basic-monitoring-end-tidal-co2asda-2
advertisement

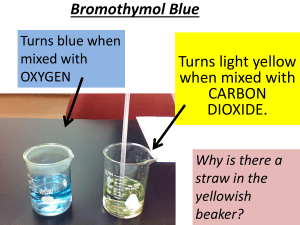
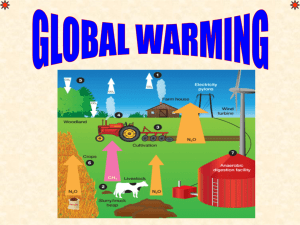
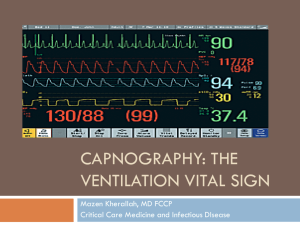
Dr. Jeffrey Elliot Field HBSc, D.D.S. , Diplomat of the National dental Board of Anesthesia, Fellow of The American Dental Society of Anesthesia Carbon dioxide absorbs infrared light with a wavelength of 4.3m m. Light at this wavelength is shone through a gas sample and the absorption is proportional to the carbon dioxide concentration. A sample of expired gas is withdrawn from the anaesthetic circuit by a pump and analyzed inside the machine. Valuable information can be obtained from the continuous measurement of carbon dioxide. At the most basic level the regular rise in carbon dioxide at the end of respiration can be used to determine respiratory rate, and regularity of respiration. 2)The shape of the capnograph (the plot of carbon dioxide against time) is used to assess pulmonary function. The carbon dioxide level should rise rapidly during the first part of exhalation and then flatten off - the "alveolar plateau". If there is pulmonary disease or poor lung perfusion (secondary to poor cardiac output) the alveolar plateau disappears. The level of carbon dioxide at the end of expiration (end tidal carbon dioxide, etCO2) is normally within a few mmHg of the arterial carbon dioxide level and therefore a predictable measure of arterial CO2. EtCO2 is very useful for assessing adequacy of ventilation both during spontaneous respiration and when using a ventilator. EtCO2 is very useful for assessing adequacy of ventilation both during spontaneous respiration and when using a ventilator. But the most important thing ETCO2 tells us in a sedated patient is : ARE THEY BREATHING In an intubated patient ETCO2 will initially confirm proper placement of the endotracheal tube. As the case progresses ETCO2 will continue to confirm that the tube is placed properly and has not moved. Finally the adequacy of ventilation can be continuously assessed. In a sedated patient it is not so much a normal value but a baseline value for that particular patient that we look at. Changes in this baseline value will let us know whether our patient is breathing normally, hyperventilating or hypoventilation. In an intubated patient a normal end tidalCO2 value is 40 mm of mercury. ETCO2 Less Than 35 mmHg = "Hyperventilation" ETC02 Greater Than 45 mmHg = "Hypoventilation" There are two main graphs that we look at which are a function of the sweep speed. At high sweep speed we get a wave form of the CO2 from each breath which is known as the capnogram. There is only one normal shape for a capnogram: At first there is a rapid rise as the dead space gas comes out of the major airways. Then there is a plateau which has a slow rise. Finally there is a rapid decline as the next breath enters the patient. A to B is post inspiration/dead space exhalation, B is the start of alveolar exhalation, B-C is the exhalation upstroke where dead space gas mixes with lung gas, C-D is the continuation of exhalation, or the plateau(all the gas is alveolar now, rich in C02). D is the end-tidal value – the peak concentration, D-E is the inspiration washout. Kinked tube (intubated patients only) Herniated cuff (intubated patients only) Bronchospasm (intubated and non-intubated patients) Any obstruction that limits expiration( eg mucous on the tube, COPD, asthma, foreign body obstruction. Causes1)Unequal emptying of lungs( pnemothorax). Seen in intubated and non-intubated patients 2)Lateral position 3)Tube touching carina Note what happens when the patient stops breathing. The pulse oximeter lags way behind the capnograh in picking up a cessation in breathing.