CDC Rwanda Transition Monitoring Approach - I-TECH
advertisement

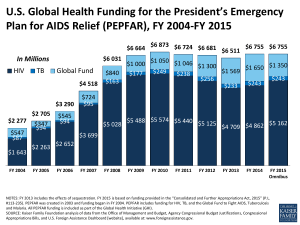
HHS/CDC Track 1.0 Transition in Rwanda Dr Ida Kankindi, Rwanda Ministry of Health Dr Felix Kayigamba, CDC-Rwanda August 2010 1 Rwanda and PEPFAR • 9 million population, 3% HIV prevalence, ~178,680 PLHIV • Major donors for HIV programs include PEPFAR and Global Fund – GF PR: $305 million since 2004 + $247 million for NSA recently awarded – 2010 PEPFAR Budget: $157 million • 2 HHS Track 1.0 partners: ICAP and AIDS Relief • Active, engaged government has led successful HIV program – 96% of pregnant women attending ANC received HIV results via PMTCT (2009) – ~75% of PLHIV in need of treatment with CD4 <350 receive ART (2009) – 1.5 million HIV tests through VCT in 2009 2 PEPFAR Contribution to Rwandan HIV Program, Oct 2008 – Sept 2009 HIV Program Result PEPFARsupported sites National results % support by PEPFAR Pregnant women who received HIV results in PMTCT 132,811 307,245 43% HIV+ pregnant women who received ARV prophylaxis in PMTCT 5,019 8,592 58% HIV+ clients receiving TB treatment 2,253 5,342 42% People counseled and received HIV test results 861,737 1,560,863 55% HIV+ persons currently receiving ART 46,341 73,769 63% 3 HHS Track 1.0 Supported HIV Clinical Services in Rwanda, December 2009 AIDS Relief ICAP TOTAL Health Facilities that provide HIV services 20 56 (47 ART) 76 (60 ART) Health Workers financed through Track 1.0 166 580 746 3,063 18,708 21,771 396 2,079 2,475 8,468 46,664 55,132 301 5,539 5,840 104,000 158,992 262,992 Active Patients on ART Children on ART HIV Patients in Care Women enrolled in PMTCT People counseled and tested at VCT 4 Principles Behind Track 1.0 Transition in Rwanda • ICAP and AIDS Relief are transitioning programs to the Rwanda MOH as the local partner • Emphasis on maintaining quality of care while increasing GOR ownership and management • Quarterly site visits have been linked to already existing PBF quarterly evaluations • Technical support and capacity building from Track 1.0 partners during the whole transition process • Gradual transition approach – Transition one-third of sites during each year (2010, 2011, 2012) 5 MOH Agencies’ Distribution of Responsibilities for Transition Implementing partner activity MOH Agency Mentoring TRACPlus Supervision, UPDC/MOH Decent M&E and Reporting Health Facilities Operations Salaries Districts Performance Based Financing CAAC (via UPDC) (via UPDC) 6 Transition Planning & Implementation Timeframe Planning phase • Establish Transition Task Force • Conduct site readiness assessment • Select 1st 24 sites for transition • Develop M&E plan Implementation phase • Transition sites (~25/yr) • Strengthen MOH capacity to manage and report according to USG requirements • Monitor performance of transitioned sites in collaboration with GOR Mar 2009 – Feb 2010 Mar 2010 – Feb 2012 TRANSITION 7 Rapid assessment of site readiness, November, 2009 • Joint MOH, CDC, ICAP, AIDS Relief visits to 65/76 sites • Completed rapid assessment tool (RAT) – Administrative, managerial, financial aspects with score • Reviewed routine HIV program performance indicators collected quarterly • Reviewed sites for transition based on criteria: – Transition district hospital with associated health centers – Clinical performance indicators: >75% • Discussions within TTF on site selection – 18 sites selected for transition March 2010 – 6 sites selected for transition October 2010 8 120 Readiness Assessment and Performance Indicator Results: District Hospitals and Health Centers Selected for Transition Starting in March 2010 * * 100 80 % * * 60 RAT Score (%) CD4 Recorded 40 ART Retention ARV Refill 20 0 Muhima Gisenyi DH Shyria DH Murunda Kabaya DH Muhororo Kibuye DH Kilinda DH Mugonero Kibogora Bushenge DH DH DH DH DH DH Ngororero ICAP-supported sites Karongi AIDS Relief –supported sites 9 Monitoring and Evaluation of Track 1.0 Transition in Rwanda • Objectives: – Establish baseline level of performance of sites – Monitor any changes in overall performance of sites – Evaluate the quality of clinical services and management capacity of sites throughout the transition process • Methods: – Conduct comprehensive assessment of sites at baseline and at 6, 12 months after transition – Quarterly site visits aim to be integrated with routine supervision through MOH, use routinely collected indicators – Two components: • Capacity assessment survey to monitor overall management • Performance indicators approved by MOH to monitor clinical performance 10 Baseline Assessment Management Results: Health Centers Health Partner Center ICAP AIDS Relief District Hospital Financial Mgt HR Clinical Mgt Supply Chain QI SI Lab Overall Score Color (%) Code Rugarama Muhima 79 PCK Muhima 60 Mwendo Muhima 71 Kabusunzu Muhima 74 Rubengera Kibuye 81 Kirambo Kibuye 73 Mukungu Kibuye 79 Munzanga Kirinda 77 Gatare Kibogora 73 Ruheru Kibogora 76 Karengera Kibogora 76 Kibogora Kibogora 64 Nyamasheke Kibogora 74 Overall average 76% Average Performance of Health Centers in the Muhima DH catchments area 72% Average Performance of Health Centers in the Kibuye DH catchments area 79% Average Performance of Health Centers in the Kibogora DH catchments area 74% Above average Average Below average 11 Baseline Assessment, Clinical Performance Indicator Results: Health Centers Partner Health Center District Hospital New ART initiation N/A Currently on ART ANC partner testing N/A N/A PCK Muhima DH Rugarama Muhima DH 8 187 Kabusunzu Muhima DH 26 Mwendo Muhima DH Rubengera CTX initiation CD4 Control TB screen at ART at 6 mo enrollment retention Pharmacy LTFU pick-up tracing 1.00 0.80 1.00 0.80 0.80 N/A 0.96 1.00 0.95 1.00 0.79 0.79 0.61 277 0.94 0.95 0.89 1.00 0.94 0.94 0.67 51 1108 0.99 0.76 1.00 0.97 0.80 0.80 0.29 Kibuye DH 12 151 0.62 1.00 0.94 1.00 0.97 0.97 0.96 Kirambo Kibuye DH 41 665 0.84 1.00 1.00 1.00 0.93 0.93 0.39 Mukungu Kibuye DH 10 225 0.98 1.00 1.00 1.00 0.81 0.81 0.88 Munzanga Kirinda DH 11 141 0.73 0.57 1.00 1.00 0.91 0.91 0.59 Kibogora HC Kibogora DH 2 152 0.89 1.00 0.80 0.91 0.87 0.87 0.68 Nyamasheke Kibogora DH 35 143 0.78 0.90 0.62 0.97 0.91 0.91 0.50 Karengera Kibogora DH 19 385 0.95 1.00 0.75 0.91 1.00 0.71 0.60 Gatare Kibogora DH 14 262 0.97 1.00 0.50 0.88 0.93 0.47 0.50 Ruheru Kibogora DH 17 298 0.89 1.00 0.56 0.88 1.00 0.67 ICAP AIDS Relief Above average Average Below average N/A 12 Baseline Assessment Dissemination Workshop: Discussions with Districts and Health Facilities 13 Discussion: Impact of M&E for Track 1.0 transition • Detailed review of site performance identified individual sites, clinical, and health systems issues in need of improvement – – – – Supply chain management: ARV stock-outs noted Financial planning and reporting Staffing/HR: insufficient staff at some sites CD4 control and ART retention need improvement in some sites • ICAP, AIDS Relief, MOH, and CDC are now organizing intensive TA to improve these areas in these transitioned sites • Transition M&E process will improve district-level supervision – Linked to performance-based financing for facilities 14 Conclusions • Track 1.0 transition in Rwanda demonstrates country ownership, leadership, management – Inclusive planning involves GOR, USG, partners – M&E builds on existing MOH systems • M&E with feedback to health facilities has led to sitespecific action plans to address clinical and management deficits – MOH also investigating cross-cutting health systems issues: supply chain, personnel 15 Next Steps • MOH, TRAC-Plus, IPs and CDC will collaborate to accomplish the following: • Phase I: • Continue to conduct quarterly assessments in 24 transitioned sites • Phase II: • Readiness assessment for the remaining 52 sites to be transitioned • Conduct baseline assessment for the selected sites • Transition the selected health facilities • Overall: • • • • Address action points derived from dissemination workshop Strengthen MOH financial and administrative capabilities Continue monitoring the quality of services Define long-term plans for technical support 16 Acknowledgments • • • • • • • Health facilities MOH UPDC TRAC Plus ICAP AIDS Relief CDC-Rwanda transition team 17 Thanks Questions/discussion 18