Evidence Based Information Retrieval (Martin)
advertisement

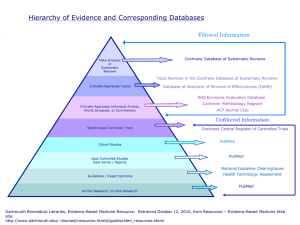
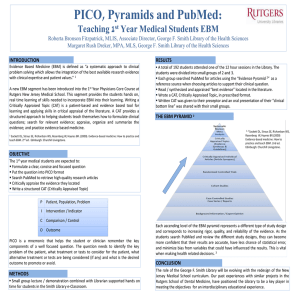
Existing knowledge can prevent… •Waste •Errors •Poor quality clinical care •Poor patient experience •Adoption of interventions of low value •Failure to adopt interventions of high value Source: Sir Muir Gray, Chief Knowledge Officer of Britain’s National Health Service. Quoted on http://www.nks.nhs.uk/. Learning Objectives At the end of the presentation, you will be able to: • Define evidence-based medicine (EBM) • Understand the Five Steps to practice EBM • Use the 4S approach to organizing clinical research evidence • Conduct an efficient online search to track down best evidence • Access online and print tools to critically appraise the evidence • Use the Five Steps in future clinical encounters What is EBM? www.cebm.net “Evidence-based medicine is the integration of best research evidence with clinical expertise and patient values” Patient Concerns EBMClinical Best research evidence Expertise Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS: Evidence based medicine: what it is and what it isn’t. BMJ 1996;312:71-2. Evolution of EBM in the Literature Term first appeared in the literature in a 1991 editorial in ACP Journal Club Volume 114, Mar-April 1991, pp A-16 Seminal article by the Evidence-Based Medicine Working Group published in JAMA Volume 268, No. 17, 1992, pp 2420-2425 Fundamentally new approach becomes widely recognized JAMA published a series of Users’ Guides to the Medical Literature that served as the first learning tools Courses were developed in residency training and medical school curricula The first handbook, Evidence-Based Medicine: How to practice and teach EBM, by Sackett, et al, was published in 1996. Fourth edition published in 2010. New York Times listed EBM as one of its ideas of the year in 2001 BMJ listed EBM as one of the 15 greatest medical milestones since 1840 New Approach Required New Skills Clinical question formulation Search and retrieval of best evidence Critical appraisal of study methods to ascertain validity of results Integration of EBM into medical school curricula patient-doctor courses Information Retrieval for Evidence Based Patient Care Using research findings versus conducting research Retrieving and evaluating information that has direct application to specific patient care problems Selecting resources that are current, valid, and available at point of care Developing search strategies that are feasible within time constraints of clinical practice Key developments that streamlined the practice of EBM Advances in ease of accessing and understanding information Development of preprocessed (preappraised) tools Improvements in search interfaces to MEDLINE Collaboration between EBM Working Group and National Library of Medicine in development of hedges, “clinical queries” tool, that filters search results to specific study types and levels of evidence Dissemination of systematic reviews of primary studies and growth of the Cochrane Collaboration Ongoing Developments… Continuing development of point of care (POC), evidence based summaries, e.g., Dynamed, ACP PIER, UptoDate, Clinical Evidence, FirstConsult None are integrated with individual patient EMRs Can be run through same computers as EMRs Some have a direct link from within the EMR via the “Info Button” Ongoing Developments… “Evolving” decision support systems that will integrate and summarize relevant evidence that answer clinical questions and automatically link, through the EMR, to a specific patient problem Production models exist for parts of decision support systems Cover limited range of clinical problems Ongoing Developments Uptake of Evidence Based Medicine process by health policy, nursing, allied health, and psychosocial fields Terminology is important when searching the literature Subject Heading is Evidence Based Medicine Evidence Based Optometry = Evidence Based Medicine and Optometry Evidence Based Practice is a broad subject heading that is used for Evidence Based Health Care in general EBM Process – 5 Steps 1. 2. 3. 4. 5. ASSESS: Recognize and prioritize important patient problems ASK: Construct clinical questions that facilitate an efficient search ACQUIRE: Track down the best evidence to answer the questions APPRAISE: Systematically evaluate best available evidence for validity, importance, and usefulness APPLY: Interpret the applicability of evidence to specific problems, given patient preferences and values Step 1 1. ASSESS the clinical problem Begin with the patient encounter Select question that Is most important to the patient’s well being Fills gaps in your clinical knowledge Is feasible to answer in the time available Step 2 ASK focused clinical questions Four common types of clinical questions: Therapy/prevention Diagnosis Etiology Prognosis Well Built Clinical Questions Deal with patient management issues Contain elements of PICO format Patient/Population Intervention Comparison Intervention (if useful) Outcome Facilitate an efficient search Example – Therapy/Prevention Question In patients with POAG or OHT, does topical pharmacological treatment compared to no treatment prevent progression or onset of VF defects? Step 3 ACQUIRE: Track down the evidence to answer the question Use the 4S approach to select the most likely resource Start with the highest level resource available 4S Hierarchy 6S Hierarchy Point of Care Summaries: Uptodate, Dynamed, FIRSTConsult, ACP PIER DARE (synopses of syntheses) ACP Journal Club (synopses of studies) Cochrane and other Systematic Reviews MEDLINE Searches limited to Clinical Queries SOURCE: Haynes, R. B. (2001). Of studies, syntheses, synopses, and systems: the “4S” evolution of services for finding current best evidence. Evidence-Based Medicine, 6 (2), 36-38. Retrieved 2-07-07 from http://ebm.bmj.com/cgi/reprint/6/2/36 Critically Appraised Content Evidence Based Retrieval 1. Find the answer that is supported by valid studies appropriate to the type of question and that is available in a timely manner. 2. Requires search terms plus best study design for question plus highest level of evidence Extract search terms from question Therapy/Prevention Question in PICO In patients with primary open angle glaucoma or ocular hypertension [Patient/Population], does topical pharmacological treatment [Intervention] versus no treatment [Comparison Intervention], prevent progression or onset of visual field defects [Outcome]? Possible Search Terms Ocular hypertension, OHT, intraocular pressure, IOP, primary open angle glaucoma, POAG, medical treatment, medical intervention, visual fields, VF Best Study Design for Type of Question Type of Question Study Design Therapy/prevention Randomized controlled trials Diagnosis Prospective cohort, blind comparison to a gold standard Prognosis Cohort, Case Control, Case Series Etiology/Harm Cohort, Case Control, Case Series As you move up the pyramid the amount of available literature decreases, but it increases in its relevance to the clinical setting. Source: Sackett, D.L., Richardson, W.S., Rosenberg, W.M.C., & Haynes, R.B. (1996). Evidence-Based Medicine: How to practice and teach EBM. London: Churchill-Livingstone. Find critically appraised content under “Evidence Based Medicine” Systems/Summaries • DynaMed – Summaries for more than 3,000 topics – Monitors >500 medical journals and systematic review databases – Updated daily – Each article evaluated for clinical relevance and scientific validity – Includes “graded evidence” Glaucoma Summary Evidence-based answer found in 1 minute, 39 seconds DynaMed 1:39 Systems/Summaries • ACP PIER – Over 400 evidence-based summaries for primary care published by the American College of Physicians – Recommendations based on citations from medical literature and ranked by experts at McMaster University – Updated monthly – Reference citations rated by type and quality of study Systems/Summaries • UptoDate – Evidence based summaries of over 9,500 topics in over 20 specialties – Ophthalmology not one of the specialties – Good for information on systemic conditions – Available through individual subscription. Online access plus Mobile app for iPhone and iPad. Cost: $199 per year in training; $499 per year in practice Available in the Optometry Clinic at Hastings Hospital. Use Resource tab and scroll down to the UptoDate link Sample summary at http://www.uptodate.com/contents/management-of-persistent-hyperglycemia-in-type-2diabetes-mellitus Systems/Summaries • FirstConsult – Available through NSU subscription to MD Consult for iPhone or iPad only – Create a personal account in MD Consult – Download the app from the Apple app store – Login with your username and password – Summaries are detailed and include sections on Differential Diagnosis – Eyes and Vision topics well covered Synopses of Syntheses • DARE (Database of Abstracts of Reviews of Effects) – contains structured abstracts of systematic reviews from around the world – covers topics such as diagnosis, prevention, rehabilitation, screening, and treatment – available on Ovid Synopses of Studies • ACP Journal Club – consists of two journals, ACP Journal Club, a publication of the American College of Physicians, and Evidence-Based Medicine, a joint publication of the American College of Physicians and the British Medical Journal Group – includes studies which ACP's editors have selected as methodologically sound and clinically relevant Syntheses • Cochrane Database of Systematic Reviews (DSR) – Part of the Cochrane Library (1996) – 916 completed reviews, 1905 protocols – Among the highest level of evidence upon which to base treatment decisions – Includes Dx since 2008 – Eyes & Vision Research Group • Contains over 165 reviews Systematic Review Analyzes data from several primary studies to answer a specific clinical question Provides search strategies and resources used to locate studies Includes specific inclusion and exclusion criteria (results in less bias) Meta-Analysis (subclass) statistically summarizes results of several individual studies Access full text of Cochrane reviews in OVID Cochrane DSR Review found in 15 seconds Copyright: The Cochrane Library, Copyright 2009, The Cochrane Collaboration Levels of Evidence Grade the quality of evidence based on the design of the clinical study Variety of hierarchies in use DynaMed GRADE Grading of Recommendations Assessment, Development and Evaluation High: High confidence that the evidence supports this finding. Further research is unlikely to change our confidence in the relationship between this clinical action and the reported patient outcome(s) Moderate: Moderate confidence that the evidence supports this finding. Further research may change our confidence in the relationship between this clinical action and the reported patient outcome(s) Low: Low confidence that the evidence supports this finding. Further research is likely to change our confidence in the relationship between this clinical action and the reported patient outcome(s) Very Low (Insufficient): Very low confidence that the evidence supports this finding. There is either no evidence available, or what is available does not allow evaluation of the relationship between this clinical action and the reported patient outcome(s) FirstConsult in transition from SORT to GRADE. See JAMA 300(15) October 2008,”Progress in Evidence-Based Medicine”, for details on GRADE Appraise the Filter (pre-appraised content) Criteria Speed of updating Scope and number of summaries Summaries with graded evidence Authors’ credentials, affiliations listed Developing and using a rubric for evaluating evidence-based medicine point-of-care tools. Journal of the Medical Library Association, Volume 99, No. 3, July 2011 Speed of updating online evidence based point of care summaries: prospective cohort analysis. BMJ 2011;343:doi:10.1136/bmj.d5856 (Published 23 September 2011) Appraisal Required by User Step 4 Appraise best available evidence from original studies If the other “S’s” don’t provide the answer, search for original studies Use “clinical queries” limit in Ovid MEDLINE to speed retrieval Least efficient (in terms of time) to answer clinical questions Primary (Original) Studies Articles that report results of original research investigations Conclusions supported by data and reproducible methodology Require time to acquire and appraise Good Source: MEDLINE (OVID) MEDLINE • Premier biomedical database from the National Library of Medicine (NLM) • Covers 1946-present • Full text available from subscribed NSU journals plus Ovid Deposit Account journals available only for NSUOCO • Ovid interface includes tools to quickly filter search results to specific study types and levels of evidence • Access from http://library.nsuok.edu/collegeop/index.html To Use Clinical Queries Tool, enter search terms and then click on “Additional Limits”. Ovid MEDLINE Clinical Queries Tool Levels of Evidence in Ovid based on AAFP SORT Level A = “Specificity” in Ovid Clinical Queries Systematic reviews of randomized controlled trials including metaanalyses Good-quality randomized controlled trials Level B = “Sensitivity” in Ovid Clinical Queries Good-quality nonrandomized clinical trials Systematic reviews not in Level A Lower-quality randomized controlled trials not in Level A Other types of study: case control studies, clinical cohort studies, cross sectional studies, retrospective studies, and uncontrolled studies Level C Evidence-based consensus statements and expert guidelines Step 5 APPLY the evidence to patient care problems Practice the EBM process in daily patient encounters Access databases and tools from http://library.nsuok.edu/collegeop/index.html UptoDate available at Hastings Hospital Use Resource tab and scroll down to UptoDate link Take Home Points Focused clinical question (PICO) reveals your search terms Start your search at top of 4S hierarchy and work down Be aware of the filter, i.e., levels of evidence, speed of updating Look at more than one resource in the hierarchy. Findings may differ. Practice makes perfect Evidence Based Medicine Lecture NSUOCO Residents Journal Club Sandra A. Martin, M.L.I.S. Health Sciences Resource Coordinator Instructor of Library Services John Vaughan Library Room 305B marti004@nsuok.edu – 918-444-3263