ODYSSEY FH I and FH II studies
advertisement

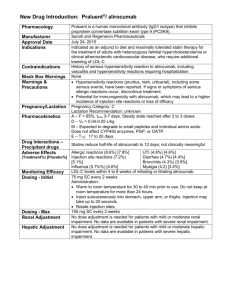
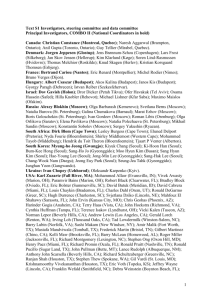
Efficacy and safety of alirocumab in patients with heterozygous familial hypercholesterolaemia (heFH) not adequately controlled with current lipidlowering therapy: Results of ODYSSEY FH I and FH II studies John J.P. Kastelein,1 Henry N. Ginsberg,2 Gisle Langslet,3 G. Kees Hovingh,1 Richard Ceska,4 Robert Dufour,5 Dirk Blom,6 Fernando Civeira,7 Michel Krempf,8 Michel Farnier9 1Department of Vascular Medicine, Academic Medical Center, University of Amsterdam, Amsterdam, The Netherlands; 2Columbia University, New York, NY, USA; 3Lipid Clinic, Oslo University Hospital, Oslo, Norway; 4Center of Preventive Cardiology, 1st School of Medicine and University Hospital, Charles University, Prague, Czech Republic; 5Institut de Recherches Cliniques de Montréal, Montreal, Canada; 6Division of Lipidology, Department of Medicine, University of Cape Town and MRC Cape Heart Group, Cape Town, South Africa; 7Lipid Unit, Hospital Universitario Miguel Servet, Zaragoza, Spain; 8CHU de Nantes - Hȏpital Nord Laennec, Saint-Herblain, France; 9Point Médical, Dijon, France 1 Industry Relationships and Institutional Affiliations 2 Author Disclosure John J.P. Kastelein Consultant/honoraria for Regeneron, Sanofi, Eli Lilly, Pfizer, Amgen, Isis, Genzyme, Aegerion and Esperion Henry N. Ginsberg Research support from Genzyme (Sanofi) and Sanofi-Regeneron, is a consultant on an advisory board for Sanofi and Regeneron and is or has been a consultant for Amarin, Amgen, AstraZeneca, BristolMyersSquibb, GlaxoSmithKline, ISIS, Kowa, Merck, Novartis, and Pfizer Gisle Langslet Advisory board fees from Amgen, Sanofi-Aventis and Janssen Pharmaceuticals G. Kees Hovingh KHs institution has received payment for conducting clinical trials from Sanofi, Regeneron, Amgen, Pfizer, Kowa, Genzyme, ISIS, Genzyme, Roche, Ely Lilly, Aegerion, Synageva, AstraZeneca and for lectures and/or advisory panel participation of KH from Amgen, Sanofi, Pfizer and Roche Richard Ceska Consultant/honoraria for Regeneron, Sanofi, Amgen, Genzyme, Aegerion, Kowa Robert Dufour Received consultancy fees from Sanofi Dirk Blom Consultant or on an advisory panel for Aegerion, Amgen, AstraZeneca, MSD, and Sanofi Aventis. DB’s institution has received payment for conducting clinical trials from Aegerion, Amgen, Eli Lilly, Novartis, and Sanofi/Regeneron; DB has participated in a lecture/speaker’s bureau or received honoraria from Aegerion, Amgen, AstraZeneca, MSD, Pfizer, Sanofi Aventis, Servier, and Unilever Fernando Civeira Grants, consulting fees and/or honoraria from Amgen, Merck, Pfizer and Sanofi Aventis Michel Krempf Grants, consulting fees and/or honoraria and delivering lectures for Abbott, Amgen, Astra Zeneca, BMS, Merck and Co, Novartis, Pfizer, Roche, Sanofi-Aventis Michel Farnier Grants, consulting fees and/or honoraria and delivering lectures for Abbott, Amgen, BoehringerIngelheim, Genzyme, Kowa, Merck and Co, Novartis, Pfizer, Recordati, Roche, Sanofi-Aventis, and SMB Heterozygous Familial Hypercholesterolaemia (heFH) HeFH is one of the most common genetic diseases (prevalence 1/200 to 1/500) characterised by: – extremely high levels of low-density lipoprotein cholesterol (LDL-C)1 – premature atherosclerosis and cardiovascular disease (CVD)1 A large proportion (~80%) of adult patients with heFH on lipid-lowering treatment do not reach the LDL-C goal of <2.5 mmol/L (100 mg/dL)2 The treatment goal for adult patients with heFH who also have coronary heart disease or diabetes is <1.8 mmol/L (70 mg/dL)1 1. Nordestgaard BG et al. Eur Heart J. 2013;34:3478–90 2. Pijlman AH et al. Atherosclerosis. 2010;209(1):189-194. 3 ODYSSEY FH I and FH II Study Design Double-Blind Treatment Period (78 Weeks) Alirocumab 75 mg Q2W SC with potential ↑ to 150 mg Q2W SC HeFH patients on max tolerated statin ± other lipidlowering therapy n=323 (FH I); n=167 (FH II) LDL-C ≥1.81 mmol/L [70 mg/dL] (history of CVD) or 2.59 mmol/L [100 mg/dL] (no history of CVD) Assessments Per-protocol dose ↑ possible based on pre-specified LDL-C level R n=163 (FH I); n=82 (FH II) Placebo Q2W SC W0 W8 W4 W16 W12 Dose ↑ if LDL-C >70 mg/dL at W8 W36 W24 Primary efficacy endpoint W64 W52 W78 Pre-specified analysis Efficacy: All Patients To W52 Safety: Baseline-W78 (all patients at least W52) Clinicaltrials.gov identifiers: ODYSSEY FH I: NCT01623115; ODYSSEY FH II: NCT01709500. 4 OLE/8 week FU (single 1-mL injection using prefilled pen for self-administration) Baseline Characteristics FH I FH II All patients on background of max-tolerated statin ± other lipid-lowering therapy Alirocumab (N=323) Placebo (N=163) Alirocumab (N=167) Placebo (N=82) Diagnosis of heFH†, % (n) Genotyping Clinical criteria 39.9% (129) 59.8% (193)‡ 38.0% (62) 62.0% (101) 70.1% (117) 29.9% (50) 81.7% (67) 18.3% (15) 52.1 (12.9) 51.7 (12.3) 53.2 (12.9) 53.2 (12.5) Male, % (n) 55.7% (180) 57.7% (94) 51.5% (86) 54.9% (45) Race, white, % (n) 92.9% (300) 88.3% (144) 98.2% (164) 97.6% (80) 29.0 (4.6) 30.0 (5.4) 28.6 (4.6) 27.7 (4.7) CHD history, % (n) 45.5% (147) 47.9% (78) 34.1% (57) 37.8% (31) Current smoker, % (n) 12.1% (39) 18.4% (30) 21.6% (36) 15.9% (13) Hypertension, % (n) 43.0% (139) 43.6% (71) 34.1% (57) 29.3% (24) 9.6% (31) 15.3% (25) 4.2% (7) 3.7% (3) Age, years, mean (SD) BMI, kg/m2, mean (SD) Type 2 diabetes, % (n) †Diagnosis of heFH must be made either by genotyping or by clinical criteria. For those patients not genotyped, the clinical diagnosis may be based on either the Simon Broome criteria for definite FH or the WHO/Dutch Lipid Network criteria with a score of >8 points. ‡In FH I, one patient was categorised as “probable” FH by clinical criteria – genotyping results for this patient are pending. Lipid Medication and LDL-C at Baseline All patients on background of max-tolerated statin ± other lipid-lowering therapy FH I FH II Alirocumab (N=323) Placebo (N=163) Alirocumab (N=167) Placebo (N=82) 100% 100% 100% 100% High-intensity statin‡, % (n) 80.8% (261) 82.8% (135) 86.2% (144) 87.8% (72) Ezetimibe, % (n) 55.7% (180) 59.5% (97) 67.1% (112) 64.6% (53) 3.7 (1.3) [144.7 (51.2)] 3.7 (1.2) [144.4 (46.8)] 3.5 (1.1) [134.6 (41.3)] 3.5 (1.1) [134.0 (41.6)] Any statin†, % (n) LDL-C, mean (SD), mmol/L [mg/dL] †Patients should receive either rosuvastatin 20-40 mg, atorvastatin 40-80 mg daily, or simvastatin 80 mg daily unless not tolerated and/or appropriate other dose given according to the judgement of the investigator. ‡High-intensity statin: atorvastatin 40-80 mg or rosuvastatin 20-40 mg daily. 6 Alirocumab Significantly Reduced LDL-C from Baseline to Week 24 versus Placebo Primary Endpoint: Percent Change from Baseline to Week 24 in LDL-C LS mean (SE) % change from baseline to Week 24 All patients on background max-tolerated statin ±other lipid-lowering therapy 7 FH I 20 9.1% Alirocumab FH II 10 Placebo 2.8% 0 -10 N=322 -20 N=163 N=166 43.4% had dose increase at W12 -30 -40 N=81 38.6% had dose increase at W12 -50 -48.7% -48.8% -60 LS mean difference (SE) vs. placebo: Intent-to-treat (ITT) Analysis −57.9% (2.7) P<0.0001 −51.4% (3.4) P<0.0001 Alirocumab Maintained Consistent LDL-C Reductions Over 52 Weeks Achieved LDL-C Over Time on Background of Maximally-Tolerated Statin ±Other LLT FH I Placebo: FH I Alirocumab: FH II FH II 4.0 mmol/L 4.0 mmol/L 4 155 3,5 3.7 mmol/L 3.5 mmol/L 3 135 116 2,5 97 1.9 mmol/L 1.8 mmol/L 77 2 1,5 1.8 mmol/L 1.7 mmol/L 58 39 1 0 4 8 12 16 20 Dose ↑ if LDL-C >70 mg/dL at W8 8 174 24 28 Week 32 36 40 44 48 52 Intent-to-treat (ITT) Analysis LLT = lipid-lowering therapy mg/dL LDL-C, LS mean (SE), mmol/L 4,5 Most heFH Patients Receiving Alirocumab on Background Statin Other LLT Achieved LDL-C Goals Proportion of patients reaching LDL-C goal† at Week 24 FH I 90 FH II 81.4% 80 Alirocumab 72.2% 70 % patients Placebo 60 50 40 30 20 11.3% 10 2.4% 0 P<0.0001 †Very 9 high-risk: <1.81 mmol/L (70 mg/dL); high-risk: <2.59 mmol/L (100 mg/dL). LLT = lipid-lowering therapy. Intent-to-treat (ITT) Analysis Safety Analysis (Pooled Data from FH I and FH II) All Data Collected Until Last Patient Visit at Week 52 % (n) of patients All patients on background of max tolerated statin ± other lipid-lowering therapy Alirocumab (N=489) Placebo (N=244) TEAEs 74.8% (366) 75.4% (184) Treatment-emergent SAEs 10.0% (49) 9.0% (22) TEAEs leading to death 0.8% (4) 0 TEAEs leading to discontinuation 3.1% (15) 3.7% (9) Adverse Events of Interest Adjudicated CV events† 1.6% (8) 1.2% (3) Injection-site reactions 11.5% (56) 9.0% (22) 0.2% (1) 1.2% (3) ALT >3 x ULN 2.1% (10/488) 1.2% (3/244) Creatine kinase >3 x ULN 3.5% (17/483) 6.2% (15/243) Neurocognitive disorders 4 TEAE-related deaths were all in alirocumab arm, 2 due to metastatic cancer (non-small cell lung and pancreatic), 2 due to MI (1 acute, 1 sudden cardiac death) †Adjudicated 10 CV events include all CV AEs positively adjudicated. The adjudication categories are the following: CHD death, non-fatal MI, fatal and non-fatal ischaemic stroke, unstable angina requiring hospitalisation, congestive heart failure requiring hospitalisation, ischaemia-driven revascularisation procedure (PCI, CABG). Statistical analyses have not been performed. Safety Analysis TEAEs Occurring in ≥5% of Either Alirocumab or Placebo Patients Collected Until Last Patient Visit at Week 52 (Pooled Data from FH I and FH II) % (n) of patients All patients on background of max tolerated statin ± other lipid-lowering therapy 11 Alirocumab (N=489) Placebo (N=244) Injection-site reaction 11.5% (56) 9.0% (22) Nasopharyngitis 10.2% (50) 11.1% (27) Influenza 8.8% (43) 6.1% (15) Headache 5.5% (27) 6.6% (16) Statistical analyses have not been performed. Conclusions In heFH patients not well controlled on maximallytolerated statin ± other lipid-lowering therapy: – Self-administered alirocumab produced significantly greater LDL-C ↓ vs. placebo at W24 (LS mean difference of 51.4-57.9%) – Majority of pts (>70%) achieved their LDL-C goals at W24 – Mean achieved LDL-C levels of 1.7-1.9 mmol/L (65.9-74.3 mg/dL) at W52 with alirocumab – ~50% did not require a dose ↑ to alirocumab 150 mg Q2W – Safety and tolerability were generally comparable in alirocumab and placebo groups 12 Thank you to all principal investigators and national coordinators! Norway: 1 site Canada: 5 sites Denmark: 3 sites Sweden: 2 sites Netherlands: 8 sites Austria: 3 sites 13 sites UK: 4 sites USA: 23 sites 1 site Spain: 9 sites Russia: 10 sites 2 sites Czech Republic: 4 sites 6 sites France: 4 sites Israel: 4 sites South Africa: 9 sites FHI ‒ 89 sites worldwide FHII – 26 sites worldwide 13