Chapter 33 Assessment and Management of Patients With
advertisement

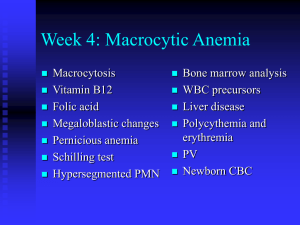
Assessment and Management of Patients With Hematologic Disorders Hematologic System • The blood and the blood forming sites, including the bone marrow and the reticuloendothelial system • Blood – Plasma – Blood cells • Hematopoiesis Blood Cells • Erythrocyte—RBC • Leukocyte—WBC – Neutrophil – Monocyte – Eosinophil – Basophil – Lymphocyte—T lymphocyte and B lymphocyte • Thrombocyte—platelet Hematopoiesis Anemias • Lower than normal hemoglobin and fewer than normal circulating erythrocytes. A sign of an underlying disorder • Hypoproliferative: defect in production of RBCs – Due to iron, vitamin B12, or folate deficiency, decreased erythropoietin production, cancer • Hemolytic: excess destruction of RBCs – Due to altered erythropoiesis, or other causes such as hypersplenism, drug-induced or autoimmune processes, mechanical heart valves • May also be due to blood loss Hematological Disorders • Hematological disorders • Anemia: a condition in which the Hb concentrations is less than normal, reflects the presence of fewer than normal RBCs within the circulation-O2 delivered to body tissue is diminished. Hematological Disorders • Three main categories for reasons of anemia • Loss of RBCs: occurs with bleeding-GI • Decreased production of RBCs: due to bone marrow suppression or deficiency of co-factors (folic acid, vit B12, Iron). • Increases destruction of RBCs: an overactive RES (reticuloendotheleal system): a special tissue macrophages that derived from monocytes, produced from the bone marrow, stay short time (24hrs) in the circulation and then inter into tissues and last for months differentiate into macrophage cells and function as foreign invaders and remove old and damaged cells from the circulation. • Or when an RBCs are abnormal and destroyed by the RES. Hematological Disorders • Anemia depends on the • The marrows’ ability to respond to the decreased RBCs. • The degree to which young RBCs proliferate in the bone marrow and the manner in which they mature • The presence of absence of end products RBCs destruction within the circulation (increase bilirubin, and hepatoglobin for example) Hematological Disorders • Classification of Anemia (table 33-3) • Anemia can be classified according to the physiological defect: • Defect in their production (hypoproliferative anemia) : # is less than normal due to bone marrow defect due to medications or chemicals or lack of factors important for RBCs production such as (iron, folic acid, erethropioten) • Destruction (hemolytic): premature destruction of RBCs. Results in tissue hypoxia, the released Hb is resulted in ↑billirubin concentration. RBCs destruction can results from abnormality in the RBCs such as Sickle cell anemia, glucose-6phosphate dehydrogenase deficiency, or within the plasma (immune hemolytic anemia) or direct injury to them. • Loss (bleeding) Hematological Disorders • Causes of hemolytic anemia • Inherited hemolytic anemia: abnormal hemoglobin, thalassemia, sickle cell anemia, RBCs membrane abnormalities • Acquired hemolytic anemia: – antibody related, iso-antibody/transfusion reaction – Autoimmune hemolytic anemia – Not-antibody related: RBCs membrane defects, liver disease, uremia, mechanical heart valve, bacterial parasitic, toxins Hematological Disorders • Manifestations of anemia depends on the speed and severity of it, duration of anemia, metabolic requirements of the individual, other concurrent disorder (cardiovascular). Special complications • The more rapid the more severe the symptoms • Patients who has anemia for a long time; Hb 911g/dl, develop no symptoms with slight tachycardia and exertion and fatigue; more active persons develop symptoms more than sedentary persons; hypothyroidism with less o2 needs may not develop symptoms. Hematological Disorders • Diagnostic findings • Hb, Hct, reticulocyte count, RBCs, and mean corpuscular volume (MCV). • Serum iron level, total- iron binding capacity (TIBC), serum vit B12, folate level • Bone marrow aspiration • Other dx is useful to determine if the anemia is separated problem or as a result of other disease such as cancer, malignancies, loss or ulcer in the GI tract Hematological Disorders • Complications • Heart failure, confusion, parasthesias, angina symptoms. Management is aimed to correct the cause, if severe RBCs can be given through transfusion Hematological Disorders • Assessment • Patient his, fatigue, malaise, pallor of skin and mucus membrane (sclera, oral mucosa) • Family his • Jaundice of hemolytic • Medication his (medication can suppress bone marrow). • Nutritional assessment: iron, folate, B12, • Cardiac assessment: heart try to compensate harder and faster in anemia (tachycardia, palpitations, dyspnea, dizziness, orthopnea, heart failure may develop evidenced by cardiomegalloy or hepatomegally and peripheral edema) • Assess GI for blood loss. FOBT. • Neurological assessment: peripheral numbness, ataxia, poor coordination, confusion. Hematological Disorders • Nursing diagnosis • Activity intolerance related to weakness, fatigue • Imbalanced nutrition, less than body requirements, related to inadquate intake of essential nutrients • Ineffective tissue perfusion related to inadequate blood volume or hematocrit • Noncompliance with prescribed therapy Hematological Disorders • Nursing interventions • Managing fatigue: balance between activity and rest • Maintaining adequate nutrition • Maintaining adequate perfusion • Promoting compliance with prescribed therapy Hematological Disorders • Hypoproliferative anemias: iron deficiency anemia • Results when dietary intake of iron inadequate for Hb synthesis; the body store only one fourth or one third of its iron • more than 500 million people develop it, most common type of anemia Hematological Disorders • The most common cause of IDA in men and postmanepaused women is bleeding (ulcers, gastritis, GI tumor, inflammatory bowel disease); pregnant women not taking iron supplement; heavy menstrual bleeding • Chronic alcoholism Hematological Disorders • Symptoms • Smooth and sore tongue • brittle and ridged nails, angular cheilosis (ulceration at the corner at the mouth) • Multiple pregnancy and GI bleeding and Pica (a craving for unusual substances ice, clay) Hematological Disorders • Diagnostic findings • Bone marrow aspiration is the most efficient • Diminished iron store cause small RBCs, MCV that measures the size of RBCs. • Low ↓ferritin level which reflects low iron stores.↓ Hb level Hematological Disorders • Investigate for intestinal cancer or of uterine fibroid tumors, polyps, ulceration, through endoscopy, stool specimen, X-ray, colonoscopy. • Administer oral iron-ferrus sulfate, ferrus gluconate, and ferrus fumarate. • It may take longer so patient must be advised to take iron for as long as 6-12 months. Hematological Disorders • If iron supp is poorly tolerated then patient need large amounts. Then it should be administer through IV or IM injection. Check for allergic reaction with small dose for the first 30 minute then administer the rest of the iron. Hematological Disorders • Nursing management • Nutritional counseling: Food source high in iron (beef or calf’s liver, chicken liver). Other meats, beans (blacks, garbanzo), leafy green vegetables, raisins, and molasses. Take all food rich in iron. • If patient take medication advise him/her to take it before meal; Iron best absorbed on an empty stomach. If it caused some distress take it with meal. Do not take antiacids with it sense it dec its absorption • Iron supp may have adverse effect on GI: nausea, vomiting, cramping. Some supp may be taken with stool softners. • If liquids: it may cause stain so take it with straw and rinse the teeth after taking it. Hematological Disorders • Instruct patient that it may cause dark stool or dark green. • IM may cause some local pain or stain of skin; avoid extra rubbing to the place and use Ztrack technique Hematological Disorders • Aplastic anemia: caused by damage or decrease in marrow stem cells, damage to the microenvironment of the marrow or replacement of the marrow with fat results in markedly marrow aplasia (↓hematopoiesis). thrompocytopnea may be also seen with it. Hematological Disorders • Idiopathic (unknown cause) or can be congenital or acquired and triggered by pregnancy or certain medications. Benzene or benzene derivative (airplane glue), toxins like pesticides. • Manifestation: pallor, fatigue, dyspnea, infection (chest, lymphadenopathy), Purpura (bruising) Hematological Disorders • Assessment and Dx • Review medication his: since toxins and some medication may be the cause • Bone marrow aspirate may show hypoplastic or aplastic (very few to no cells), marrow can be replaced with fat. Hematological Disorders • Medical management • Bone marrow transplantation if there is a donor and young people. • Peripheral blood stem cell transplantation • Immunosuppressive therapy to prevent the lymphocyte from destroying the stem cells. • Transfusion of RBCs and platelets as necessary. • Nurses should monitor infection and bleeding which may cause death in aplastic anemia • Hematological Disorders Megalosplastic Anemia • ↓ of vit B12 or folic acid, identical bone marrow or peripheral blood changes occur because both vits are essential for DNA synthesis. • Results in production of large RBCs called megaloplastic • Bone marrow analysis shows hyperplasia: abnormal ↑ in the # of cells and the precursor erythroid and myeloid cells are large and bizzare in appearance. RBCs can be destroyed at the marrow or they leave the marrow mature but very few in #. • Hb can be 4 to 5 g/dl. WBC count 2000-3000/mm³ and the platelets less than 50,000/mm³. RBCs, platelets are abnormal large and bizzare shape, MCV is high > 110μm³. Hematological Disorders • Pathophysiology • 1-Folic acid deficiency • Folate storage in the body are small and deplete quickly in 4 months • Folic acid is found in uncooked green vegetables • This anemia can be found in people with male-absoprtion diseases Hematological Disorders • 2-Vit B12 deficiency • The body has large stores of B12 so anemia may not be apparent in years • In strict vegetarians • Crohns’ disease with less absorption in the GI; abnormality in the gastric mucosa or stomach wall atrophy, and fails to excrete intrinsic factors (secreted from the cells in the gastric mucosa and bind with B12 to be absorbed) this called pernicious anemia. Hematological Disorders • Clinical manifestations in both types of anemia are similar; in B12 anemia there are some neurological symptoms. Therefore, serum level of both Vit B12 and folate must be measured. • Manifestations of anemia appear very slowly (weakness, fatigue, lethargy, restlessness). • Very pale, smooth sore tongue, mild diarrhea, confused numbness in the extremities, loss of position sensation, difficulty maintaining their balance due to spine damage. • May last several year if not treated and eventually death may happened due heart failure because of anemia. Hematological Disorders • Assessment and diagnostic findings • Schilling test for vit B12 deficiency: small radioactive oral B12 is administered and followed in few hours with nonradioactive paranteral dose of B12. if the oral B12 is absorbed; then more than 8% of it will be excreted in the urine; if no radioactive is present in the urine then the vit b12 stays in the GI; then the cause is GI malabsorption of vit b12. • Therefore, If readioactive present in the urine it means the cause of anemia is not pernicious anemeia or ileal disease. • The intrinsic factor antibody test: + indicate the presence of antibodies that bind with B12 and prevent it from binding to receptors in the ileum and thus preventing its absorption Hematological Disorders • Medical management • Folate deficiency can be treated with folic acid in the diet and administer 1 mg of it daily orally or IM (if not tolerated orally). • Vit B12 treated with B12 replacement; with orally vit or fortified soy milk. Nurses should assess signs and symptoms Pay attention to ambulation, safety, coordination, and asses patient gait and stability and the need for assistive devise. Since mouth and tongue sores are present encourage family to have small, soft frequent meals. Teaching about follow up and screening and severity of the disease Hematological Disorders • Hemolytic anemia: short life span for the RBCs, ↓O2 and hypoxia and %80 of the heme is converted to bilirubin conjugate in the liver and converted to bile. Hematological Disorders • Sickle cell anemia severe hemolytic anemia results from sickle hemoglobin gene. • RBCs containing HBS usually are round, very pliable, biconcave disk shape and becomes deformed, rigid and sickle shaped. • It results in ischemia and infarction, patient may have pain, swelling and edema, or may adhere to each others and make occlusion of arterioles. • Can be in different shapes: carrier-sickle cell hemoglobin C (SC) less sever; Sickle cell hemoglobin D (SD) and sickle cell beta-thallassemia. Persons with trait or carrier should not get married, more likely to have children with two abnormal genes. Hematological Disorders • Clinical manifestations • Always anemic Hb 7-10 g/dl • Jaundice, because bone marrow try to compensate the bones may become enlarge face and skull. • Chronic: tachycardia, murmur, cardiomegally in adults dysarythmias and heart failure. Hypoxic damage of vital organs, infection, renal failure, pulmonary hypertension • Complications: infection, stroke, renal failure, impotence, heart failure, CVA, skin ulcers, eye: scarring, hemorrhage, retinal detachment, blindness. Hematological Disorders • Sickle cell crisis occurs in three types: • Very painful crisis due to hypoxia and necrosis • Aplastic crisis: infection with human parvovirus, Hb falls rapidly and bone marrow cannot compensate • Sequestration crisis: when organ pool the sickle cells; in children spleen infarction and no longer functioning; in adults liver and lungs. • The SCA can diagnosed in childhood; infants become anemic and have crisis at year 1 or 2 then they may die at the 1 year of life. Can manage to 42 years old and can cure in the 30s of age…depends on the severity of it Hematological Disorders • Medical management • BMT: few people may have due to incompatible donors or the severe organs damage already • Pharmacological therapy: hydroxyurea (hydrea): chemotherapy; decrease the permanent formation of sickled cells. They decrease the painful crisis in, have lower incidence of acute chest syndrome and less need for blood • Side effects: chronic suppression of WBC formation, and later development of malignancy, patients may develop liver toxicity at low dose Hematological Disorders • Transfusion therapy: essential to prevent complications of SCA. 90% reduction of stroke in children. • Risks include: iron overload, poor venous access; infection (Hebatitis); and all oimmunization from the repeated transfusion, increase concentration of Hb Need very close observation specially for hemolytic reaction because with repeated transfusion patient develop autoantibodies which made the cross matching difficult • Daily folic acid replacement; antibiotic to treat infection the major cause of death; to decrease chest infection: antibiotic and spirometer; bronchoscopy; corticosteriod, Hematological Disorders • Supportive therapy: pain management is essential; pain can last hours to days and vary from one to another. Aspirin, NSAID. • Support groups: physical and occupational therapy D5W • Adequate hydration and O2 therapy Hematological Disorders • • • • • Nursing process for patient with SCA. Assess pain. Assess of body system for signs of hypoxia assess resp system, neurological system signs of infections and Lab test for HB and HCT + previous medical history or bld transfusion hist Hematological Disorders • Possible nursing Dx • Acute pain related to tissue hypoxia due to aggultination of sickle cells within the body vessels • Risk for infection • Risk for powerlessness related to illness induced helplessness • Deficient knowledge regarding sickle cells prevention Hematological Disorders • Nursing interventions are aim to • Manage pain • Prevent and treat infection: if oral complete the entire course • Promoting coping skills: stamina and positive self esteem; , trust. • Increase knowledge: maintain adequate hydration to prevent the severity and occurrence of the attack Blood & Blood components Therapy • Blood unit is 450 ml; can be separated into RBCs, platelets, plasma (can be separated into albumin, immune globulin, factor VIII, Factor IX). • RBCs should be stored at 4 C and stored safely for up to 42 days • Platelets should be stored at room temp and last only for 5days; and plasma should be immediately frozen to maintain activity of clotting factors and last for 1 year, frozen Blood & Blood components Therapy • Blood donation • To protect both the recipient and the donor you should review the following types of history • Viral hepatitis, infusion or transfusion of any blood derivative, untreated syphilis or malaria, drug abuse, HIV, skin infection, asthma, urticaria, pregnancy, tooth extraction within 72 hours, exposure to infectious disease, recent immunization, tattoo, cancer and blood donation • Body weight should exceed 50 Kg, > 17 yrs old not qualified, stable VS, HB 12.5 g/dl women and men 13.5 g/dl Blood & Blood components Therapy • • • • • • • Administering blood and blood components (RBCs) Review the order Review institutional policy. consent form Explain the procedure Take VS Instruct patient about signs of reaction to blood components (itching, hives, swelling, SOB, fever, chills, flushing). • Use 2o-gauge needle or larger for placement in large vein. • Review institutional policy after the IV line is started • Double check on the ABO and Rh type, check patient name and label. Blood & Blood components Therapy The procedure • Obtain the blood from the blood bank after starting the IV line. • Double check on Dr.order and patient name and labels • Initiate the transfusion within 30 min • In the first 15 min start slowly no faster than 5 mL/min if no signs of adverse effect increase the rate • Check closely for 15-30 min any signs for reaction and vital signs, infusion time not more than 4 hours because of increasing bacterial proliferation • Observe signs of adverse reaction: circulatory overload, sepsis, febrile reaction, allergic reaction, acute hemolytic reaction • Change blood tubing every 2 units transfused Blood & Blood components Therapy • After the procedure • Obtain vital signs and compare baseline measurement • Dispose materials carefully • Document the procedure • Monitor patient response to and effectiveness of the procedure • Alert • Never add medication to blood or blood products. • Blood should be warmed • If blood is too thick to run freely you can add normal saline to the unit. • Administering platelets or fresh frozen plasma (FFP) • Same procedure with some differences • Check patients, labels, dr. order, policy, consent form, explain procedure, use 22gauge needle, take VS. • The procedure • Double check on everything related to administration • Obtain the platelets and FFP from the blood bank only after the IV line started • Check the blood unit for any abnormal color clumps (excessive red may indicate it is contaminated with larger amount of RBCs) • Infuse as fast as patient tolerate to prevent plantlets clumping during administration • Observe for transfusion reaction (hives, back pain, SOB, restless, • Flush line with saline after transfusion • • • • • After the procedure Obtain VS Dispose the used material appropriately Record and document the procedure Monitor patient for effectiveness of the therapy, platelets count can be obtained after 1 hr of transfusion • Alert: FFP does not require necessarily the RH compatibility, only ABO compatibility; platelets are not typically matched for ABO. •