted from WHO World Health Day 2011 Antibiotic Awareness Week What is happening in our health service ? • Local activities, contacts • Include information about local activities. NPS MedicineWise Take the health professional pledge • Visit nps.org.au/antibiotics to access resources for health professionals and consumers. • Become an antibiotic resistance fighter: take the health professional pledge. • Join the conversation on twitter @NPSMedicineWise or facebook.com/npsmedicine wise. A global effort • European Antibiotic Awareness Day http://ecdc.europa.eu/en/eaad/ Pages/Home.aspx • Canadian Antibiotic Awareness Week http://antibioticawareness.ca/ • United States Get Smart About Antibiotics Week http://www.cdc.gov/GetSmart/c ampaignmaterials/week/index.html Join the conversation Follow us on Twitter @ACSQHC Monday 17 November • Australian Antibiotic Awareness Week • #ABXAus Tuesday 18 November • #AntibioticDay • A global twitter chat involving partner countries • Organisations and experts participating “Never underestimate the importance of consumer groups and civil society in combating antimicrobial resistance. They are important movers, shakers, and front-line players, especially in this age of social media”. 23. Dr Margaret Chan, Keynote address at the conference on Combating antimicrobial resistance: time for action Copenhagen, Denmark 14 March 2012 . http://www.who.int/dg/speeches/2012/amr_20120314/en/ last accessed 22/9/14 Remember…. Antibiotics are a limited, precious resource • Antibiotic resistance is a growing, global problem • Antibiotic resistance is an issue in our hospitals and in our communities, for all of us who prescribe or use antibiotics • Resistant infections are harder to treat and are associated with higher rates of mortality and morbidity • Inappropriate use of antibiotics promotes resistance • Few new antibiotics are being made available • To conserve the antibiotics we have, antibiotics must always be used responsibly • If we don’t all take action today ……. there may be no cure tomorrow… Acknowledgements and References • • • • • • • Australian Commission on Safety and Quality in Health Care – Antibiotic Awareness Week working group members – AMS Jurisdictional Network – AMS Advisory Committee Australian Group on Antimicrobial Resistance National Antimicrobial Utilisation Surveillance Program NHMRC/ Melbourne Health Centre for Antimicrobial Stewardship European Centre for Disease Prevention and Control World Health Organization (WHO), World Health Day Campaign 2011 http://www.who.int/world-health-day/2011/en/index.html. References available at www.safetyandquality.gov.au/aaw2014 This presentation is intended to be used by health professionals, and reasonable care has been taken to ensure that the information is correct at the date of creation. It is intended to be used in its original version. The original version along with a complete list of references can be downloaded from the Commission web page: www.safetyandquality/aaw2014