Gary Humble, Senior Associate
OPEN MINDS
April 18, 2013
Updates On
Health Care
Reform
Nationally and
in Washington
State
OPEN MINDS © 2013. All rights reserved.
2
1.
2.
3.
4.
5.
6.
7.
Medicaid expansion
Employer mandate implementation
Individual mandate implementation
Health insurance exchanges
Essential health benefit requirement
Medical loss ratio requirements
End of disproportionate share payments to
hospitals
OPEN MINDS © 2013. All rights reserved.
3
The Medicaid expansion provision of PPACA extends
Medicaid eligibility to all Americans who earn less
than 133% of the poverty level (approximately
$14,000 for an individual and $29,000 for a family
of four)
New rules go into effect on January 1, 2014
OPEN MINDS © 2013. All rights reserved.
4
Adoption of Medicaid expansion provision of PPACA, by state,
as of January 17, 2013
Committed to
expand coverage
• Arizona, California, Colorado, Connecticut, Delaware,
Hawaii, Illinois, Maryland, Massachusetts, Minnesota,
Michigan, Nevada, New Jersey, New Mexico, New York,
Ohio, Oregon, Rhode Island, Vermont, Washington,
Washington D.C.
Declined to
expand coverage
• Alabama, Georgia, Iowa, Louisiana, Maine, Mississippi,
North Carolina, Oklahoma, Pennsylvania, South
Carolina, South Dakota, Texas, Wisconsin, Wyoming
Undecided
• Alaska, Arkansas, Florida, Idaho, Indiana, Kansas,
Kentucky, Missouri, Montana, Nebraska, New
Hampshire, North Dakota, Tennessee, Utah, Virginia,
West Virginia
OPEN MINDS © 2013. All rights reserved.
5
Effective January 1, 2014
Medicaid will be expanded to include individuals between the
ages of 19 up to 65 (parents, and adults without dependent
children) with incomes up to 138% FPL
Anticipate enrolling up to new 254,000 participants in next few
years
OPEN MINDS © 2013. All rights reserved.
6
•
•
•
•
Forecasted to save $142 million in State
funding in the next State Bi-annual budget
Will bring in an additional $1.2 billion in
federal funds to the State
Create 10,282 jobs (direct or indirect) as a
result of Medicaid Expansion
Savings for Businesses- Reducing Cost
Shifting of uncompensated care in their
insurance premiums
OPEN MINDS © 2013. All rights reserved.
7
Employers must provide health care coverage for employees or pay a
tax penalty
Employers with at least 50 FTE must provide health care coverage that
meets requirements and provides the “essential health benefits
package”
Tax credit incentives are currently in place for small business (less than
25 employees) offering health insurance
Tax penalties of $2,000 for each FTE, beyond the company’s first 30
workers, begin in 2014
OPEN MINDS © 2013. All rights reserved.
8
Individuals are required to purchase health insurance or pay a “tax”
of $695 or 2.5% of income, whichever is higher
Individuals must purchase health insurance if the monthly premium
is less than 8% of their monthly income
Individual penalties will go into effect in 2016
OPEN MINDS © 2013. All rights reserved.
9
System in which individuals can compare and purchase
health insurance policies with baseline levels of coverage
State options include state-run exchange, federal/state
partnership exchange, and federal-run exchange
States will begin open
enrollment October 2013
Federal grants available
for states through the end
of 2014
Exchanges must be selffunding starting in 2015
OPEN MINDS © 2013. All rights reserved.
10
Application Status Of Health Insurance Exchange, By State,
As Of December 14, 2012
State run (19)
• California, Colorado, Connecticut, Hawaii, Idaho,
Kentucky, Massachusetts, Maryland, Minnesota,
Mississippi, Nevada, New Mexico, New York, Oregon,
Rhode Island, Vermont, Utah, Washington, Washington
D.C.
State-federal
partnership (6)
• Arkansas, Delaware, Illinois, Iowa, North Carolina, West
Virginia
Will not operate
own exchange (23)
• Alabama, Alaska, Arizona, Georgia, Indiana, Kansas,
Louisiana, Maine, Missouri, Montana, Nebraska, New
Hampshire, New Jersey, Ohio, Oklahoma, Pennsylvania,
South Carolina, South Dakota, Tennessee, Texas,
Virginia, Wisconsin, Wyoming
Undecided (3)
• Florida, Michigan, North Dakota
OPEN MINDS © 2013. All rights reserved.
11
•
•
•
•
State of Washington will operate their own
Health Insurance Exchange
The Insurance Exchange could serve as
many as 400,000 Washington residents
The Washington State Health Care Authority
(HCA) will oversee the development of the
Insurance Exchange
Enrollment begins in October, 2013 for a
January 1, 2014 effective date
OPEN MINDS © 2013. All rights reserved.
12
The name of the
Washington Insurance
Exchange is Health Plan
Finder
Received 24 letters of
Interest from health and
dental insurance carriers to
participate in State’s online
health insurance exchange
Interested plans include
Regence BlueCross
BlueShield of Oregon, Group
Health Cooperative, Kaiser,
Molina Health Plan
OPEN MINDS © 2013. All rights reserved.
13
Essential Health Benefits Categories
1. Ambulatory patient services
2. Emergency services
3. Hospitalization
“Essential health benefits”
determined by each state – going
live with HIE @October 2013
4. Maternity and newborn care
5. Mental health and substance use disorder services, including behavioral
health treatment
6. Prescription drugs
7. Rehabilitative and habilitative services and devices
8. Laboratory services
9. Preventive and wellness and chronic disease management
10. Pediatric services, including vision and oral care
OPEN MINDS © 2013. All rights reserved.
14
•
Law Enacted in 2012
◦ Specifies selection of the largest small group plan
as the benchmark for establishing essential health
benefits
◦ Regulations require every plan to cover a list of 10
“essential” benefits
◦ Standardized coverage levels: “bronze” coverage;
“silver” coverage; 80 “gold” coverage; “platinum”
coverage
◦ For those under Age 30, preventive/catastrophic
coverage with a high deductible
OPEN MINDS © 2013. All rights reserved.
15
Medical Loss Ratio is the percentage of premiums that the health
insurance plan uses to reimburse providers
Plans that fail to meet the minimum must rebate the difference back
to consumers
MLR standards:
1. Health plans in large group markets must spend at least 85% of premiums
2. Health plans in the individual and small group markets must spend at least
80% of premiums
MLR requirements were effective January 1, 2012
OPEN MINDS © 2013. All rights reserved.
16
Disproportionate share: Federal funds to hospitals for indigent care
Medicaid disproportionate share in Washington: $185, 197, 033 million in FY 2011
$21 billion U.S. In 2011 FYI: $11 billion Medicare DSH and $10 billion in Medicaid
DSH)
Rationale for reducing DSH payments followed from the expected reduction in the
number of uninsured as a result of Medicaid expansion and implementation of health
insurance exchanges for those not qualifying for Medicaid
Medicare DSH payments will
decrease by 25% in FY 2014
Medicaid DSH payments will
decrease by $14.1 billion
between 2014 and 2020
OPEN MINDS © 2013. All rights reserved.
17
Health care
reform moves
ahead
“Bend the cost
curve” is the
theme
“Beyond FFS” is
the model
Focus on
complex highcost consumers
OPEN MINDS © 2013. All rights reserved.
18
1.
Medicaid expansion likely in all states
except five: Texas, Louisiana, Florida, South
Carolina, Mississippi
2.
3.
Managed care across all populations more
common to control financial risk
Medical loss ratio rules (MLR) and ACOs
causing disintermediation of health
insurance companies
◦ Risk-based partnerships with ACOs
◦ Acquisition of provider capacity
4.
Health exchanges and employer mandates
move ahead
OPEN MINDS © 2013. All rights reserved.
19
1.
2.
3.
4.
5.
6.
Federal and state deficits
Insurers and managed care plans
under price pressure
Consumers paying more out of
pocket
Rising cost per person – aging
population, longer life expectancies,
new technologies
Rising proportion of population
uninsured and uncertain future of
reform
All the ‘easy’ cost savings have been
made
Paying for
Medicare is
taking up all
the Federal
budget
conversation
Paying for
Medicaid is
taking up all
the “oxygen” in
state budgets
OPEN MINDS © 2013. All rights reserved.
20
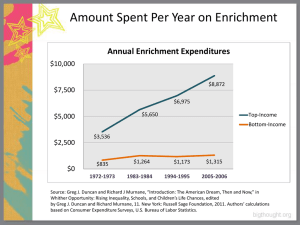
5% of U.S. population
account for half (49%) • $11,487 per person
of health care spending
50% of population
account for only 3% of
spending
• $664 per person
OPEN MINDS © 2013. All rights reserved.
21
•
•
Services to support
chronic illnesses
contribute to 75% of
the $2 trillion in U.S.
annual spending
Patients with comorbid chronic
conditions costs 7x
as much as patients
with one chronic
condition
Nine Highest-Cost
Chronic Conditions
1.
2.
3.
4.
5.
6.
7.
8.
9.
Arthritis
Cancer
Chronic pain
Dementia
Depression
Diabetes
Schizophrenia
Post traumatic conditions
Vision/hearing loss
OPEN MINDS © 2013. All rights reserved.
22
Coordination
more
important
than
integration
Integration of
Primary Care &
Chronic Disease
Management
Integration of
Primary Care &
Behavioral
Health
Integration of Primary
Care & Behavioral
Health Coordination
of behavioral health
services and primary
care services to
improve consumer
services and
outcomes
Integration of Primary
Care & Chronic
Disease Management
Coordination of
services to manage
and address multiple
chronic disease states
within or parallel to
primary care
OPEN MINDS © 2013. All rights reserved.
23
97%
100%
Percent of Total Expenditures
90%
80%
80%
64%
70%
60%
49%
50%
40%
30%
22%
20%
3%
10%
0%
Top 1%
Top 5%
Top 10%
Top 20%
Top 50%
OPEN MINDS © 2013. All rights reserved.
Bottom 50%
24
•
•
•
•
•
•
Management via ACOs,
medical homes, and primary
care
Specialist role is secondary
Focus on prevention and
wellness
Consumer self-care and
consumer convenience is key
Web presence (optimization,
reputation, etc.) critical for
consumer referrals
Health information exchange
a requirement
Primary care
relationships with
clearly defined
specialty service
Consumer
‘experience’ (and
preference) critical
Web presence key
referral mechanism
Health information
exchange
capabilities
OPEN MINDS © 2013. All rights reserved.
25
• Coordination of medical,
behavioral, and social service
needs by specialty group
within larger system
◦ Health homes
◦ Waiver-based HCB programs
◦ PACE programs
◦ Specialty care management
programs
• Assumption of performance
risk (with or without financial
risk)
Cross-specialty and
cross-system care
coordination
capability
EHR system and HIE
with real-time care
management
metrics
Performance-based
contracting and
risk-based
contracting
capabilities
OPEN MINDS © 2013. All rights reserved.
26
New Functionality In
Telecommunications
Synergistic Environmental
Factors In Current Market
New Health Data Systems
& Informatics
Emerging
Developments in
Neuroscience
OPEN MINDS © 2013. All rights reserved.
27
28
29
30
31
32
33
34
OPEN MINDS © 2012. All rights reserved.
35
36
Ipad With Patient Self-Reporting Tools
OPEN MINDS © 2012. All rights reserved.
38
More P4P
New
Service
Delivery
Models
OPEN MINDS © 2013. All rights reserved.
Less FFS
43
Integrated care is a model
of health care delivery that
engages people in the full
range of physical,
behavioral, preventive and
therapeutic services to
support a healthy life.
In an integrated care
setting, behavioral
health and medical
providers work together to
coordinate treatment and
follow-up of a person’s
health care.
OPEN MINDS © 2013. All rights reserved.
44
FFS Financing
Beyond FFS Financing
Payer (or MCO) maintains risk for unit cost
and quantity of services used
Payer (or MCO) contracts with provider
organizations to deliver services to a
population for a fixed amount of dollars
Consumers request services
Consumers request services
MCO “approves” service
Provider organizations deliver services
and are reimbursed based on volume
Provider organizations determine type and
amount of service, delivers service, and
manage pool of dollars
OPEN MINDS © 2013. All rights reserved.
45
The overarching reasons for health care
reform are to achieve the Triple Aim:
• Improve the health of the defined
population
• Enhance the patient experience (including
quality, access and reliability)
• Control or at least, control the per capita
cost of care
OPEN MINDS © 2013. All rights reserved.
46
External Changes
• Successful Behavioral Health Organizations will be
able to identify their customers’ needs and fill them
• Successful Behavioral Health Organizations must
know who their customers are today and how that
customer base will change in the future
• Successful Behavioral Health Organizations must
demonstrate their value and effectiveness to their
customers
OPEN MINDS © 2013. All rights reserved.
47
Examples of Customers:
• Hospitals
◦ Now responsible for meeting certain Medicare
quality measures
◦ Financial penalties are imposed if measures are not
met. Could mean millions of lost revenue.
◦ One major metric hospitals are now measured- 30
day readmission rate for certain diagnoses
◦ Behavioral health patients pose a unique challenge
for hospital discharge planners
OPEN MINDS © 2013. All rights reserved.
48
Health Plans
• State run Health Insurance Exchange
• May be involved down the road for both Medicaid
and/or Medicare/Medicaid (Dual Eligible) clients
• Have certain HEDIS measures that they are
responsible for meeting
• In some states, financial rewards/penalties are
associated with those health plans meeting/not
meeting these standards
OPEN MINDS © 2013. All rights reserved.
49
Primary Care Practices
Many will be
involved in
becoming a Patient
Centered Medical
Home (PCMH)
Typically, these
practices do not
have the expertise
to work with our
population
Will be held
accountable for the
care coordination
and ultimately, for
reducing the cost
of their patients’
care
OPEN MINDS © 2013. All rights reserved.
50
Accountable Care Organizations (ACOs)
• Responsible for managing the care of their ACO
members
• Will again need the expertise of the behavioral
health community in order to manage both the
medical and behavioral health needs of the patient
• Will require creativity in service design to
adequately manage our population (i.e. housing)
OPEN MINDS © 2013. All rights reserved.
51
Other External Changes:
• Technology usage in the area of chemical dependency (i.e. telemedicine, smart
phones)
• Treatment Philosophy issues- Abstinence based versus Medication Assisted
Treatment (MAT)
• Possibility of merging, strategically aligning, partnering with other providersMental Health Agencies, Federally Qualified Health Centers (FQHCs), hospitals,
ACOs
OPEN MINDS © 2013. All rights reserved.
52
Health Care Reform is creating a tremendous amount of
upheaval in our industry. But opportunities will exist for
those organizations that are willing to change and take risks
The missions of your organizations do not have to be
compromised in order to survive in this era of reform
The methods in which you provide services may need to be
changed and/or modified (individualized treatment plans,
technology, customer/referral base)
OPEN MINDS © 2013. All rights reserved.
53
Organizations that are willing to
change, consider other treatment
methods, look to fill the various
customers’ needs will be well
positioned for the future
Organizations that are not open to
exploring various business
relationships or are unwilling to
change the way they do business
because, after all, we’ve always
done it this way will be hard
pressed to survive.
OPEN MINDS © 2013. All rights reserved.
54
It is not necessary to change.
Survival is not Mandatory
Peter Drucker
OPEN MINDS © 2013. All rights reserved.
55
Questions?
OPEN MINDS © 2013. All rights reserved.
56
Upcoming Education Events
2013 Planning & Innovation Institute
June 11-13, 2013 New Orleans, Louisiana
2013 Executive Leadership Institute
September 11-143 2013 Gettysburg, Pennsylvania
OPEN MINDS © 2013. All rights reserved.
57
The market intelligence to navigate.
The management expertise to succeed.
www.openminds.com
openminds@openminds.com
717-334-1329 | 877-350-6463
163 York Street, Gettysburg , Pennsylvania 17325

![The mysterious Benedict society[1]](http://s2.studylib.net/store/data/005310565_1-e9948b5ddd1c202ee3a03036ea446d49-300x300.png)