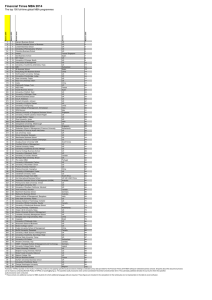
W53_Radakovich_Emplo..

Employers and The
Affordable Care Act – Why
Are We Still Confused?
Presented by: Katherine L.
Radakovich, MBA, SPHR
Chief Human Resources Officer
Chartiers Center
Welcome
• Presenter introduction
• Show respect for differing ideas, thoughts, and questions
• Silence electronic devices
• Time for Q & A will be provided at the end of the presentation
• This is not a substitution for legal advice
Katherine L. Radakovich, MBA,
SPHR
2
Seminar Objectives
• Using the information provided today, participants and Employers will be able to:
– Recognize and understand key components of the ACA
– Differentiate and analyze compliance requirements
– Confidently create an action plan to comply with the ACA and be ready for a DOL audit
Katherine L. Radakovich, MBA,
SPHR
3
How do you feel about compliance and the ACA?
Katherine L. Radakovich, MBA,
SPHR
4
PPACA
• PPACA –Patient Protection and
Affordable Care Act - ACA
• One of the most significant laws affecting the workplace in recent history
• Time to reshape benefit packages
• Communication is key
• Compliance delays
• Interpretation and guidance changes on a daily basis
Katherine L. Radakovich, MBA,
SPHR
5
Recent Top 5 Employer
Concerns
• May 2015 Fisher and Phillips LLP released 5 current employer concerns:
• The employer mandate
• The individual mandate
• Wellness programs
• Reporting requirements
• Automatic enrollment and nondiscrimination regulations
Katherine L. Radakovich, MBA,
SPHR
6
Understand what is (and is not) delayed
• Employer Mandate
– 2015 – large employers (with 100+ employees) are required to offer
ACA compliant (affordable) health care coverage to 70% of their employees. 95% in 2016 (1/1/15)
– Employers with 50-99 – delayed requirement until 2016 (1/1/16)
– Also known as “shared responsibility” or “play or pay”
Katherine L. Radakovich, MBA,
SPHR
7
Understand what is (and is not) delayed
• 2014 – Requirements (not delayed)
– Eliminating pre-existing conditions exclusions
– Imposing the 90 day waiting period
– Eliminating annual dollar limits on essential health benefits
– Include coverage for clinical trials
– Eliminating maximums on annual deductions and limiting out of pocket costs
– Eliminating the ability of grandfathered plans to exclude adult children who have access to other employer coverage
Katherine L. Radakovich, MBA,
SPHR
8
2014-2015 Requirements
• Individual Coverage Mandate
– Individuals are required to obtain health coverage or pay a penalty
– Supreme Court rules it is constitutional
• Health Insurance Exchanges
– States establish insurance exchanges that sell qualified health plans to individuals and small business – or participate in the
Federal Exchange
Katherine L. Radakovich, MBA,
SPHR
9
2014-2015 Requirements
• No Pre-existing Condition Limits
– Elimination of ALL pre-existing condition exclusions
• Dependent Coverage Expansion
– Grandfathered plans may no longer deny coverage to dependent children even if they are eligible for other employer coverage
– Spouses are not considered dependents
Katherine L. Radakovich, MBA,
SPHR
10
2014-2015 Requirements
• Limited Waiting Periods
– Group health plan waiting periods may not exceed 90 days
– Coverage must begin on the 91 st day of employment
– June 2014 – Final Rule - Orientation period can last 1 month before beginning the 90 day waiting period
– This rule applies to plan years starting
January 1, 2015.
– Final rule defines the 1 month orientation period beginning the first of of employment and ends the same day in the following month. Coverage must start by the first day of the fourth month.
Katherine L. Radakovich, MBA,
SPHR
11
2014-2015 Requirements
• Wellness Programs
– Employers can offer employees incentives up to 30 % (may increase to 50%) of the cost of coverage for participation in wellness programs
– HIPAA Wellness Program Rule issued
Katherine L. Radakovich, MBA,
SPHR
12
2014-2015 Requirements
• Automatic Enrollment
– Employers with more than 200 full time employees are required to auto-enroll employees in the health plan
– Delayed until regulations are issued
• Employer Shared Responsibility
– Employers with 100 + employees may face a penalty if the group health plan does not provide affordable, minimum essential coverage to at least 70% of full time employees.
Katherine L. Radakovich, MBA,
SPHR
13
2014-2015 Requirements
• Provision applies if:
– The employer does not offer minimum essential coverage to all full-time employees and their dependents
– The employer offers minimal essential coverage that is not considered affordable or does not provide minimum value
Katherine L. Radakovich, MBA,
SPHR
14
2014-2015 Requirements
• Additional reporting requirements
– Employers are required to file annual reports with the IRS (and provide annual statements to employees)
– Must contain specific plan information, and certification of minimum essential coverage
– Reports due to employees by
January 31 st of the following the year the report is submitted to the
IRS
Katherine L. Radakovich, MBA,
SPHR
15
Are you ready for a DOL audit?
• Affordable coverage
– What is considered affordable coverage under the employer mandate?
• Employee’s contribution to self only benefits cannot exceed 9.5% of the employees household income
• Employers have no practical way of knowing what an employee’s “household income is”
• Employees can shop on the exchange if the employer does not provide affordable or minimum coverage
• Employees may qualify for federal tax credits
• In 2015 large employers will face fines of
$2000 per employee, for failure to provide compliant coverage AND employees qualify for tax credits (2016 Mid-size employers must comply)
• Small employers (50 or less employees) are not required to provide health care coverage
Katherine L. Radakovich, MBA,
SPHR
16
Who is eligible for tax credits?
• An employee qualifies for tax credits when:
– Singles who make less than $46,000
– Family of 4 who earns less than $94,000
– Employers may pay fines up to $2,000 per employee over the first 30 employees
– Employers may pay fines up to $3000 per each employee that actually receives tax credits
• If an employee seeks coverage on the exchange AND the employer offers compliant coverage the employee will not receive tax credits and the employer will not be assessed a penalty
Katherine L. Radakovich, MBA,
SPHR
17
Safe Harbor Methods
• To be compliant with affordable coverage – utilize safe harbor methods:
– Employees required premium co-share for the lowest cost, self-only coverage that provides minimum value not being greater than 9.5% of the employee’s W-2 taxable income
– Taxable calculation currently excludes:
• Employee’s contribution to health savings account
• Employer 401(k) plans, or other nontaxable Section 125 plans (cafeteria plans)
– Cost of Dependent coverage
• Not calculated in the affordable coverage percentage
Katherine L. Radakovich, MBA,
SPHR
18
Safe Harbor Methods
– Coverage is minimum value if
• The plan covers 60% of an employee’s medical expenses. (Actuarial value)
– Minimum value is provided prior to
Wellness program participation
• Minimum value calculation may be calculated assuming that every employee satisfies the terms of the program relating to prevention or reduction of tobacco use.
Katherine L. Radakovich, MBA,
SPHR
19
Full Time Employees
• Under the Employer Mandate:
– Coverage must be provided to employees who work an average of
30 or more hours per week
– The measurement period to meet the 70% coverage and then 95% coverage levels can be 3 -12 months
– Stability period cannot be shorter than 6 months
Katherine L. Radakovich, MBA,
SPHR
20
Qualifying for “fewer than
100 employees”
• Employers must certify
– Employer must average 50 full time employees – includes part time employees’ whose combined hours equal full time employee equivalents
– Feb 2014 – through the end of December
2014 – the employer cannot reduce its workforce or hours of service to meet the condition of having fewer than 100 employees
– Must maintain and/or not reduce the health coverage offered as of February 2014 until the last day of the 2015 plan year
– Employers are not penalized for employees who receive Medicaid coverage
– Mandate delay adds to the penalty confusion
Katherine L. Radakovich, MBA,
SPHR
21
Who is a Full Time Employee or a
Full Time Employee Equivalent?
• FTE = 30 hours/week average (130 hours/month)
• Hours include ANY PAID LEAVE
• Reasonable counting method
– Month to Month
• Penalty determined on a monthly basis
• 3 month breather if coverage is offered the 1 st day of the 4 th month
– Measurement and Stability Period
– May use different methods or measurement periods for different classes
• Hourly v. Salary, Union v. Non-Union, different states NOT variable hour v. non variable hour
Katherine L. Radakovich, MBA,
SPHR
22
Who is a Full Time Employee or a Full Time Employee
Equivalent?
• Break in service/Leave of Absence
Rules
– Must treat rehired employees as new employees
• If period of no service was 13 weeks or more
– Under rule of parity
• Treat as continuing employee as same status for that stability period
• For employees returning after special unpaid leave (FMLA, Jury) – exclude special unpaid leave or credit hours at average weekly rate
Katherine L. Radakovich, MBA,
SPHR
23
Health Care Strategy
Planning
• Keep in mind the following when making decisions about employee health plans:
– The actual cost of play or pay
– The effect of changing the composition of the workforce – reducing employee hours, hiring part time, etc.
– How to treat retirees – do you offer retiree coverage?
– Understand future cost savings of wellness plans
– Eliminate coverage for part time employees
– No longer offer to cover employee spouses
Katherine L. Radakovich, MBA,
SPHR
24
Planning for Federal
Reporting Requirements in
2015
• New regulatory reporting in 2015
– Evaluate the processes you are using to track an employee’s key information:
• Address
• Social Security Number
• Number of individuals covered any given time on the health plan
• Dates employee was covered during a calendar
• This information will be required for reporting
Katherine L. Radakovich, MBA,
SPHR
25
Planning for Federal
Reporting Requirements in
2015
• IRS Reporting
– Internal Revenue Code (Title 26)
• Information gathering begins in 2015
• First reports filed in 2016
– 6055 and 6056
– Information gathering begins in 2015
– Draft form available as of 8/28/14
– Watch for further communication – final rulings
– Completed by anyone who provides minimum essential health coverage
– Section 6056 reporting applies only to large employers
– Currently the IRS is evaluating reporting methods
Katherine L. Radakovich, MBA,
SPHR
26
Planning for Federal
Reporting Requirements in
2015
• Who will be responsible for reporting requirements?
– HR’s new role
• HR will keep employees informed on employer health coverage and about the exchanges
Katherine L. Radakovich, MBA,
SPHR
27
Self Compliance Tool
Affordable Care Act
Provisions
• Be ready for an audit
– Use the self compliance tool
– Does not cover all aspects of the law
– http://www.dol.gov/ebsa/healthref orm/ - most up to date guidance
– Compliance aid is continually updated as changes are made
Katherine L. Radakovich, MBA,
SPHR
28
Self Compliance tool will help you determine the following:
• Determine Grandfather Status and what that means for you, the employer
• Determine compliance with Dependent coverage of children to Age 26
• Determining compliance to Rescission
Provisions
– A cancellation or discontinuance of coverage that has a retroactive effect; treats a policy as void from start date (do not pay premiums)
Katherine L. Radakovich, MBA,
SPHR
29
Self Compliance tool will help you determine the following:
• Compliance with Lifetime Limits and restrictions on annual limits
• Compliance with Pre-existing condition exclusion for individuals
• Compliance provision of supplying the Summary of
Benefits and Coverage to employees and Uniform Glossary
• Compliance with the Patient
Protection Provisions
– Employee has the right to designate primary care provider of choice covered in the plan
Katherine L. Radakovich, MBA,
SPHR
30
Self Compliance tool will help you determine the following:
• Compliance in the coverage of preventive services
– Plan must provide preventive services without cost sharing
• Compliance in the internal claims and appeals process and external review
– Health insurers offering group health plans must offer effective internal claims and appeal process
– Must comply with State or Federal external review process
– Ensure your group health plan offers this provision
Katherine L. Radakovich, MBA,
SPHR
31
Self Compliance tool will help you determine the following:
• Self Compliance tool provides questions to help employers review its group health plan and ensure compliance with ACA
Employer provisions
Katherine L. Radakovich, MBA,
SPHR
32
Cost Controlling Steps while complying with the ACA
Employer Provisions
• Provide Consumer (employee) engagement tools
– Teach employees to be better health care consumers
– Choose a plan that offers cost transparency tools for employees to make smart provider choices
Katherine L. Radakovich, MBA,
SPHR
33
Cost Controlling Steps while complying with the ACA
Employer Provisions
• Consumer Directed Plans
– Implement or expand a CDP
– Assists in the elimination of high cost plans
• Wellness Programs
– Offer wellness incentives
– Cannot violate the HIPAA
Nondiscrimination Rules
• Spousal Coverage
– Eliminate or limit spousal coverage
– Spousal surcharges
Katherine L. Radakovich, MBA,
SPHR
34
Cost Controlling Steps while complying with the ACA
Employer Provisions
• New delivery models
– Encourage employees to use highperformance networks – accountable healthcare organizations, designated centers of excellence
• Specialty pharmacy benefits
– Specialty drugs can make up 30% of a plans costs
– Require step therapy – trying lessexpensive medication to manage condition first
Katherine L. Radakovich, MBA,
SPHR
35
Sharing the cost
• 2015 Employee Contributions
– Move to a private exchange
• Gives employee’s the choice of provider
• Mixed views on whether it will save employers money
– Large organizations will make employees responsible for at least
20% of coverage costs.
– “Skinny” plans do not meet ACA affordability or minimum value test
• Low value plan
Katherine L. Radakovich, MBA,
SPHR
36
Do not ignore the ACA
• In summary – to-dos
– Determine if you are in compliance
• Self audit tool
– Determine if you are a “large” employer
• Subject to play or pay
– Determine your 2015 plan design
– Determine which employees will be eligible for open enrollment
– Determine whether or not your organization will be subject to the
“auto-enroll” requirement (pending ruling status)
Katherine L. Radakovich, MBA,
SPHR
37
Summary
• Use the ACA as a catalyst to strategize employee benefits for recruiting and retention purposes
• ACA is constantly evolving
– Assign an expert in your organization to monitor the ACA
• Its time to get ready for
2015/2016 Reporting
Requirements
Katherine L. Radakovich, MBA,
SPHR
38