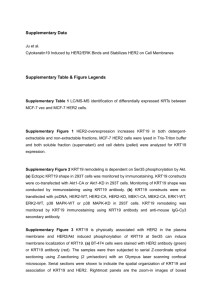
Anti HER2 mAbs
advertisement

A 2008 Lifetime Television movie, directed by Dan Ireland, starring Harry Connick, Jr. The film is based on the true life story of Dr. Dennis Slamon. New York (NY): Random House, 1998. 214 pp., illus. ISBN 0-679-45702-X Targeted Agents for HER2+ Breast Cancer 10.1200/JCO.2011.40.2545 Pertuzumab Trastuzumab Pertuzumab Fisher, et al. J. Mol. Biol. 2010;402:217-229. OS (after an additional year of follow-up) Lancet Oncol 2013; 14: 461–71 Published Online April 18, 2013 FDA On June 8, 2012, the U. S. Food and Drug Administration approved pertuzumab injection (PERJETA, Genentech, Inc.) for use in combination with trastuzumab and docetaxel for the treatment of patients with HER2-positive metastatic breast cancer who have not received prior anti-HER2 therapy or chemotherapy for metastatic disease. Pertuzumab is a recombinant humanized monoclonal antibody that targets the extracellular dimerization domain (Subdomain II) of HER2, and thereby blocks ligand-dependent heterodimerization of HER2 with other HER family members, including EGFR, HER3 and HER4. EMA march 4, 2013 The European Medicines Agency (EMA) has approved Roche’s PERJETATM (pertuzumab) RG1273 for patients with previously untreated HER2-positive metastatic breast cancer (mBC). PERJETA is approved in combination with Herceptin® (trastuzumab) and docetaxel in adult patients with HER2-positive metastatic or locally recurrent unresectable breast cancer, who have not received previous anti-HER2 therapy or chemotherapy for their metastatic disease EMILIA OS: Second Interim Analysis 85.2% (95% CI: 82.0-88.5) 100 OS (%) 80 Median, Mos Events, n Cap + Lap 25.1 182 T-DM1 30.9 149 Stratified HR: 0.68 (95% CI: 0.55-0.85; P = .001) Efficacy stopping boundary P = .0037 or HR: 0.73 64.7% (95% CI: 59.3-70.2) 78.4% (95% CI: 74.6-82.3) 60 40 T-DM1 51.8% (95% CI: 45.9-57.7) Lapatinib-capecitabine 20 0 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 Mos Pts at Risk, n 496 471 453 435 403 368 297 240 204 159 133 110 86 63 Lapatinibcapecitabine 495 485 474 457 439 418 349 293 242 197 164 136 111 86 T-DM1 Data cutoff July 31, 2012; median follow-up: 18.6 mos. 45 27 17 7 4 62 38 28 13 5 Verma S, et al. N Engl J Med. 2012;367:1783-1791. FDA On Feb. 22, 2013, the U. S. Food and Drug Administration approved approved Kadcyla (ado-trastuzumab emtansine), a new therapy for patients with HER2-positive, late-stage* (metastatic) breast cancer. This application is currently under review by the EMA Phase III MARIANNE Study: T-DM1 ± Pertuzumab in HER2+ MBC PD Trastuzumab + Taxane (n=364) Patients with HER2+, previously untreated MBC T-DM1 + Pertuzumab (n=364) (N=1092) T-DM1 + Placebo (n=364) • Primary endpoints: PFS as assessed by IRF, AEs – Superiority design with a noninferiority analysis – Interim futility analysis: option to drop experimental arm • Secondary endpoints: OS, TTF by IRF, ORR, CBR, DOR ClinicalTrials.gov. NCT01120184. MM-302 Nanotherapeutic encapsulation of liposomal doxorubicin with an anti-HER2 antibody fragments coupled to its surface. Upon administration of MM-302, the immunoliposome allows for specific delivery of doxorubicin to tumors overexpressing the HER2 receptor. Once inside the cancer cell, the liposome breaks down and releases doxorubicin intracellularly, promoting cell death. Cancer Res 2012;72(24 Suppl):Abstract nr P5-18-09. Recombinant antibody fragments IgG 150 KDa Fv Fab scFv 50 KDa Fc MM-302 MM-302 MM-302 Targeted Agents for HER2+ Breast Cancer 10.1200/JCO.2011.40.2545 ARRY-380 ARRY-380 is an orally active, small molecule, reversibleselective inhibitor of the HER-2 tyrosine kinase receptor with antitumor activity in HER2-positive breast cancer in vitro and in vivo . In multiple preclinical tumor models, ARRY-380 was well tolerated and demonstrated significant dose-related tumor growth inhibition that was superior to trastuzumab and lapatinib. http://www.arraybiopharma.com/_documents/Publication/PubAttachment430.pdf http://www.arraybiopharma.com/_documents/Publication/PubAttachment462.pdf ARRY-380 These findings led to a phase I trial which found ARRY-380 to be well tolerated, with rash and diarrhea as the most frequent adverse effects http://www.arraybiopharma.com/_documents/Publication/PubAttachment462.pdf http://www.arraybiopharma.com/_documents/Publication/PubAttachment462.pdf http://www.arraybiopharma.com/_documents/Publication/PubAttachment506.pdf Inhibitors of EGFR-receptors Neratinib (HKI-272) oral, multitargeted, irreversible inhibitor of HER1, HER2 and HER4 Neratinib Gajria D Chandarlapaty S. Expert Rev Anticancer Ther. 2011;11(2):263-75 Randomized Phase II: Neratinib vs Lapatinib + Capecitabine in Locally Advanced or MBC Response n Median Survival, Mos 95% CI Neratinib 117 4.5 3.1-5.7 L+C 116 6.8 5.9-8.2 Neratinib 117 19.7 18.2-NE L+C 116 23.6 18.0-NE P Value PFS .231 OS • Most commonly observed severe AEs: diarrhea and hand–foot syndrome – 28% in the neratinib arm vs 10% of the patients in the L + C arm experienced grade 3/4 diarrhea Martin M, et al. SABCS 2011. Abstract S5-7. .280 AFATINIB Afatinib has demonstrated preclinical activity in HER2-positive and triple-negative xenograft models of breast cancer, and clinical activity in phase I studies. The most common treatment-related adverse events of EGFR-TKIs in general, and afatinib in particular, are gastrointestinal and cutaneous side effects, specifically diarrhea and rash The recommended phase II dose of afatinib is 50 mg orally daily based on phase I trials in patients with advanced solid tumor malignancies Afatinib is in Phase III clinical development in breast cancer, NSCLC and head and neck cancer OncoTargets and Therapy 2013:6 This study is ongoing, but not recruiting participants. Cancer Res 2012;72(24 Suppl):Abstract nr OT1-1-16. Novel Monoclonal Antibodies Anti HER2 mAbs MGAH22 TrasGEX Ertumaxomab Anti HER3 mAbs ………. Novel Monoclonal Antibodies Anti HER2 mAbs MGAH22 TrasGEX Ertumaxomab Anti HER3 mAbs ………. MGAH22 www.macrogenics.com MGAH22 Chimeric IgG1 anti-HER2 antibody based on mouse clone 4D5, the precursor to trastuzumab. Engineered to maintain the antigen-binding properties of the original antibody while optimizing its interactions with human FcϒRs. The optimized Fc domain confers enhanced ADCC against all HER2+ tumor cells tested, including cells resistant to trastuzumab’s anti-proliferative activity or expressing low HER2 levels. MGAH22 Novel Monoclonal Antibodies Anti HER2 mAbs MGAH22 TrasGEX Ertumaxomab Anti HER3 mAbs ………. TrasGEX Biosimilar or biobetter? Significantly improved ADCC-activity promising a significantly better therapeutic outcome for all patients eligible for treatment with Trastuzumab. Simultaneously, the fully human nature of Tras-GEX’ host cell lines avoids the common immunogenic reactions against host-derived non-human components. Biosimilars are structural imitations of the originator, whereas biobetters are improvements to the originator biological molecule TrasGEX TrasGEX Phase II is estimated to start in Q3 / 2013. Novel Monoclonal Antibodies Anti HER2 mAbs MGAH22 TrasGEX Ertumaxomab Anti HER3 mAbs ………. Ertumaxomab Bispecific Trifunctional mAb IgG Fab Fv IgG Anti-HER2 Fc Anti-CD3 Fc “An antibody which behaves like a man with a wife and a mistress” Rev. Med. Virol. 2009; 19: 181–183 Clin Cancer Res 2006;12:3085-3091 Ertumaxomab Porin mediated lysis T cells Tumor cells CD3 HER2 Cytokine activation and coreceptor activation Phagocytosis ADCC Fcγ receptor I/III Accessory cell (macrophage, dendritic cell, NK cell…) Clin Cancer Res 2006;12:3085-3091 Phase II Study of Single Agent Trifunctional Antibody Ertumaxomab (Anti-HER-2 & Anti-CD3) in HER-2 Low Expressing HormoneRefractory Advanced Breast Cancer Patients (ABC). Cardoso F et al. Results: Of the planned 40 pts, 28 were enrolled. Recruitment was prematurely terminated due to a strategic change in the sponsor's clinical development program. Eight of 26 evaluable patients (30.8%) had SD at day 70. The median TTP in the evaluable population was 65.5 days (95%, CI: 43-98). The most frequently observed AEs were pyrexia (74.1%), headache (40.7%), chill (33.3%), and vomiting (29.6%). AEs were mostly of mild or moderate intensity and the majority (73.8%) resolved within one day. http://www.abstracts2view.com/sabcs10/view.php?nu=SABCS10L_1066&terms= Novel Monoclonal Antibodies Anti HER2 mAbs MGAH22 TrasGEX Ertumaxomab Anti HER3 mAbs ………. HER2:HER3 Dimers May Provide an Escape Mechanism From Trastuzumab Homodimers HER2:HER2 HER3:HER3 Heterodimers HER4:HER4 HER1:HER2 HER1:HER3 HER1:HER4 HER2:HER3 HER2:HER4 HER1:HER1 + HER3:HER4 + + + + + + + + + + + + + + Signaling activity Tzahar E., et al. Mol Cell Biol. 1996. Sergina NV, et al. Nature. 445:437-441. U3-1287 (AMG-888) The maximum administered dose was 20 mg/kg q2w. The most frequent AEs related to U3-1287 were fatigue (21.1%), diarrhea (12.3%), nausea (10.5%), decreased appetite (7.0%), and dysgeusia (5.3%). No patient developed anti-U3-1287 antibodies. In these heavily pretreated patients, stable disease was maintained ≥ 9 weeks in 19.2% in part 1 and ≥ 10 weeks in 25.8% in part 2. CONCLUSIONS: U3-1287 treatment was well tolerated, and some evidence of disease stabilization was observed. PK data support U3-1287 dosing of 9 to 20 mg/kg every 2 to 3 weeks. Combination studies of U3-1287 are ongoing. MM-121 A Phase 1/2 study evaluating MM-121 in combination with erlotinib is ongoing in patients with non-small cell lung cancer, as well as a Phase 1 dose escalation trial testing the safety and pharmacokinetics of MM-121. MM-121 Recombinant antibody fragments Domain VH - 15 KDa IgG Domain VL - 15 KDa Fv scFv 28 KDa Fab Intrabody Intracellular Localization Domain Fc Cytosol Nucleus Recombinant antibody fragments Tandem antibody “TandAb” IgG Fv Fab Flexibody Fc Triabody 75 KDa Tetrabody 100 KDa Recombinant antibody fragments IgG 150 KDa Diabody 55 KDa Fv Fab Monospecific 50 KDa Diabody Fc Bispecific MM-111 MM-111 is a bispecific antibody fusion protein consisting of two human single-chain variable fragment (scFv) antibodies linked by modified human serum albumin (HSA). IgG 150 KDa 50 KDa modified human serum albumin Fv Fab Anti-HER2 Anti-HER3 Fc MM-111 MM-111 can be rationally combined with trastuzumab or lapatinib for increased antitumor activity and may in the future complement existing HER2-directed therapies to treat resistant tumors Mol Cancer Ther 2012 Mar;11(3):582-93. DEVELOPING A NEW DRUG On average, it takes between nine and 17 years, and only one in approximately 19,817 candidate compounds actually becomes a drug. http://www.eisai.com/ir/individual/knowledge.html