Psychoneuroimmunology
advertisement
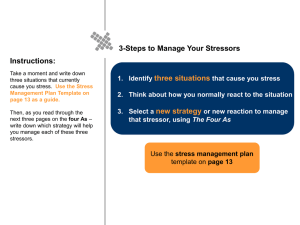
Psychoneuroimmunology Margaret E. Kemeny, Ph.D. Jason Satterfield, Ph.D. Stress and Coping Assessment: A Caregiver Case Example Objectives: -“Pull forward” stress & disease basics from MS1 - Illustrate clinically-relevant strategies to assess stress and coping prior to learning PNI basics Mark Simmons is a 62yo man who was diagnosed with Alzheimer’s Disease at the age of 58. Prior to that time he worked full time as a civil engineer. He and his wife Marsha (aged 56) live at home. Marsha works part-time at home as an accountant as well as serving as Mark’s primary care-giver. Both Mark and Marsha are your patients. Marsha has been having frequent URI’s and appears worn and fatigued. How Can Stress Cause Disease? What should trigger a stress and coping assessment? Signs of emotional distress, depression, or anxiety Multiple somatic complaints – insomnia, appetite, pain, fatigue Frequent colds, infections, slow healing times Stressor onset or change Stress Assessment Step 1: Ask about frequency “How often have you felt nervous or stressed out in the past month?” Step 2: Ask about cause (i.e. stressor) “What’s been causing you to feel stressed out?” Be sure to ask, “And is there anything else?” Frequency: “I feel stressed out nearly all the time. It’s just so hard for us right now.” Stressor 1: Caregiving, grief for husband Stressor 2: Ms. Simmons is worried about her own health. Stressor 3: Finances are worrisome but not at crisis point. Stress Assessment Step 3: Ask about duration “How long has this been going on?” Step 4: Ask about impact “How has this stress been affecting you?” Be sure to ask about both the social and occupational domains – “How has it affected your relationships? Your performance at work? Any other effects?” Stress Assessment Step 5: Ask about coping strategies “What have you been doing to cope with this stressful situation? How well has that been working for you?” Be sure to ask, “How can we help you get through this difficult time? What would be most helpful for me to do right now?” Duration: Mr. Simmons began having difficulties about 4-5 years ago. In the past year, the caregiving demands have been rapidly escalating. Ms. Simmons has been ill herself over the past 68 months. Their financial stress is just now starting. Impact: Ms. Simmons has trouble sleeping, fatigue, irritability, and frequent colds/URI’s. She neglects her health, avoids some of her friends, and had to cut way back on her accounting job. Coping strategies: She uses an in-home health aid 20hrs/wk. She watches TV late at night to relax. She keeps a journal when she has time. Stress Assessment Recap Be sure to ask about the 5 elements – Frequency – Cause – Duration – Impact – include social and occupational – Coping – the good, the bad, and how we can help Our Plan for Ms. Simmons? Schedule f/u appt for 1-2 wks to discuss adjunctive tx or stress management programs. Give her a depression screener to complete before next visit. Give referral to social work to arrange respite and assist with shared care scheduling. Give URL for local support group and ask her to consider joining. Will discuss next time. “Watchful waiting” re insomnia and other somatic sx possibly related to stress (no meds yet) How Can Stress Contribute to Disease? 1 2 Psychoneuroimmunology: Investigations of the bidirectional linkages between the CNS, the endocrine system and the immune system, and the clinical implications of these linkages. 3 STRESSOR NO MODERATING VARIABLES Genetic predisposition Previous life experiences Coping Social support Psychological Stress? YES HYPOTHALAMIC ACTIVATION CRH PITUITARY FACTORS ACTH SYMPATHETIC ACTIVATION Norepinephrine Medulla GLUCOCORTICOIDS Cortex Adrenal Glands IMMUNE SYSTEM EPINEPHRINE 4 Noradrenergic fibers innervate immune organs (lymph node, thymus, spleen, bone marrow) • Release NE in close proximity to immune cells (greater density in T cell areas) • Leukocytes express a and b adrenergic receptors • NE and E can influence leukocyte activity e.g., macrophage production of TNFa NE and epinephrine can alter lymphocyte migration: Immediate exposure (30 min) Longer exposure (days) # lymphocytes, natural killer cells # natural killer cells 5 6 NE can alter innate and adaptive immune function in organs and in circulation: – “Fine tunes” immune responses, allowing for quick adjustments (within minutes) – Shift from Th1 to Th2 7 STRESSOR NO MODERATING VARIABLES Genetic predisposition Previous life experiences Coping Social support Psychological Stress? YES HYPOTHALAMIC ACTIVATION CRH PITUITARY FACTORS ACTH SYMPATHETIC ACTIVATION Norepinephrine Medulla GLUCOCORTICOIDS Cortex Adrenal Glands IMMUNE SYSTEM EPINEPHRINE 8 Leukocytes express glucocorticoid receptors; cortisol acts on glucocorticoid receptors to have the following effects (as with synthetic GCs): inhibit lymphocyte proliferation inhibit production of pro-inflammatory cytokines Shift from Th1 to Th2 cell activity by stimulating synthesis of IL-10, IL-4 9 Definition of Stressors Stressors: environmental or internal demands which tax or exceed a person’s resources 10 Stressor Time Windows Immediate acute phase (within minutes of stressor onset); the “fight/flight” response Short-term stressors (that last for days or weeks) – Ex.: exams*, moving, being fired Chronic stressors (that last for months or years) – Ex.: caregiving for a family member with Alzheimer’s Disease, marital discord, poverty 11 Innate Immune System Mobilization in the Immediate Acute Phase of a Stressor (fight/flight): min to hrs post stressor onset Redistribution of immune cells (increase in leukocytes in blood) Increase in innate, non-specific immunity (increased NK cell activity) (Decrease in specific immunity) Alterations in Specific Immunity following Exposure to Short-term Stressors: days or weeks post stressor onset Decrease in Th1 cellular immune response (e.g., proliferative response of lymphocytes) Increase in Th2 humoral immunity (e.g., Th2 cytokine production) 12 13 Alterations in Non-specific and Specific Immunity following Exposure to Chronic Stressors: months to years post stressor onset Decrease in both Th1 cellular and Th2 humoral immune response (e.g., lower antibody titers to hepatitis B vaccines*) Decrease in innate, non-specific immune responses (except inflammatory activity) Persistent inflammatory activity (e.g., increased pro-inflammatory cytokine production) *antibody response can be enhanced with stress reduction intervention 14 Effects of Stress on the Immune System Depend not Only on Timing but Characteristics of the Person Immune effects are stronger in those who: – Are older – More depressed – Less supported Health behaviors (below) are affected by stress but immune effects of stress exposure are not due only to these effects. Drug use Alcohol Use Exercise Diet Medication adherence Sleep loss 15 16 Sympathetic Nervous System (SNS) mediation of immune effects of immediate acute phase of stressors (minutes to hours): the fight/flight response 17 SNS mediation of immune effects of immediate acute phase stressor—parachute jump 18 19 Figure 3 • NK cell # (CD16, CD56) and activity increased with jump •Effect abolished with badrenergic antagonist •NE levels correlated with NK cell # and function • Similar effects in studies of acute stressors in the laboratory •This and other studies show that NE is a critical mediator of the immune effects of the immediate fight/flight phase of the stress response 20 Hypothalamus CRH Anterior Pituitary ACTH Adrenal Cortex Cortisol Certain stressors can activate the HPA (more selective activation than ANS)-causing increased release of cortisol in blood, saliva an urine Stressors immediate-acute phase Short-term-days/weeks Chronic-months/years HPA appears to be an important mediator of effects of short-term and chronic stressors on the immune system Hypothalamus CRH Cortisol suppresses immune functions such as pro-inflammatory cytokine production via the glucocorticoid receptor (GCR). Anterior Pituitary ACTH Adrenal Cortex Cortisol GCR Immune Cell 21 22 Hypothalamus CRH Anterior Pituitary But stress-> INCREASES proinflammatory cytokine production One mechanism: Glucocorticoid Resistance: stress induced downregulation of GCR; cortisol cannot restrain pro-inflammatory cytokine production so cytokine production increases (animal/human studies) ACTH Adrenal Cortex Cortisol GCR Immune Cell 23 Glucocorticoid Resistance: Decreased ability for dexamethasone to suppress IL-6 production in vitro in chronically stressed individuals (parents of children with cancer) Miller et al., 2002 24 Are these stress-induced immunologic changes clinically significant? Do they contribute to disease onset or accelerate disease course? 25 Above: A 3.5-mm mucosal wound used to study delayed closure associated with stress and immune mechanisms of effect. 26 27 Healing time (as measured by response to hydrogen peroxide) is shown for each of the 11 subjects for the two time periods, summer vacation and examinations. Also high stress increased susceptibility to opportunistic bacterial infections in the wounds. 28 Mediators of Stress-related Changes in Wound Healing diminished mononuclear cell trafficking to the wound site reduced expression of cytokine, chemokine, growth factor genes decreased production of pro-inflammatory cytokines in wound environment* How Might Information From the Field of Psychoneuroimmunology Influence Your Clinical Practice? Ask about life stressors (short term and chronic), impact on functioning Ask about how a pt is coping, social supports. “Does it help?” Recognize that test results during chronically stressful times could be unreliable (repeat testing?) Recognize that vaccinations may be less protective during stressful times (consider other precautions) Recognize that wound healing may be influenced by stress Recognize that immune functions may be affected by the use of drugs that influence the ANS or glucocorticoids (e.g., bblockers). Ask about therapy and make recommendations and/or referrals as needed (know what is available in the community). recognize the limitations in knowledge when patients ask about whether a given therapy (visualization, etc) can improve their immune system. 29