Ebola and Preparedness for THE outpatient setting
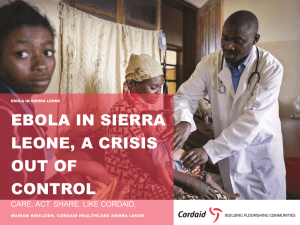
advertisement

The Colorado Medical Society is proud to host: Ebola and preparedness for the outpatient setting featuring Connie Savor Price, MD FOR AUDIO: Dial-In Number (U.S. & Canada): 866.740.1260 Access Code: 8586318 EBOLA AND PREPAREDNESS FOR THE OUTPATIENT SETTING Connie Savor Price, MD Chief, Infectious Diseases Denver Health and Hospital Professor of Medicine University of Colorado Colorado Medical Society November 4, 2014 Disclosures • Grants/Research Support: AHRQ; DHHS/CDC; VA Foundation; Accelerate Diagnostics; Dept of Defense; Medimmune; Rebiotix • Consultant: Accelerate Diagnostics, DHHS/Office of the Assistant Secretary for Preparedness and Response (ASPR), Johns Hopkins International, Kingdom of Saudi Arabia Ministry of Health • Speaker’s Bureau: None • Stock Shareholder: Doximity • Other Financial or Material Support: None Objectives Upon completion of this webinar, participants should be able to . . • Define the epidemiology of the current Ebola outbreak • Describe the risk factors for transmission of Ebola • Apply sound infection prevention strategies to suspected Ebola patients in the outpatient setting BACKGROUND Ebola patient left to die outside Liberian hospital because there is no more room How Many People Have Been Infected? As of October 29, 2014 • More than 13,000 people in Guinea, Liberia, Nigeria, Senegal and Sierra Leone have contracted Ebola since March • More than 4,900 people have died • Liberia: cases doubling ~ every 15-20 days; Sierra Leone and Guinea: cases doubling ~ every 30-40 days http://www.nytimes.com/interactive/2014/07/31/world/africa/ebola-virus-outbreak-qa.html?_r=1 New cases for the week ending Oct. 21 Where is the Outbreak? Montserrado County in Liberia, which includes the capital, Monrovia, recorded over 300 new cases in the week ended Oct 21 Number of New Cases Each Week http://www.nytimes.com/interactive/2014/07/31/world/africa/ebola-virus-outbreak-qa.html?_r=1 Africa is the 2nd Largest Continent It is at least 4 times bigger than the continental US The current Ebola activity is focused in a very small part of Western Africa 2014 Ebola Outbreak Cumulative Cases in Liberia 0 2 4 Range Hundreds of Thousands 8 If the disease continues spreading without effective intervention 6 Assumes 70 percent of patients are treated in settings that confine the illness and that the dead are buried safely. About 18 percent of patients in Liberia and 40 percent in Sierra Leone are being treated in appropriate settings. 10 12 11,000-27,000 cases through Jan. 20 Worst-case Scenario 537,000-1.4 M cases through Jan. 20 14 Best-case scenario http://www.nytimes.com/interactive/2014/07/31/world/africa/ebola-virus-outbreak-qa.html?_r=1 MMWR September 23, 2014 / 63(Early Release);1-14 Comparison to Past Ebola Outbreaks Ebola cases and deaths by year, and countries affected 1976 (virus discovered) 2nd-worst year Sudan, Democratic Republic of Congo 602 cases (dark orange) 431 deaths (light orange) Cases 1995 5th Democratic Republic of Congo 315 cases 254 deaths Deaths 2000 3rd Uganda 425 cases 224 deaths 2007 2014 4th Uganda, Democratic Republic of Congo 1st Sierra Leone, Liberia, Guinea, Nigeria 413 cases 224 deaths 6,553 cases 3,083 deaths as of Sept. 26 http://www.nytimes.com/interactive/2014/07/31/world/africa/ebola-virus-outbreak-qa.html?_r=1 Why Is this Outbreak So Hard to Contain? • Lack of knowledge amongst the population about Ebola • High mobility of people in this area of the world • Wide geographic spread of cases • Distrust of medical personnel • Fear • Incomplete contact tracing • Burial rituals- deceased people are usually washed and then • • • • clothed Culinary practices– bats, bushmeat Lack of adequate public sanitation Access to healthcare Emergence in several highly populated areas in West Africa US to Ramp Up Ebola Response Initiatives Planned by President Obama http://www.wsoctv.com/ap/ap/top-news/us-to-assign-3000-from-us-military-to-fight-ebola/nhNR4/ There Are No Regularly Scheduled Direct Flights To The U.S. From Liberia, Guinea Or Sierra Leone http://fivethirtyeight.com/datalab/why-an-ebola-flight-ban-wouldnt-work/ Ebola Outside of Africa (n=18) Recovered In treatment Died As of Oct. 28, 2014 A doctor, who was recently in Africa treating Ebola patients, tested positive on Oct. 23. Omaha Dallas Oslo London Paris NIH New York Atlanta The two nurses who contracted Ebola at a Dallas hospital were transfered to biocontainment units in Atlanta and Bethesda Hamburg Leipzig Frankfurt Madrid A Spanish nurse contracted Ebola while treating a missionary who died in a Madrid Hospital. Countries with Ebola outbreaks (Nigeria now contained) http://www.nytimes.com/interactive/2014/07/31/world/africa/ebola-virus-outbreak-qa.html?_r=1 9/25 9/28* 9/30* 10/8 Nurse1 tests positive for Ebola 9/24 Positive Ebola test confirmed 9/20 Seeks care at Dallas hospital but is sent home 9/19 Arrives in Dallas to visit family. Nurse2 tests positive for Ebola Patient dies Admitted to Dallas hospital and placed in “isolation” Begins to develop symptoms Boards flight from Liberia. Timeline: Ebola Arrival and Spread in a Dallas Hospital 10/11 10/15 * Nurse 1 and 2 were treating the patient during this time Ebola Among Health Care Workers In As of October 14, 2014 West Africa West African Healthcare Workers 450 MSF Healthcare Workers 416 400 3 350 300 233 250 200 150 700 100 50 0 cases deaths MSF healthcare workers in West Africa since March 2014 Number infected with Ebola US Hospitals Designated To Accept Ebola Patients* *A full list is forthcoming New York/ Long Island Omaha Bethesda Chicago Denver/Aurora Atlanta http://www.nytimes.com/interactive/2014/07/31/world/africa/ebola-virus-outbreak-qa.html?_r=1 The Ebola Virus • Ebola hemorrhagic fever or EVD • Viral Hemorrhagic Fever • Rare and deadly disease • Caused by infection with one of the Ebola virus strains. • Named after the Ebola River in the Democratic Republic of the Congo (formerly Zaire) • First outbreak (Zaire 1976) • 318 human cases • 88% mortality • Spread has been due to healthcare sites, burial rituals and close family contact with ill patient's • Five types • Zaire, Sudan, Tai Forrest, Bundibugyo and Reston Ebola Ranks Relatively Low On The Contagiousness Scale R0 (“R-nought”) Although HIV and Ebola have similar R0s, but Ebola's infections per unit of time is much higher than HIV. When everyone is vaccinated, the R0 to ~zero for measles. Because people with Ebola aren't contagious until they show symptoms,R0 is certain to be way less than two in this country Where Does Ebola Come From? Transmission • Highly infectious but not highly transmissible • Index case likely becomes infected through contact with an infected animal • Once an infection occurs in humans, the virus spreads through direct contact (through broken skin or mucous membranes) with • A sick person's blood or body fluids (urine, saliva, feces, vomit, and semen) • Objects (such as gloves, needles) that have been contaminated with infected body fluids (virus can survive in environment many days) http://www.cdc.gov/vhf/ebola/transmission/index.html Virus Survival • Can survive for several hours on surfaces • Environmental testing of high touch surfaces in an Emory patient room negative • May survive up to 6 days in moist environment • Enveloped virus: standard disinfectants (detergent, 70%ethanol, bleach) are effective Ribner B., IDWeek 2014 Symptoms in Confirmed and Probable Ebola Patients in West Africa, 2014 100 87 80 Specific hemorrhagic symptoms were rarely reported (in <1% to 5.7% of patients). 76 Percent 68 66 65 60 53 44 40 20 39 39 37 (n=467-1151) 33 30 23 22 21 18 13 11 10 8 6 6 0 Dye, C. N Engl J Med 2014;371:1481-95 Time between Exposure and Disease Onset, West Africa, 2014 The mean incubation period was 11.4 days. Approximately 95% of the case patients had symptom onset within 21 days after exposure Dye, C. N Engl J Med 2014;371:1481-95 Diagnosis • Laboratory findings may include low white blood cell and platelet counts and elevated liver enzymes. • Virus detectable by real-time RT-PCR from 3-10 days after symptoms appear (may be detectable earlier) • Collect a minimum volume of 4mL whole blood (preserved with EDTA) in plastic collection tubes • All suspect cases should be immediately reported to the CDPHE Communicable Disease Branch for approval for diagnostic testing • Testing should encompass evaluation for other sources of febrile illness in the returned traveler Treatment • Severely ill patients require intensive supportive care. • Patients are frequently dehydrated and require oral rehydration with solutions containing electrolytes or intravenous fluids. • New drug therapies are being evaluated. Emergency investigational new drug application and IRB needed • Mapp Biopharmaceutical and contact information at • http://www.mappbio.com/ • ZMapp information at • http://www.mappbio.com/zmapinfo.pdf • Chimerix brincidofovir information at • http://ir.chimerix.com/releasedetail.cfm?releaseid=874647 washingtonpost.com British volunteer receives Ebola vaccine in second human trial By Abby Phillip September 17 Felicity Hartnell, a clinical research fellow at Oxford University, injects Ruth Atkins with an experimental Ebola vaccine in Oxford, England. (Steve Parsons/Associated Press/Pool) PLANNING CONSIDERATIONS FOR OUTPATIENT SETTING Assumptions for Planning • Cases will be rare • Cases will not involve multiple persons, likely just individuals • Cases will likely present through Denver International Airport (DIA), Emergency Departments (ED), Urgent Care, less likely on a routine clinic visit • Based on the epidemiology to date in the US, these assumptions are functional for planning at this time, adjustments will be made if warranted. • STAFF SAFETY IS #1 PRIORITY “Ask. Isolate. Call.” Ask: About travel to the 3 countries of interest (Sierra Leone, Liberia, Guinea) Ask: About exposure to persons with Ebola Ask: About symptoms consistent with Ebola Virus Disease Ask: EVERYONE, EVERY TIME Who should ask? MDs, nurses, triage staff, first responders, front office staff “ASK” Screening • Screening of patients at all points of first access • Clinics, Urgent Care Centers, ED, Paramedics, Call Centers • Patient waiting areas shall have signs posted instructing patients to notify provider if they have traveled to West Africa in past 3 weeks • Providers shall have screening tools in provider work areas and exam areas with screening questions Please alert your provider if you have traveled to West Africa in the past 3 weeks Por favor, informe a su médico si usted ha viajado a África occidental en las últimas 3 semanas S'il vous plaît alerter votre fournisseur si vous avez voyagé en Afrique de l'Ouest au cours des 3 dernières semaines When to Suspect Ebola Suspect Ebola in patients who have TRAVELED TO GUINEA, SIERRA LEON, or LIBERIA WITHIN 21 DAYS of symptoms or contact with blood or body fluids of another person known to have or suspected to have Ebola AND One or more of the following SYMPTOMS: Fever (subjective or measured greater than 38.0°C or 100.4°F) - Severe headache - Muscle Pain - Weakness Abdominal (stomach) pain - Vomiting - Lack of Appetite - Diarrhea - Unexplained bleeding or bruising Call 911 Modified from Identify, Isolate, Inform: Emergency Department Evaluation and Management for Patients Who Present with Possible Ebola Virus Disease http://www.cdc.gov/vhf/ebola/hcp/ed-management-patients-possibleebola.html Oct 31, 2014 Call CDPHE 303-692-2700 or 303-370-9395 (after hours) Personal Protective Equipment • Initial Evaluation for Clinically Stable and “Dry” Patient • • • • • Face shield Mask or respirator Gown- Impermeable or fluid resistant Gloves (double) Limit patient and environmental contact • Hospital Management for Clinically Unstable or “Wet” Patient* • Impermeable gown, 2 layers of gloves, N95 or PAPR hood, Face • • • • shield, Surgical hood, Boot covers Strict donning/doffing protocol with trained staff Always work in pairs Must document competency Essential staff only *http://www.cdc.gov/vhf/ebola/hcp/infection-prevention-and-control-recommendations.html Requires evaluation and care in a specialized (usually ED) setting with facilities and trained staff Good Doffing for Everyday Infection Prevention The are general* recommendations for safe donning and doffing of PPE *Specific recommendations for Ebola are described for the hospital setting in the CDC’s Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Virus Disease in U.S. Hospitals “CALL” What to report to CDPHE (303-692-2700, evenings and weekends: 303-370-9395) • All suspect cases should be immediately reported to CDPHE. • Persons who have NO symptoms of Ebola but have exposure to Ebola (either “high-risk” or “some risk”). • State health will notify local public health agencies of a suspect case in their jurisdiction immediately. • State public health will assist all hospitals and local health departments with a suspect case. This includes coordinating with CDC, figuring out logistics, transport of patient (if needed), getting appropriate testing, case-finding, etc. Then what? Clinical and public health action plan, based on exposure risk and clinical presentation. Environmental Contamination • CDPHE will provide guidance • Do not attempt to disinfect area on your own • Block off contamination, move patients and healthcare workers away from contamination Handling Waste in Clinics • All waste will be handled as category A waste • Do not attempt to clean up or dispose of waste OUTPATIENT TABLETOP 42-year-old Liberian male presents with low-grade fever and abdominal pain +/vomiting. What is the next step? A. Prescribe ciprofloxacin for his abdominal pain and send B. C. D. E. him home Obtain the intake nurse’s notes Ask him when he was last in Liberia Draw a CBC and basic chemistries Have the patient’s family member call the CDC You are concerned for Ebola. What is the next step? Choose as many as apply A. Put the patient in a negative airflow room B. Find a PAPR and quickly learn how to use it C. Notify public health D. Put the patient in an exam room (ideally with a bathroom) E. Wash your hands and put on gloves, gown (fluid resistant or impermeable), eye protection (goggles or face shield), facemask before continuing further evaluation You learn he was in Monrovia 11 days ago. Before he can answer your questions about sick contacts, he vomits at the registration desk. What do you do next? A. Immediately clean it up B. Block off the area and relocate patients and staff away from the contaminated space C. Pour bleach on it (you planned to replace the carpet anyway) D. Ask the patient to clean it up E. Evacuate the building The patient is escorted to a private room. He was accompanied by family members. What do you do next? Choose as many as apply. A. Escort the family members to a separate exam room B. Ask if any of the family members feel ill C. Ask them to leave the clinic immediately D. Give them a mask E. Collect their contact information F. Call CDPHE The patient’s temperature is measured at 103 degrees. CDPHE has sent paramedics and the patient is removed from your clinic. What do you do next? A. Cancel your clinics for the next 21 days B. Make sure you take out all the trash from the patient’s C. D. E. F. exam room Book a cruise, leave ASAP Perform fever and symptom monitoring for 21 days Quarantine yourself in an outdoor tent Await further guidance from CDPHE Where do you find more information? A. www.colorado.gov/ebola B. www.cdc.gov/ebola C. COHELP (303-389-1687 or 1-877-462-2911) D. www.cms.org E. All of the above QUESTIONS? Connie.Price@dhha.org