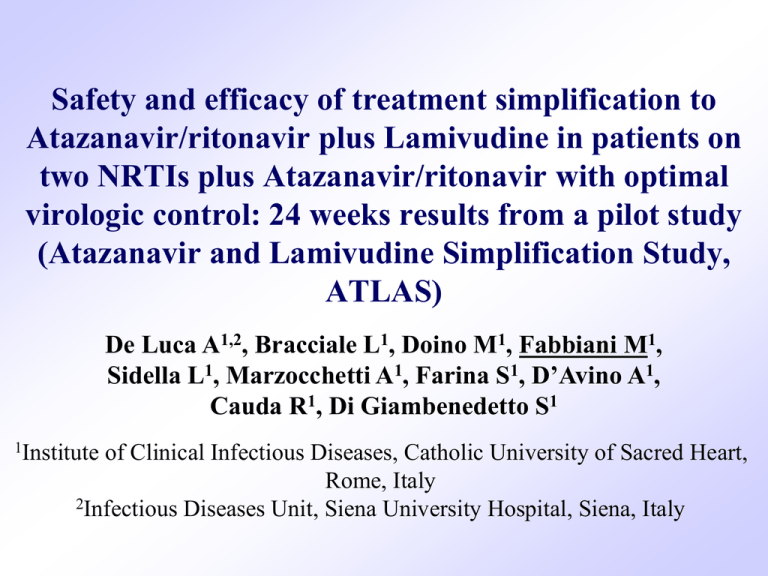
Safety and efficacy of treatment simplification to
Atazanavir/ritonavir plus Lamivudine in patients on
two NRTIs plus Atazanavir/ritonavir with optimal
virologic control: 24 weeks results from a pilot study
(Atazanavir and Lamivudine Simplification Study,
ATLAS)
De Luca A1,2, Bracciale L1, Doino M1, Fabbiani M1,
Sidella L1, Marzocchetti A1, Farina S1, D’Avino A1,
Cauda R1, Di Giambenedetto S1
1Institute
of Clinical Infectious Diseases, Catholic University of Sacred Heart,
Rome, Italy
2Infectious Diseases Unit, Siena University Hospital, Siena, Italy
Introduction
• Long term toxicity and costs of cART
highlight the need of treatment simplification
strategies
• Monotherapy with boosted PIs has been
investigated with controversial results
• Dual therapy could be a suitable option in
certain patients
Atazanavir/ritonavir + lamivudine
• Tolerability:
– ATV is a PI with a low metabolic impact;
– 3TC generally very well tolerated.
• Once daily administration
• Relatively limited pill burden
• Relatively limited costs
ATLAS
• Pilot study (40 patients)
– Prospective single-arm, single center, 48 weeks
– Safety and tolerability
– Max allowed failure rate (confirmed VL>50 cp/mL):
12.5%
– Enrolment June 2009 – May 2010
– Clinicaltrials.gov NCT00885482
• Inclusion criteria:
– Patients on ATV/rit + 2 NRTIs from at least 3 months
– HIV-RNA <50 copies/mL from at least 3 months
– CD4 >200 cells/µL from at least 6 months
ATLAS
• Exclusion criteria:
– Previous virological failure of 3TC or PIcontaining regimens or exposure to mono-dual
NRTI
– Virological failure with other regimens but a GRT
with any RAM to 3TC or ATV
– Proton pump inhibitors co-administration
– HBsAg positive
– Pregnancy
ATLAS: study procedures
• At baseline simplification to ATV/rit 300/100 mg OD +
3TC 300 mg OD
• Follow up visits at 4, 12, 24, 36 and 48 weeks
• At each visit: chemistry, CD4 and HIV-RNA, TDM, self
reported adherence (VAS)
• At baseline and at 48 weeks: Quality of Life, self-reported
symptoms, Neurocognitive assessment, Bone density
(DXA), Fat distribution (DXA, Liposound), carotid IMT
and endothelial function (brachial FMD)
Population: baseline characteristics (n=40)
Age (years)*
Male sex
Foreign born
Injecting drug users
HCV co-infection
Past AIDS-defining events
Time from HIV diagnosis (years)*
Time (years) from starting cART*
Time (years) from starting last cART regimen*
Tenofovir-containing NRTI backbone
CD4 cells count (cells/µL)*
CD4 cells count nadir (cells/µL)*
Time (months) with viral load <50 copies/mL*
n (%)
45 (41-52)
23 (57.5)
2 (5)
9 (22.5)
8 (20)
9 (22.5)
11.4 (7.1-15.2)
8.5 (6.3-10.2)
2.6 (1.7-4.2)
39 (97.5)
598 (483-778)
108 (45-223)
21 (10-30)
Values are expressed as n (%) except for *median (IQR)
Results of 24 weeks interim analysis
• 40/40 patients completed Week 4, 38/40 Week 12, 36/40 week 24
• All patients maintained an HIV-RNA<50copies/mL, without
viremic blips
• No significant modifications of CD4 cells count
Proportion of patients with
HIV-RNA<50copies/mL
120
100
100%
100%
100%
100%
80
60
40
20
0
BL
Week 4 Week 12 Week 24
Changes in CD4 cells count
P=0.458
P=0.402
P=0.277
Severe clinical adverse events
A total of 5 severe adverse events were
observed in 5 patients :
• 2 renal colic
• 1 hypertensive crisis
• 1 brain hemorrhage
• 1 pregnancy (the only dropped patient)
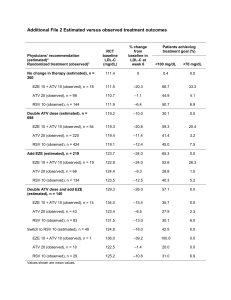
Laboratory toxicity
• 14 patients with baseline grade 3 elevation of total
bilirubin
• New grade 3 laboratory toxicities were observed in 18 pts
Grade 3
toxicities at
baseline
New Grade 3 toxicities
Week 4
Total bilirubin
14/40 (35%) 6/25 (24%)
Total Cholesterol
2/38 (5.3%)
LDL
2/35 (5.7%)
Triglycerides
1/38 (2.6%)
Amylases
Week 12
Week 24
9/24 (37.5%) 6/21 (28.6%)
3/38 (7.9%) 1/36 (2.8%)
4/33 (12.2%) 2/35 (5.7%)
1/38 (2.6%)
1/33 (3%)
Total patients
13
3
4
1
1
Mean change (mg/dL)
Cholesterol changes from baseline
+20
+21
P<0.01 for all parameters at all time points
+18
+17
+13
+9
+4 +3 +4
Baseline
Week 4
Week 12
Week 24
TC/HDL 4.3 (3.5-5.4) 4.2 (3.5-5.5) 4.4 (3.5-5.6) 4.4 (3.5-5.6)
HDL/LDL 0.4 (0.3-0.5) 0.4 (0.3-0.5) 0.4 (0.3-0.5) 0.4 (0.3-0.5)
p
ns
ns
Triglycerides changes from baseline
P=0.442
P=0.126
P=0.342
-0.04
P=0.020
-0.06
P=0.012
-0.08
P<0.001
Mean change (mL/min/1.73m2)
Mean change (mg/dl)
Renal function change from baseline
+6
P=0.097
+6
P<0.001
+4
P=0.017
Mean change (mg/dL)
Bilirubin change from baseline
+0.3
P=0.07
+0.3
P=0.04
+0.1
P=0.7
+0.1
P=0.5
+0
P=0.8
+0.1
P=0.6
Changes in ATV plasma levels (C24h or C12h)
P=0.664
P=0.469
P=0.925
Patients
BL
36
W4
32
W12
28
W24
25
ATV geometric mean (GM)
2.21 (0.22-5.76) 2.46 (0.63-5.70) 2.82 (0.48-7.58) 2.20 (0.04-10.2)
concentration (95% CI), mg/L
GM relative changes
-
+11.3%
+27.6%
-0.5%
Conclusions
• Simplification regimen with ATV/rit+3TC maintained
virological suppression through 24 weeks
• 2 severe adverse events possibly related to drugs (renal
colic); no severe laboratory adverse event; bilirubin
increased temporarily.
• TC, HDL and LDL increased (a lipid-lowering effect of
TDF was recently suggested)*; TC/HDL and HDL/LDL
ratios were unchanged.
• Renal function improved significantly (probably due to
TDF discontinuation)
*Tungsiripat
M. AIDS. 2010 Jul 17;24:1781-4
Conclusions
• 48 weeks efficacy and safety results are necessary to
confirm preliminary safety and efficacy of simplification
to ATV/r+3TC
• Results will form the basis for definitive testing of this
strategy in a randomized controlled trial.