Enthesitis Assessment in Psoriatic Arthritis
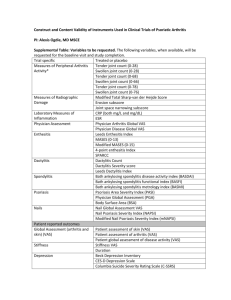
advertisement

Assessment of enthesitis in psoriatic arthritis Philip Helliwell University of Leeds Assessment of enthesitis in psoriatic arthritis – why bother? • Enthesis suggested as hallmark pathoanatomical feature • Clinical and radiological enthesopathy one of distinguishing clinical features for spondyloarthropathy and psoriatic arthritis • Active clinical involvement may reflect general disease activity What instruments already exist? • Mander enthesitis index (MEI) – Mander M, Simpson JM, McLellan A, Walker D, Goodacre JA, Dick WC. Studies with an enthesis index as a method of clinical assessment in ankylosing spondylitis. Ann rheum Dis 1987; 46:197-202. • MASES – Heuft-Dorenbosch L, Spoorenberg A, van Tubergen A, Landewe R, van der Tempel H, Mielants H et al. Assessment of enthesitis in ankylosing spondylitis. Annals of the Rheumatic Diseases 2003; 62:127-132. • SPARCC – Gladman DD, Cook RJ, Schentag C, Feletar M, Inman RI, Hitchon C et al. The clinical assessment of patients with psoriatic arthritis: results of a reliability study of the spondyloarthritis research consortium of Canada. J Rheum 2004; 31(6):1126-1131. • MAJOR – Braun J, Brandt J, Listing J, Zink A, Alten R, Golder W et al. Treatment of active ankylosing spondylitis with infliximab: a randomised controlled multicentre trial. Lancet 359(9313):118793, 2002. Mander (MEI) enthesitis index •Nuchal crests •Manubriosternal joints •Costochondral joints Basic score uses graded response with score range 0-90 Modified score uses binary response with score range 0-30 •Greater tuberosity of humerus •Lateral and medial epicondyles of humerus •Iliac crests •Ant sup iliac spines •Greater trochanter of femur •Medial and lateral condyles of femur •Insertion of Achilles tendons •Insertion of plantar fascia •Cervical, thoracic and lumbar spinous processes •Ischial tuberosities •Post sup iliac spines MASES enthesis index •Reduced number of sites (13) •Removed grading of tenderness (binary response) •Avoided joint margins •Better reliability • 1st Costochondral joints •7th costochondral joints •Iliac crests •Ant sup iliac spines •Insertion of Achilles tendons •lumbar spinous processes •Post sup iliac spines SPARCC enthesis index •8 sites •Not graded •Reliability shown in SPARCC study (Gladman et al. J Rheum 2004; 31(6):1126-1131) •Greater tuberosity of humerus •Insertion of Achilles tendons •Insertion of plantar fascia •Tibial tuberosity MAJOR enthesis index Graded as present/absence of tenderness •Iliac crests •Greater trochanter of femur •Medial and lateral condyles of femur •Insertion of Achilles tendons •Insertion of plantar fascia Reliability of enthesitis indices Results from INSPIRE study Figures are ICC (95% CI) Psoriatic arthritis MAJOR 0.70 (0.5 – 0.89) MASES 0.56 (0.34 – 0.82) SPARCC 0.81 (0.64 – 0.93) Ankylosing spondylitis A new index for psoriatic arthritis • 28 Ss with ‘active’ psoriatic arthritis starting treatment with new DMARDs • All had enthesitis assessed at each of 5 visits over 6 months • MEI (x2), MASES, SPARCC, MAJOR • On final dataset performed data reduction using method of Heuft-Dorenbosch Heuft-Dorenbosch L, Spoorenberg A, van Tubergen A, Landewe R, van der Tempel H, Mielants H et al. Assessment of enthesitis in ankylosing spondylitis. Annals of the Rheumatic Diseases 2003; 62:127-132. A new index for psoriatic arthritis • All MEI entheseal points graded to binary • Frequency tables – entheseal point found to be most frequently tender, noted, and these patients not included in next ‘round’ • Process repeated until 80% assessments included A new index for psoriatic arthritis • 80% of assessments included after just 3 ‘rounds’ – 1st round: right lateral epicondyle (49%) – 2nd round: right medial femoral condyle (70%) – 3rd round: right PSIS, Cx spinous process and left Achilles insertion were equal (80%) • LENIN: right and left lateral epicondyle humerus, right and left medial femoral condyle, right and left AT insertion (max 6) Change in enthesis scores following treatment change 3.5 3 2.5 2 1.5 1 0.5 0 m on th s s Si x m on th h on t Th re e m ne O B as el in e MEI (0.40) MEI mod (1.03) MASES (0.76) MAJOR (1.19) SPARCC (1.05) LENIN (1.19) MEI scores are divided by 10 Relationship between enthesis indices and other measures of disease activity 0.6 Spearman rho 0.4 0.2 MEItotal MASES SPARCC MAJOR LENIN 0 -0.2 -0.4 Values >±0.2 are significant LD I le n Sw ol Te nd e r t VA Sp s hy VA Sp C R P -0.6 Assessment of enthesitis in psoriatic arthritis • Indices developed in patients with ankylosing spondylitis seem to function well in psoriatic arthritis – Repeatability – Responsiveness – Relation to other measures of disease activity • New index derived from psoriatic arthritis population also functions well, although possibly not as well, has good effect size, and is quick and simple to perform The OMERACT filter • Truth – Poor relationship between clinical and U/S detected enthesitis – Juxta-articular position of entheses may lead to confounding with articular pain • Discrimination – All indices able to discriminate between states of low and high disease activity (data not shown) – All indices show good responsiveness and effect sizes • Feasability – LENIN is quickest and easiest but all others, excepting MEI, are also simple to perform Acknowledgements • Rose Hellaby Trust supported Paul Healy • Sanofi-Aventis provided funding for the study and the MRI scans (dactylitis)