NCEP ATP IV Guidelines - Montana Pharmacy Association

NCEP ATP IV GUIDELINES:
2013 UPDATE
Kerry Haney, PharmD, BCACP, CPP
UM Skaggs School of Pharmacy
1/12/13
Learning Objectives
1.
2.
3.
List three anticipated changes to the ATP IV guidelines
Compare and contrast two validated risk assessment tools used to stratify risk of developing cardiovascular disease and individualize LDL-c goals
Describe the primary treatment targets from the ATP III guidelines and potential changes for ATP IV
National Cholesterol Education Program (NCEP)
Adult Treatment Panel (ATP) Guidelines
• U.S. guidelines for the detection, evaluation, and treatment of hyperlipidemia in adults
• Developed by an expert panel for the National Heart,
Lung, and Blood Institute (NHLBI)
• Division of National Institutes of Health (NIH)
• Long history of developing clinical practice guidelines
• First JNC report published 1976
• ATP release history:
• ATP I First released in 1988
• ATP II 1993
• ATP III 2001
For more information or to check status: http://www.nhlbi.nih.gov/guidelines/indevelop.htm
Potential Changes for ATP IV
• Current guidelines
• ATP III
•
•
Focus on LDL-c
Greatest intensity of treatment for patients at highest risk
• Other dyslipidemia management guidelines
•
•
Changes in LDL-c targets for those at highest risk
Some modifications of risk factors
• Direction from expert panel for ATP IV
• Critical questions
• Scientific evidence from clinical trials
U.S. Guidelines for
Management of Dyslipidemias
2001
2004
2008
2011
2012
NCEP ATP III guidelines
NCEP ATP III implications
ADA/ACCF Consensus Statement on
Lipoprotein Management in Patients with
Cardiometabolic Risk
AHA/ACC guidelines for secondary prevention
AACE Guidelines for the Management of
Dyslipidemia and Prevention of Atherosclerosis
ADA Standards of Medical Care in DM 2013
AACE = American Association of Clinical Endocrinologists, ACC = American College of Cardiology, ACCF
= American College of Cardiology Foundation, ADA = American Diabetes Association, AHA= American
Heart Association
Critical Questions for ATP IV
What evidence supports LDL-c goals for secondary prevention?
What evidence supports LDL-c goals for primary prevention?
What is the impact of the major cholesterol drugs on efficacy/safety in the populations?
Overview of Potential Changes for ATP IV
• Modification of CVD Risk Estimation
• Adjustment of major risk factors and CHD risk equivalents
• Alternative risk assessment tool to Framingham Risk Score (FRS)
• Changes in Treatment Targets
• Changes in LDL-c goals
• More aggressive treatments in those at elevated risk of CHD
• Changes in target emphasis
• Recommended Pharmacologic Treatment
• Continued use of statins at optimal dosing
• Highlight lack of CV outcome evidence for adjunctive therapies
LDL-c
HDL-c
TG
ATP III Classification of Cholesterol
Concentrations
Lipoprotein
TC
Concentration (mg/dL) Interpretation
< 200
200-239
≥240
Desirable
Borderline high
High
<100
100-129
130-159
160-189
≥190
Optimal
Near/above optimal
Borderline high
High
Very high
<40
≥60
<150
150-199
200-499
≥500
Low
High
Normal
Borderline high
High
Very high
ATP III Treatment Targets
Primary Target:
LDL-c
Secondary Target:
Non-HDL-c
(Once LDL goal met and if TG
≥200)
Exception: TG lowering is an immediate target if ≥ 500 mg/dL
NCEP ATP III: Determining LDL-c Goals
Presence of ASVD,
DM
≥2 major CV risk factors*
Yes No
Yes No
10-year CHD risk:
FRS
High-Risk:
<100mg/dL, optional <70mg/dL
>20% 10-20% <10%
High-Risk :
<100mg/dL
Mod-high Risk:
<130mg/dL, optional
<100mg/dL
Moderate risk
<130mg/dL
Lower risk
<160mg/dL
ATP III 2004 Implications
• Very high risk definition:
• Presence of CVD plus:
•
•
•
•
Multiple major risk factors (DM)
Severe and poorly controlled risk factors (smoking)
Metabolic syndrome
ACS
• Optional goal of LDL-c < 70
Potential Change for ATP IV
CHD Risk Equivalents
• Chronic kidney disease (CKD)
• Potentially added as a CHD risk equivalent
•
•
Increased risk of CHD and premature CHD
Evidence suggests patients with CKD have expected 10-yr risk CHD >
20%
• Guidelines
• National Kidney Foundation (NKF) Kidney Disease Outcomes Quality
Initiative (K/DOQI) Group 2003
• AHA supported recommendation 2003
NCEP ATP III: Determining LDL-c Goals
Presence of ASVD,
DM
Yes No
≥2 major CV risk factors*
Yes No
10-year CHD risk:
FRS
High-Risk:
<100mg/dL, optional
<70mg/Dl
>20% 10-20% <10%
High-Risk :
<100mg/dL
Mod-high Risk:
<130mg/dL, optional
<100mg/dL
Moderate risk
<130mg/dL
Lower risk
<160mg/dL
ATP III Risk Stratification for LDL-c Goal
• Determine presence of other major risk factors
Age
M en≥45
Women ≥55
Family history of premature CHD
First degree relative with heart disease in males before 55 or women before 65
Hypertension
≥ 140/90 or on antihypertensive medications
Cigarette smoking
Low HDL
< 40mg/dL* (negative risk factor if HDL > 60)
If 2 or more risk points are present, then calculate FRS
NCEP ATP III: Determining LDL-c Goals
Presence of ASVD,
DM
Yes No
≥2 major CV risk factors*
Yes No
10-year CHD risk:
FRS
High-Risk:
<100mg/dL, optional
<70mg/Dl
>20% 10-20% <10%
High-Risk :
<100mg/dL
Mod-high Risk:
<130mg/dL, optional
<100mg/dL
Moderate risk
<130mg/dL
Lower risk
<160mg/dL
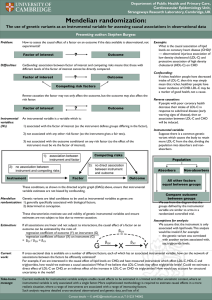
Framingham Risk Assessment Tool
•
•
•
•
Background
•
•
•
Derived from the Framingham Heart Study
Validated method to predict 10year risk of ‘hard’ coronary heart disease
(nonfatal MI or coronary death)
Used in those without ASVD or risk equivalents (DM)
Score
• Low <10%, Moderate 10-20%, High >20%
Limitations
• Predicts risk best
• ages 30-65
• Less precise in those with diabetes, pre-diabetes, severe HTN, LVH, younger men and women, and some racial groups – Japanese-Americans, Hispanic men, and Native American women.
• Limited to estimation of 10-year risk
Available
• http://www.nhlbi.nih.gov/guidelines/cholesterol/atglance.pdf
• http://hp2010.nhlbihin.net/atpiii/calculator.asp
Framingham Risk Assessment Tool
Alternative Risk Assessment Tools
• Reynolds Risk Assessment (RRS)
• Tool has been developed to improve 10-year risk estimation
• FRS may underestimate risk in the young and in women who are classified as low risk
• Utilizes 7 risk factors:
•
• age, SBP, TC, HDL-c, smoking hs-CRP
•
<1 mg/L low, 1-3 mg/L (intermediate), >3 mg/L (high risk)
• parental history of premature MI
• An optional assessment tool in the Canadian Cardiovascular
Society guidelines 2009 and 2012 AACE Dyslipidemia Guidelines
• www.reynoldsriskscore.org
NCEP ATP III: Determining LDL-c Goals
Presence of ASVD,
DM
Yes No
≥2 major CV risk factors*
Yes No
10-year CHD risk:
FRS
High-Risk:
<100mg/dL, optional
<70mg/Dl
>20% 10-20% <10%
High-Risk :
<100mg/dL
Mod-high Risk:
<130mg/dL, optional
<100mg/dL
Moderate risk
<130mg/dL
Lower risk
<160mg/dL
Anticipated Changes to LDL-c Goals
• Optional goals will become new treatment goals
• LDLc goal < 70 for very high risk
• High risk and moderate risk less clear
• Several clinical trials have shown consistent reduction in CHD events (patients with CHD or ACS) when achieving LDL-c of
60-80mg/dL compared to LDL-c levels of 100mg/dL
• PROVEIT-TIMI22, A-to-Z, TNT, IDEAL
• One study has also shown coronary atheroma regression when
LDL-c levels are lowered below 80mg/dL (average 60.8mg/dL) with high potency statins
• Asteriod
• Two studies have shown continuous risk reduction in patients with moderate risk taking statins
• ASCOT, JUPITER
ADA/ACCF Consensus Statement
Lipoprotein Management in Patients with
Cardiometabolic Risk
LDLc
(mg/dL)
Non-HDLc
(mg/dL)
Apo B
(mg/dL)
Very High Risk
Established CVD
DM and ≥ 1 major CVD risk factors*
<70 <100 <80
High Risk
No CVD and ≥ 2 major CVD risk factors*
DM and no major CVD risk factors*
<100 <130 <90
*Risk factors: dyslipidemia, smoking, HTN, family history of premature CAD
Brunzell JD, et al. Diabetes Care 2008; 31:811-22
.
AACE LDLc Treatment Goals
Risk Category
Very High Risk
Patient Population
Established or recent hospitalization for coronary, carotid or peripheral vascular disease
DM with ≥ additional risk factors
LDLc (mg/dL)
< 70
High Risk ≥ 2 major risk factors and FRS > 20%
CHD risk equivalent
≥ 2 major risk factors and FRS 10-20%
< 100
Moderately High Risk <130
Moderate Risk ≥ 2 major risk factors and FRS < 10%
Low Risk
CHD risk equivalent = DM, PAD, AAA, CAD
≤ risk factor
Endocr Pract. 2012; 18 (Suppl 1)
< 130
< 160
Treatment Strategies
• Statins
• Recommended first line:
• Most robust data for efficacy in reducing CHD events
•
•
•
LDL lowering with statin therapy correlates with 30-35% CVD relative risk reduction
Lowers LDL 21-63%
Pleiotropic effects
•
•
•
•
•
Improves endothelial function
Inhibits platelet aggregation
Decreases LDL oxidation
Reduces vascular inflammation
Stabilizes atherosclerotic plaques
• CV event reduction has been disappointing when adding on other lipid lowering therapies
•
•
•
Enhance, SEAS – statin plus ezetimibe
AIM-HIGH – statin plus niacin
ACCORD
– fenofibrate plus simvastatin (in DM)