workshop slides
advertisement

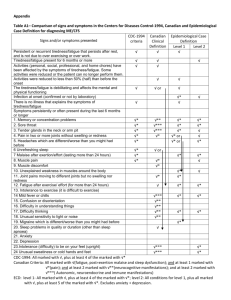
SCOTTISH GOOD PRACTICE STATEMENT ON ME-CFS Dr Gregor Purdie GP and Clinical Lead for ME-CFS Dumfries and Galloway Health Board Dr Gregor Purdie • GP for 27 years • First encouraged to take interest in this area as a JHO in 1979 • Recognised patterns of illness in patients in GP practice • Clinical Lead for ME-CFS for Dumfries and Galloway Health Board from 1997 Dr Gregor Purdie • • • • Developed links with MERUK Met Keith Anderson Member Cross Party Group on ME at Holyrood Development of Scottish Good Practice Statement on ME-CFS • Parallel development of Health Care Needs Assessment WHY A GOOD PRACTICE STATMENT • Ill understood clinical area • Levels of evidence of interventions not strong enough for SIGN Guideline • Controversial area of practice • Much research still needing to be undertaken CLINICAL ASSESSMENT Presentation • • • • Onset sudden on gradual Post viral Physical illnesses Stressful events Presenting symptoms • Persistent/recurrent fatigue • Muscle/joint aches and pains • May be present at rest and provoked by physical and mental exertion • POST EXERTIONAL FATIGUE • Substantial reduction in activity levels PRESENTING SYMPTOMS • • • • • • • Recurrent flu like symptoms Sore throats Painful swollen lymph glands Sleep disturbance Headaches Muscle twitches/spasms/weakness Fogging of cognition Other Presenting Symptoms • • • • • • • Peri-oral and peripheral parasthesiae Postural light headedness Palpitations Dizzyness Sensitivity to light and noise Pallor Nausea and Irritable Bowel Symptoms Other Presenting Symptoms • • • • Alcohol Intolerance Urinary Symptoms Feelings of fever and shivering Altered appetite and weight EXAMINATION • • • • • • Height and weight ERECT AND SUPINE BP General Clinical Examination Skin and joints Neurological Examination Mental State Examination “RED FLAGS” • Substantive unexplained weight loss • Neurological signs • Symptoms or signs of inflammatory joint disease or connective tissue disease • Symptoms or signs of cardio-respiratory disease • Symptoms of sleep apnoea • Clinically significant lymphadenopathy INVESTIGATION • There is at present no confirmatory test available on the NHS • Present clinical investigation is to help exclude alternative diagnoses INVESTIGATIONS FOR ALL PATIENTS • • • • • • • FBC U&Es and Creatinine and LFTs TFTs Glucose ESR/CRP Calcium Creatine Kinase INVESTIGATIONS WHERE INDICATED BY HISTORY OR EXAMINATION • • • • • • • AMA (if minor alterations in LFTs) ANA Coeliac Serology CMA EBA ENA HIV INVESTIGATIONS WHERE INDICATED BY HISTORY OR EXAMINATION • • • • Hepatitis B and C LYME SEROLOGY Serology for chronic bacterial infections Toxoplasma • ECG • Tilt table testing INTERVENTIONS, MANAGEMENT AND REHABILITATION General Principles • Good doctor patient relationship • Treat patients with respect • Empathic listening • All treatment plans collaborative and tailored to the needs of individual patients TREATMENT OF SPECIFIC SYMPTOMS • • • • • Headache Irritable Bowel Syndrome Dizzyness Depression Sleep disturbance • Follow standard clinical practice • Physical treatments – eg TNS and Acupunture MEDICATION • Usually beneficial to start with a very low dose • Liquid preparations found to be helpful • Side effects can be bad in the initial treatment stages DIETARY ADVICE • Food intolerances reported • Encourage a healthy diet • Reported value from Vit B12, Vit C, co-enzyme Q, multi-vitamins and minerals. • Vit D REHABILITATION • • • • PACING Graded Exercise Couselling Cognitive behaviour therapy SPECIAL AREAS CHILDREN Presentation • CAN BE PROFOUNDLY AFFECTED • Significant impact on development and academic progress • Fluctuation in severity can be more dramatic than in adults • Severe exhaustion, weakness, pain and mood changes make life very challenging Prognosis • The evidence available suggests that children and young people are more likely to recover than adults. Principles of Care • BASED ON GIRFEC • “feel confident about the help they are getting; understand what is happening and why, have been listened to carefully and their wishes have been heard and understood; are appropriately involved in discussions and ddecisions which affect them; can rely on appropraite help being available as soon as possible; and that they will have experienced more streamlined and coordinated response from pratitioners” DIAGNOSIS • Speedy diagnosis to ally fears of other serious illness • Children can be diagnosed when symptoms have been present for 3 months • Diagnostic criteria as per adults Clinical Presentation • • • • • Loss of energy/fatigue Cognitive problems Disordered sleep patterns Weight change Gastro-intestinal disorder • Investigation similar as for adults Clinical Management • • • • • • As advocated in RCPCH Guideline:Activity management advice Advice and symptomatic treatment Early engagement with the family Regular Review of Progress Specific Advice on diet, sleep problems, pain management, pyschological support and comorbid depression where present CARE NEEDS • A CHILD CAN BE SO PROFOUNDLY AFFECTED THAT THE FAMILY MAY REQUIRE PRACTICAL HELP IN THHE HOME SETTING • SPECIALIST REFERRAL • COMMUNITY OT • MONITORING AND REVIEW SCHOOLING • DIFFICULTIES IN MAINTAINING A SCHOOL PROGRAMME • EXCLUDE OTHER DEFINED CAUSES OF SCHOOL ABSENCE • SUPPORTIVE LETTER FROM GP OUTLINING CONDITION • ARRANGEMENTS RESPONSIVE TO CHILD’S CONDITION CHILD PROTECTION • CONCERNS THAT MISUNDERSTANDING AND LACK OF INFORMATION ABOUT ME-CFS IN EDUCATION AND SOCIAL SERVICES HAVE LED TO INAPPROPRAITE INITIATION OF CHILD PROTECTION PROCEDURES SEVERELY AFFECTED SEVERELY AFFECTED • IN MOST EXTREME CASES TOTALLY BEDBOUND or housebound and wheelchair bound • Can be triggered by one prominent symptom or a cluster • REPORT CONSTANT PAIN • INABILITY TO TOLERATE MOVEMENT, LIGHT OR NOISE AND CERTAIN SCENTS AND CHEMICALS Severely affected • Severe – any patient who is so affected as to be effectively housebound for a prolonged period for time(>3 months) • Very severe – bedridden for a prolonged period (>3 months) Principles of Care • • • • • • Very individualised approach Check for inter-current illnesses Realistic Expectations Agreement of goals Input from full Primary Care Team Aware of extent of clinical needs Management • • • • • • • Medication – value of liquid preparations Referral Diet Hospitalisation Respite Caring for the Carers Part of Long Term Conditions planning PROGNOSIS PROGNOSIS • Majority show a degree of improvement over time • Relapse and remission • Milder fatigue states have a more favourable outcome • Significant minority severely affected for many years THE FUTURE RESEARCH AND DEVELOPMENT • Controversies on present assessment and management eg GET and CBT • Need for evidence base for empirical research • XMRV • MRC • MERUK • Development of a national group to drive forward the agenda