TRANS*GENDER INCLUSIVE
HEALTH CARE
Challenges and Opportunities
Hello and Welcome
My name is Nicole Nisly
My pronouns are she, her and hers
I am a physician and my title is as below
Professor
of Internal Medicine
Co-Director of the LGBTQ Clinic at the University of
Iowa Health Care
Director of Complementary and Alternative Medicine
Clinic
Internal Medicine Diversity Officer
I am a Primary Care Physician
Is Trans*gender care medically
necessary?
AMA: “An established body of medical research
demonstrates the effectiveness and medical necessity of
mental health care, hormone therapy, and sex
reassignment surgery as forms of therapeutic treatment
for many people diagnosed with GID (gender identity
disorder)”
RESOLVED, That our American Medical Association
support public and private health insurance coverage
for treatment of gender identity disorder as
recommended by the patient’s physician. (AMA HOD
Resolution 122, 2008)
National Association of Social Workers
2008 Position Statement
“NASW supports the rights of all individuals to
receive health insurance and other health care
coverage without discrimination on the basis of
gender identity, and specifically without the
exclusion of services related to transgender or
transsexual transition, in order to receive medical
and mental health services through their PCP and
the appropriate referrals to medical specialists,
which may include hormone replacement therapy,
surgical interventions, prosthetic devices and other
medical procedures”
HHS Secretary K Sebelius LGBT Pride
Month Statement, 2013
Affordable Care Act (Obamacare) as of 2014;
No longer imposing life time dollar limit on healthcare
insurance coverage
Cannot deny coverage or impose higher rates because
someone is lesbian, gay, bisexual or transgender
Requires coverage for preventive health services including
HIV screening, contraception, intimate partner violence
screening at no out of pocket charge
New inclusive National Standards for Culturally and
Linguistically Appropriate Services
www.ThinkCulturalHealth.hhs.gov
On Health Disparities Experienced by
Gender Non Conforming Patients
Institute of Medicine Report, 2011
The Health of Lesbian, Gay, Bisexual, and
Transgender People: Building a foundation for
Better Understanding
Challenges posed by lack of adequate data, as few
surveys include gender identity questions
Barriers to accessing healthcare: personal and system
Increased risk of depression and suicide, STI, lack of
routine health care, suffer violence and bullying, lack
of social support
WPATH: Standards of Care
World Professional Association for Transgender Health
International, multidisciplinary professional organization
whose mission is to promote evidence-based care,
research, public policy…developing standards for best
practices
Standards of Care for the Health of Transsexual,
Transgender, and Gender Non Conforming People, 7th
edition, 2011
Recognized as authoritative guidelines and standards of
care by American Medical Association, American
Psychological Association, National Association of Social
Workers
www.wpath.org
In October of 2012 the new LGBTQ
clinic was launched
A bit of history and reasons why we created the
clinic, with the help from many here in this
audience: faculty, staff, students and community
members.
Dr Imborek and I met at the Transweek, organized
by the UI Trans* students and allies. The idea
came up as we heard their stories…
Let’s create an LGBTQ home, a safe and
welcoming space
The stories that inspired
Luna* is a 62 year old Trans* woman whose sex assigned at
birth was male. She was married for several years and has 2
daughters. Later in life she transitioned to her tru gender
identity as a Trans* woman. I am ready to complete a physical
and she says: “Doc, you are about to enter uncharted
territory”. What do you mean? I reply. “I have never had a full
physical including breast and pelvic exam since my transition
10 years ago”. I pause shocked and think: but you have
received care every 3 months here…But I say, well, today is the
day, get undressed and put on the gown dear and I will come
right back.
And then I tried to make an
appointment…
Jack* is a 22 year old Gender Non Conforming person
who identifies as Queer and who uses He/Him/His as
pronouns, he was a female as his sex assigned at birth.
He has been receiving testosterone for several months but
has been experiencing heavy vaginal bleeding. He tries to
make an appointment in two different areas at a Health
Center and is met with barriers, because of his gender
identity and finally needs to be seen at the ETC, where he
feels disregarded, is told that “we don’t know how to treat
people like you” and has his pronoun and preferred name
incorrectly used and disrespected.
Is this common? Sadly, yes…
LGBTQ individuals across their life spectrum are target of
discrimination, stigma, harassment and violence. They have a
higher risk of depression and suicide, homelessness, STI
including HIV and substance abuse than their heterosexual
peers. They have less access to health care and even when
access is available, they use the health system less frequently.
The health of LGBTQ patients is not well known and research is
particularly lacking on Transgender specific health needs.
The Health of Lesbian, Gay, Bisexual and Transgender People:
Building a Foundation for Better Understanding. Institute of
medicine, 2011
Providers for Trans*gender inclusive
care at the UIHC
LGBTQ clinic: provides primary care home for gender non
conforming patients, initiates hormone management,
generates appropriate surgical referrals and provides post
surgical follow up.
It was launched in October of 2012 to address a critical
need for safe and effective evidence-based care and care
coordination for gender non conforming patients.
Health provider education and training and research
initiatives are part of the mission for this program.
Team approach with Gynecology, Urology, Plastic Surgery,
Psychology and Family Counseling, Pharm D, Social Work.
Dermatology, others to come.
Early experience for UI LGBTQ clinic
New patients to UIHC seeking gender affirming care
Most are interested in hormone therapy care
Those interested in surgery are most interested in
surgical procedures widely utilized by many and
available at the UIHC:
Orchiectomy, TAH/BSO, Mastectomy (male chest wall reconstruction), Breast Augmentation
As need and volume grow, will expand to complete sex
change operations as needed, the UIHC has the expertise.
Gender Non conformity
Gender non conformity: expression of gender
characteristics, including identities, that are not
stereotypically associated with one’s assigned sex at
birth is a common and culturally diverse human
phenomenon that should not be judged as inherently
pathological or negative. (WPATH 2011)
Gender non conforming people may experience
minority stress from chronic experience of suffering
stigma, discrimination, prejudice, abuse, neglect,
violence, which may make people vulnerable to anxiety,
depression. (IOM 2001)
Gender non conforming people are not inherently
disordered.
Gender Dysphoria DSM-V
Discomfort and distress that is caused by a discrepancy
between a person’s gender identity and their sex
assigned at birth.
Treatment to assist people with such distress to explore
their gender identity is individualized. What helps one
person may not help another.
Gender dysphoria can in large be alleviated through
treatment.
A diagnosis of dysphoria should lead to evaluation and
treatment consideration
Unrecognized gender dysphoria may be diagnosed
when patients are seen for GAD, MDD, substance
abuse, etc
Issues of Cost Vs Benefits Analysis
Medical benefit: widely recognized. These are
medically necessary, life-saving treatments
Hidden cost of no treatment: suffering, mental health
costs, suicide risk, campus violence, work place
intolerance
Insurance coverage for City and County of SF:
30,000 employees
80,000 plan members
Estimated cost: 35 people per year accessing $50,000 in
services, per individual claim.
5 year utilization: 97 claims, total of $383,000
Opportunities
Education: physicians, residents and students, nurses,
social workers, counselors, lawyers, corrections
officers
Research: bridge the gap. Ideas: LGBTQ health
registry, Trans* folks in the corrections systems
Information dissemination: web site, publications,
lectures
Changing the system works towards eliminating
health disparities for sexual and gender minority
folks
How to support our LGBTQ patients:
EMR
Document on EMR: may use feature Epic FYI
Preferred name and Preferred pronoun should always be
documented and used in documentation, letters. May use
AKA: JOHN Doe, AKA Jane Doe. Our staff refers to patient
by preferred name.
Sex assigned at birth (legal sex for most people) vs gender
identity: there are many ramifications that require discussion
and evaluation for legally changing one’s legal sex.
Identify patient support system and refer to support groups,
counseling and family counseling as needed (see resource
list provided separately)
Identify patients at risk for bullying, violence, sex workers
and barriers to care
UIHC LGBTQ patients
Gender affirming care, including hormones, surgery,
voice therapy referrals through LGBTQ clinic at IRL:
319/467-2000. Iowa Care included.
Personnel training, creating a welcoming
environment: Our staff received Safe Zone Training.
Our web site provides information and useful links
for patients who identify as LGBTQ and their
families, in particular gender non conforming
people should be emphasized.
www.uihealthcare.org/lgbt/
Gender Non Conforming 101
Sex: Female, Male, Intersex
Genetically determined, based on physical characteristics
“sex assigned at birth”: health care providers and parents
name the sex
Gender: one’s self identified sex identity. It may be
incongruent with genetically determined sex.
Identified as Woman, Man, Trans* (gender non conforming)
Gender expression: one’s expression of maleness,
femaleness.
It is connected but independent of SEX and GENDER
identity.
Trans*
Man (transgender man, trans man)
Sex
Woman (transgender woman, trans woman)
Sex
assigned at birth female
assigned at birth male
Non Binary or Gender Queer
Does
not identify in the male or female gender binary
Gender
non conforming, gender fluid
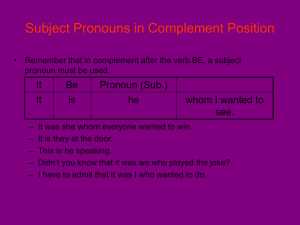
Pronouns
They identify your gender, who you are.
Because our society is binary when it comes to
gender, most people do not need to identify their
pronoun when meeting a new person, it is implied
Sometimes because of one’s gender expression, a
pronoun may need to be identified
Babies,
telephone, androgynous person
People that identify as Trans* commonly specify
their pronouns and name when greeting a new
person
Gender inclusive greeting
“Hello, my name is Dr Nisly, my pronouns are she, her
and hers. How may I call you and what is your
pronoun?”
Call patient by preferred name and pronoun of
reference
Sometimes patient’s pronouns are non commonly
recognized in the binary spectrum:
They, them, theirs
Zir, zir, zir
“I just met Syd and they were going to the library to pick up
their books”
Sexual orientation
Who I am attracted sexually to
Who I have sex with
A person may identify as gay and have never had sex
with someone of the same gender.
A person may identify as heterosexual or straight and
may occasionally have sex with someone of the same
gender.
For health risk evaluation, we ask: do you have sex with
man, women, Trans*, all the above or none.
A Trans* person identifying as gay or lesbian, will have
sex with someone of the same sex assigned at birth.
LGBTQ in the Corrections System
It is medically very important to address and treat
the person based on their gender identity for the
sake of their mental health and well being
It creates a safety challenge and safety always
comes first.
Examples of inclusive use of gender identity include
in personal meetings, medical or health care
appointments.
Housing should be based on safety for the gender
non conforming inmate and their peers.
Questions and Discussion
Deirdre (Donald)Nansen
McCloskey
Distinguished Professor
of Economics, History,
English, and
Communication
University of Illinois at
Chicago (formerly UI
Professor)
Professor of Economic
History,Gothenburg
University, Sweden