FY15 Brand Refresh ALA PPT template
advertisement

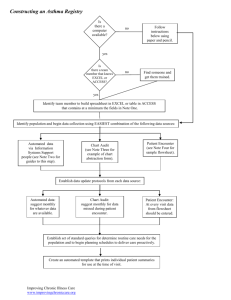
Enhancing Care for Children with Asthma Felicia T. Fuller, Dr.PH Jill Heins, MS November 18, 2014 American Public Health Association New Orleans, LA Project Mission and Method Mission: The systems-change project utilizes a collaborative approach to implement new systems that support and sustain the adherence to the National Heart, Lung, and Blood Institute (NHLBI) asthma guidelines in partnering clinics. Method: Use a continuous quality improvement approach to develop clinic systems that facilitate and ensure high quality asthma care in clinics. Importance of this Initiative 1. Evidence-based framework 2. Sustained changes to the health care system 3. Impact on high-risk, diverse patients 4. Statistically significant outcomes 3 Enhancing Care for Children with Asthma Goals 1. Teach primary care practices how to change (not a top down or cookie cutter model) by using Plan, Do, Study, Act Rapid Cycle Improvement 2. Sustain changes in primary care practice 3. Use “asthma” to learn change 4. Build awareness and capacity in the community 4 Implementation of Initiative 1. State-level project managers 2. 12-month partnership with clinic 3. 5 joint in-person clinic meetings to cover specific quality improvement steps 4. Monthly technical assistance calls 5. Training available 6. Tools and resources provided 7. Chart audits at baseline, 12, and 18 months 5 12 Project Components 1. Buy-in 2. Rooming process 3. Documentation process (opportunity to pilot electronic DDS) 4. Self-assessment process 5. Controller meds 6. Albuterol refill protocol 7. Asthma action plan 8. Spirometry 9. Tobacco dependence 10. Self-management/Patient education 11. ED follow-up 12. Planned visit Lesson learned: Organizational buy-in is most vital. EMR/documentation process is most difficult and takes the most time 6 7 Clinic Trainings Provided 1. Kickin’ Asthma and/or Open Airways 2. Implementation of Spirometry—one hour lecture about how to best conduct spirometry 1. Onsite refresher course provided 3. Interpretation of Spirometry—two hour lecture about how to interpret spirometry 1. Onsite refresher course provided 4. Asthma 101 for clinic staff 5. Asthma Educator Institute – a 16 hour training for non-providers 8 Outcome Measures 1. Severity rating 2. Patient self-assessment (asthma control) 3. Controller medications 4. Written Asthma Action Plans 5. Spirometry 6. Patient education 7. Absenteeism 8. Health care utilization Lesson learned: ALA has the ability to push best practices and quality forward in a friendly way. 9 Regional Findings Improvement in Quality Indicators Baseline - 12 Month - 18 Month Postintervention Aggregate 23 Primary Care Clinics* 100% Illinois New Mexico 90% 80% 70% Texas 60% Oklahoma 40% 50% 30% 20% 10% 0% Severity Rating ACT Baseline Controller Med AAP 12 Month Spirometry Education 18 Month 10 Community Education and Outreach 1. Erie Health System (Chicago) perfected asthma group visit 2. 2 Southside Chicago schools became Asthma Friendly Schools 3. NM legislation to stock emergency albuterol in schools 4. North Navajo Medical Center, EPA, and ALANM to air radio PSAs 5. Training 175 youth coaches in Tulsa 6. Taught 200 students in 7 schools in Tulsa Open Airways for Schools 7. Partnership with Texas Children’s Hospital 8. Trained 65 Asthma 101 community facilitators 9. Re-engaged Texas Gulf Coast Asthma Coalition 11 Can this Model be Replicated/Expanded 1. Proven model with 10 years of experience 2. 160+ clinics in 9 different states 3. Have been supported by 8 different funding sources 4. Works with any variety of clinic models 5. Commitment of clinics for 1-year partnership 6. “Share generously. Steal shamelessly.” 7. Generalizable to other diseases states: COPD and tobacco cessation Lessons learned: This is not a “program in a box”. Experience + Capacity = Success 12 Our Credo We will breathe easier when the air in every American community is clean and healthy. We will breathe easier when people are free from the addictive grip of tobacco and the debilitating effects of lung disease. We will breathe easier when the air in our public spaces and workplaces is clear of secondhand smoke. We will breathe easier when children no longer battle airborne poisons or fear an asthma attack. Until then, we are fighting for air. 13