AADs pharmacology1
advertisement

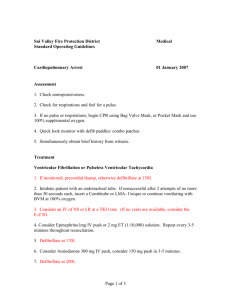
Anti-Arrhythmic Agents PRCL 628: Medical Pharmacology Robert J. DiDomenico, PharmD, FCCP Clinical Associate Professor Cardiovascular Clinical Pharmacist OBJECTIVES For each of the anti-arrhythmic drugs, students should be able to: 1. Describe the mechanism of action. 2. Compare and contrast the pharmacokinetic and drug interaction profiles within each class. 3. Compare and contrast the clinical effects. 4. List the common and/or serious adverse effects. Anti-Arrhythmic Agents PRCL 628: Medical Pharmacology Required Reading: 1. Hume JR, Grant AO. Chapter 14. Agents Used in Cardiac Arrhythmias. In: Katzung BG, Masters SB, Trevor AJ, eds. Basic & Clinical Pharmacology. 12th ed. New York: McGrawHill; 2012. http://www.accessmedicine.com/content.aspx?aID=55822293. Suggested Reading: 1. Sampson KJ, Kass RS. Chapter 29. Anti-Arrhythmic Drugs. In: Knollmann BC, ed. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011. http://www.accessmedicine.com/content.aspx?aID=16668361. “Antiarrhythmic drugs are toxins with occasional therapeutic side effects” • Peter Buttrick, MD Sampson KJ, Kass RS. Chapter 29. Anti-Arrhythmic Drugs. In: Knollmann BC, ed. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011. http://www.accessmedicine.com/content.aspx?aID=16668361. Mechanisms of Arrhythmias Arrhythmia Common Mechanism Therapy Premature atrial, nodal, & ventricular depolarizations Unknown None Atrial fibrillation Disorganized Control ventricular rate: AV nodal blockade “functional” re-entry Maintain NSR: Class I & III AADs, ablation Atrial flutter Disorganized Control ventricular rate: AV nodal blockade “functional” re-entry Maintain NSR: Class I & III AADs, ablation Atrial tachycardia Automaticity or re-entry Control ventricular rate: AV nodal blockade Maintain NSR: Class I & III AADs, ablation AVNRT Re-entry within/near AV node AV nodal blockade Ablation AVRT Re-entry (accessory pathway) AV nodal blockade Ablation Ventricular tachycardia Re-entry or triggered ICD, Class I & III AADs Ventricular fibrillation Disorganized re-entry ICD, Class I & III AADs Mechanisms of Arrhythmias Enhanced Automaticity • Susceptible tissues include SA & AV nodes, His-Purkinje system, & cells that lack spontaneous pacemaker activity (e.g., ischemic ventricular cells) • Stimuli • Beta-adrenergic stimulation • Hypokalemia • Mechanical stretch Mechanisms of Arrhythmias Triggered Activity Sampson KJ, Kass RS. Chapter 29. Anti-Arrhythmic Drugs. In: Knollmann BC, ed. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill; 2011. http://www.accessmedicine.com/content.aspx?aID=16668361. Mechanisms of Arrhythmias Re-Entry Sanoski CA, Bauman JL. Chapter 25. The Arrhythmias. In: Wells BG, ed. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=7972803. Pharmacologic Approaches to Terminating Tachyarrhythmias 1. Decrease automaticity of ectopic foci 2. Facilitate conduction (shorten refractory period) in an area of unidirectional block 3. Depress conduction (prolong refractory period) in either part of the re-entry circuit http://www.cvpharmacology.com/antiarrhy/sodium-blockers.htm Pharmacology of Antiarrhythmic Drugs V-W class Drugs Ion channel Conduction Velocity Refractory Period Automaticity Ia Disopyramide Procainamide Quinidine Na+ (intermediate) Ib Lidocaine Mexiletine Na+ (fast) / Ic Flecainide Propafenone Na+ (slow) Pharmacology of Antiarrhythmic Drugs V-W class Drugs Ion channel Conduction Velocity Refractory Period Automaticity Ia Disopyramide Procainamide Quinidine Na+ (intermediate) Ib Lidocaine Mexiletine Na+ (fast) / Ic Flecainide Propafenone Na+ (slow) II Betablockers Ca++ (indirect) Pharmacology of Antiarrhythmic Drugs V-W class Drugs Ion channel Conduction Velocity Refractory Period Automaticity Ia Disopyramide Procainamide Quinidine Na+ (intermediate) Ib Lidocaine Mexiletine Na+ (fast) / Ic Flecainide Propafenone Na+ (slow) II Betablockers Ca++ (indirect) III Amiodarone Dofetilide Dronedarone Ibutilide Sotalol K+ http://www.cvpharmacology.com/antiarrhy/potassium-blockers.htm Pharmacology of Antiarrhythmic Drugs V-W class Drugs Ion channel Conduction Velocity Refractory Period Automaticity Ia Disopyramide Procainamide Quinidine Na+ (intermediate) Ib Lidocaine Mexiletine Na+ (fast) / Ic Flecainide Propafenone Na+ (slow) II Betablockers Ca++ (indirect) III Amiodarone Dofetilide Dronedarone Ibutilide Sotalol K+ IV Diltiazem Verapamil Ca++ Drug Bioavail ability (%) Primary Elim Route Half-life CYP substrate CYP inhibition PGP inhibition Amiodarone 22 – 88 Hepatic 15 – 100 d 3A4, 1A2, 2C19, 2D6 2C9, 2D6, 3A4, 1A2, 2C19 Yes Dofetilide 85 – 95 Renal Hepatic 6 – 10 hr 3A4 - No Dronedarone 4 – 15 Hepatic 13 – 19 hr 3A4 2D6, 3A4 Yes Flecainide 90 - 95 Renal Hepatic 10 – 20 hr 2D6, 1A2 2D6 No Ibutilide n/a Hepatic Renal ~6 hr (2 – 12) Unknown Unknown Unknown Lidocaine n/a Hepatic 1.5 – 2 hr 1A2, 3A4, 2C9, 2A6, 2B6 1A2 No Mexiletine 80 – 95 Hepatic Renal 10 – 14 hr 1A2, 2D6 1A2 No Propafenone 11 – 39 Hepatic 3 – 25 hr 1A2, 2D6, 3A4 1A2, 2D6 No Sotalol 90 – 90 Renal 10 – 20 hr - - No Sanoski CA, Bauman JL. Chapter 25. The Arrhythmias. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, eds. Pharmacotherapy: A Pathophysiologic Approach. 8th ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=7972803. Accessed August 7, 2013. Drug Other Effects Adverse Events/Toxicity Amiodarone Contains iodine Beta-blocker CCB Bradycardia, thyroid dysfunction, hepatotoxicity, pulmonary toxicity photosensitivity, GI disturbances Disopyramide Anticholinergic Torsades de Pointes, heart failure, GI disturbances, glaucoma, urinary retention, dry mouth Dofetilide - Torsades de Pointes Dronedarone Beta-blocker CCB Increased creatinine, GI disturbances Flecainide - Ventricular tachycardia, headache, dizziness, visual changes Ibutilide - QTc prolongation, ventricular tachycardia, Torsades de Pointes, hypotension Lidocaine - CNS toxicity, seizures Mexiletine - Lightheadedness, dizziness, anxiety, GI disturbances, tremor, visual changes Propafenone Weak betablocker Ventricular tachycardia, dizziness, GI disturbances Sotalol Beta-blocker Torsades de Pointes, bradycardia, heart failure, bronchospasm ACC/AHA/ESC Guidelines for the Management of Patients with Atrial Fibrillation. J Am Coll Cardiol 2001;38:1266. CAST Investigators. N Engl J Med 1989;321:406-12. Risk Factors for Ventricular Proarrhythmia with Antiarrhythmic Drugs Class Ia & III Antiarrhythmic Drugs Class Ic Antiarrhythmic Drugs Long QTc syndrome (baseline) (> 460ms) Widened QRS (baseline) (> 120ms) Structural heart disease Structural heart disease Bradycardia Rapid ventricular response High doses High doses Excessive QTc prolongation (> 15% from baseline) Excessive QRS widening (> 50% from baseline) Electrolyte deficiencies Low K+ and/or Mg++ Drug Interactions •Diuretics •Other QT prolonging drugs Examples of QTc Prolonging Drugs Psychotropics Anti-infectives • Haloperidol • Risperidone • Ziprasidone • Olanzapine • Quetiapine • Macrolide antibiotics • Quinolone antibiotics • Bactrim • Azole antifungals Antidepressants Quinine • SSRIs • Tricyclic antidepressants Methadone Promethazine Tacrolimus http://www.crediblemeds.org/everyone/composite-list-all-qtdrugs/ Bauman JL. Eur Heart J 2001;3:K93-K100. Common Antiarrhythmic Drug Interactions Avoid/Contraindicated Use caution • QTc prolonging drugs • Amiodarone, Dronedarone • Amiodarone, Dronedarone • Strong CYP3A4 inhibitors • Dofetilide • Verapamil • Cimetidine • Hydrochlorothiazide • Trimethoprim • Warfarin • Statins • Digoxin • Propafenone • Itraconazole • Strong CYP2D6 inhibitors • Ketoconazole • Moderate CYP3A4 inhibitors • Prochlorperazine • Flecainide • Megestrol • Moderate/strong CYP2D6 inhibitors • Propafenone, Flecainide • HIV protease inhibitors Antiarrhythmic Drug Selection for Maintaining Normal Sinus Rhythm No/Minimal Structural Heart Disease Hypertension Amiodarone Dofetilide Heart Failure Substantial LVH ≠ LVH Dronedarone Flecainide Propafenone Sotalol Coronary Artery Disease Amiodarone Dofetilide Sotalol Catheter Ablation Amiodarone Dofetilide Amiodarone Dofetilide Catheter Ablation Wann LS, et al. Circulation 2011;123:104-23.



![Cardio Review 4 Quince [CAPT],Joan,Juliet](http://s2.studylib.net/store/data/005719604_1-e21fbd83f7c61c5668353826e4debbb3-300x300.png)


