Potentially inappropriate prescribing and cost outcomes for older
advertisement
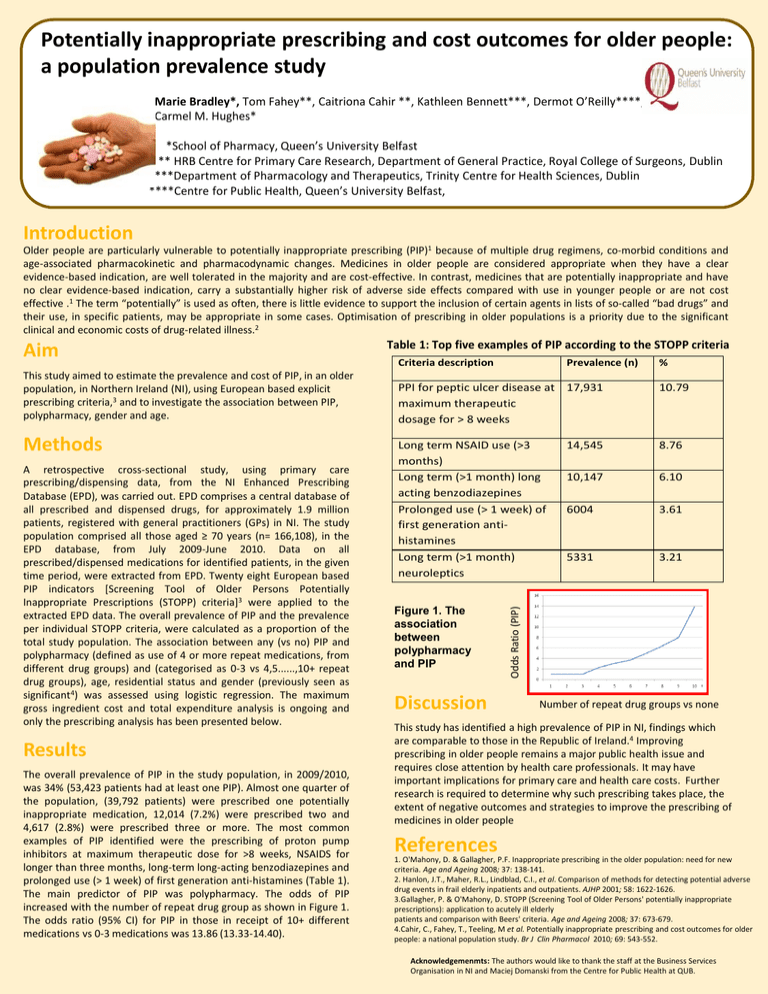
Potentially inappropriate prescribing and cost outcomes for older people: a population prevalence study Marie Bradley*, Tom Fahey**, Caitriona Cahir **, Kathleen Bennett***, Dermot O’Reilly****, Carmel M. Hughes* *School of Pharmacy, Queen’s University Belfast * ** HRB Centre for Primary Care Research, Department of General Practice, Royal College of Surgeons, Dublin ***Department of Pharmacology and Therapeutics, Trinity Centre for Health Sciences, Dublin ****Centre for Public Health, Queen’s University Belfast, Introduction Older people are particularly vulnerable to potentially inappropriate prescribing (PIP)1 because of multiple drug regimens, co-morbid conditions and age-associated pharmacokinetic and pharmacodynamic changes. Medicines in older people are considered appropriate when they have a clear evidence-based indication, are well tolerated in the majority and are cost-effective. In contrast, medicines that are potentially inappropriate and have no clear evidence-based indication, carry a substantially higher risk of adverse side effects compared with use in younger people or are not cost effective .1 The term “potentially” is used as often, there is little evidence to support the inclusion of certain agents in lists of so-called “bad drugs” and their use, in specific patients, may be appropriate in some cases. Optimisation of prescribing in older populations is a priority due to the significant clinical and economic costs of drug-related illness.2 This study aimed to estimate the prevalence and cost of PIP, in an older population, in Northern Ireland (NI), using European based explicit prescribing criteria,3 and to investigate the association between PIP, polypharmacy, gender and age. Methods A retrospective cross-sectional study, using primary care prescribing/dispensing data, from the NI Enhanced Prescribing Database (EPD), was carried out. EPD comprises a central database of all prescribed and dispensed drugs, for approximately 1.9 million patients, registered with general practitioners (GPs) in NI. The study population comprised all those aged ≥ 70 years (n= 166,108), in the EPD database, from July 2009-June 2010. Data on all prescribed/dispensed medications for identified patients, in the given time period, were extracted from EPD. Twenty eight European based PIP indicators [Screening Tool of Older Persons Potentially Inappropriate Prescriptions (STOPP) criteria]3 were applied to the extracted EPD data. The overall prevalence of PIP and the prevalence per individual STOPP criteria, were calculated as a proportion of the total study population. The association between any (vs no) PIP and polypharmacy (defined as use of 4 or more repeat medications, from different drug groups) and (categorised as 0-3 vs 4,5......,10+ repeat drug groups), age, residential status and gender (previously seen as significant4) was assessed using logistic regression. The maximum gross ingredient cost and total expenditure analysis is ongoing and only the prescribing analysis has been presented below. Results The overall prevalence of PIP in the study population, in 2009/2010, was 34% (53,423 patients had at least one PIP). Almost one quarter of the population, (39,792 patients) were prescribed one potentially inappropriate medication, 12,014 (7.2%) were prescribed two and 4,617 (2.8%) were prescribed three or more. The most common examples of PIP identified were the prescribing of proton pump inhibitors at maximum therapeutic dose for >8 weeks, NSAIDS for longer than three months, long-term long-acting benzodiazepines and prolonged use (> 1 week) of first generation anti-histamines (Table 1). The main predictor of PIP was polypharmacy. The odds of PIP increased with the number of repeat drug group as shown in Figure 1. The odds ratio (95% CI) for PIP in those in receipt of 10+ different medications vs 0-3 medications was 13.86 (13.33-14.40). Table 1: Top five examples of PIP according to the STOPP criteria Criteria description Prevalence (n) % PPI for peptic ulcer disease at maximum therapeutic dosage for > 8 weeks 17,931 10.79 Long term NSAID use (>3 months) Long term (>1 month) long acting benzodiazepines Prolonged use (> 1 week) of first generation antihistamines Long term (>1 month) neuroleptics 14,545 8.76 10,147 6.10 6004 3.61 5331 3.21 Figure 1. The association between polypharmacy and PIP Discussion Odds Ratio (PIP) Aim Number of repeat drug groups vs none This study has identified a high prevalence of PIP in NI, findings which are comparable to those in the Republic of Ireland.4 Improving prescribing in older people remains a major public health issue and requires close attention by health care professionals. It may have important implications for primary care and health care costs. Further research is required to determine why such prescribing takes place, the extent of negative outcomes and strategies to improve the prescribing of medicines in older people References 1. O'Mahony, D. & Gallagher, P.F. Inappropriate prescribing in the older population: need for new criteria. Age and Ageing 2008; 37: 138-141. 2. Hanlon, J.T., Maher, R.L., Lindblad, C.I., et al. Comparison of methods for detecting potential adverse drug events in frail elderly inpatients and outpatients. AJHP 2001; 58: 1622-1626. 3.Gallagher, P. & O'Mahony, D. STOPP (Screening Tool of Older Persons' potentially inappropriate prescriptions): application to acutely ill elderly patients and comparison with Beers' criteria. Age and Ageing 2008; 37: 673-679. 4.Cahir, C., Fahey, T., Teeling, M et al. Potentially inappropriate prescribing and cost outcomes for older people: a national population study. Br J Clin Pharmacol 2010; 69: 543-552. Acknowledgemenmts: The authors would like to thank the staff at the Business Services Organisation in NI and Maciej Domanski from the Centre for Public Health at QUB.