ASCO_2013_files/Burtness EG disc ASCO 2013
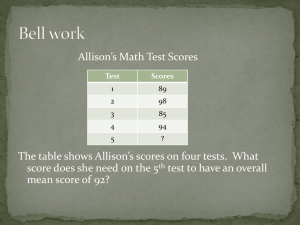
advertisement

Esophagogastric Cancer Barbara Burtness, MD Fox Chase Cancer Center June 3, 2013 Lapatinib in combination with capecitabine plus oxaliplatin in HER2-positive advanced or metastatic gastric, esophageal, or gastroesophageal adenocarcinoma: The TRIO-013/LOGiC Trial JR Hecht, Y Bang, S Qin, H Chung, J Xu, J Park, K Jeziorski, Y Shparyk, PM Hoff, AF Sobrero, P Salman, J Li, S Protsenko, ME Buyse, K Afenjar, T Kaneko, A Kemner, S Santillana, MF Press, DJ Slamon Translational Research In Oncology HER2 in Gastric Cancer • Amplified in 7-34%1 • Amplification may predict resistance to conventional modalities2 OS INT0116 According to Treatment Arm 1. 1. Gravalos and Jimeno. Ann Oncol 2008; 19:1583 2. Gordon M A et al. Ann Oncol 2013;annonc.mdt106 HER2 Directed Therapy in Gastric Cancer ToGA Trial demonstrated survival advantage for addition of trastuzumab in HER2 + gastric cancer1 1. Bang et al. Lancet 2010; 376:687 Comparing Lapatinib and Trastuzumab • Antibody may also exert anticancer activity via recruitment of immune effectors • Interpatient variation in lapatinib drug metabolism and bioavailability is significant – Pharmacogenomic predictors, role of smoking undefined • Markers of resistance – MET associated with lapatinib resistance in HER2 activated gastric cancer cell lines1 – Secondary HER2 mutations described in acquired lapatinib resistance in BrCa2 • Downstream signaling intermediaries – Kras mutation 6%, PTEN loss 15%3 1. Chen CT et al. Mol Cancer Ther. 2012 Mar;11(3):660-9. 2. Kancha RK, et al. PLoS One. 2011;6(10):e26760. 3. Okines et al. Eur J Can 2013; S0959:115 Lapatinib in Gastric Cancer • Lapatinib administered to 47 chemonaive metastatic gastric cancer patients at 1500 mg orally daily1 – PR =9% – Median TTF 1.9 months – OS 4.8 months • Gene expression of HER2, IL-8 and genomic polymorphisms IL-8, and vascular endothelial growth factor correlated with OS 1. Iqbal S, et al. Ann Oncol. 2011;22:2610. OS by gene expression Marker RECIST Response OS median p months EGFR > median 11% 3.3 EGFR <median 0% 5.7 HER2> median 13% 6.8 HER2 <median 0% 3.0 IL-8> median 0% 3.0 IL8< median 17% 5.6 0.24 0.0031 0.016 Iqbal S, et al. Ann Oncol. 2011;22:2610-5 TRIO-013/LOGiC Study Design Day 1: Oxaliplatin 130 mg/m2 Day 1−14: Capecitabine 850 mg/m2, bid 1. Confirmed histology Day 1−21: Lapatinib 1250 mg, qd (one cycle = 21 days) 2. Local/central HER-2+ 3. Confirmed eligibility R Day 1: Oxaliplatin 130 mg/m2 Day 1−14: Capecitabine 850 mg/m2, bid Stratification factors •Prior (neo)Adjuvant therapy Day 1−21: Placebo, qd (one cycle = 21 days) •Region (Asia, North America, Rest of the World) Tumor tissue sent to central lab Primary Efficacy Population (PEP) (HER-2 status confirmed by FISH) Cumulative survival probability Primary Endpoint: Overall Survival (PEP) 1.0 PEP 0.8 Median (95% CI) (mo) 0.6 HR (95% CI) CapeOx+L N=249 CapeOx+P N=238 12.2 (10.6, 14.2) 10.5 (9.0, 11.3) 0.91 (0.73, 1.12) 0.4 0.2 CapeOx+L CapeOx+P 0.0 Subjects at risk CapeOx+L CapeOx+P 0 5 10 249 238 199 189 133 106 15 20 25 30 Time since randomization (months) 83 53 47 34 24 17 9 11 ITT analysis HR 0.91 35 40 45 3 7 3 2 2 Overall Survival: Subgroup Analysis Hazard ratio (95% CI) Primary efficacy population (N=487) 0.91 (0.73, 1.12) Region Asia (n=193) North America (n=17) Rest of World (n=277) 0.68 (0.48, 0.96) 1.61 (0.53, 4.83) 1.04 (0.79, 1.37) Yes (n=38) No (n=449) 1.52 (0.68, 3.41) 0.83 (0.67, 1.04) Age (years) <60 (n=236) ≥60 (n=251) 0.69 (0.51, 0.94) 1.08 (0.81, 1.45) Baseline ECOG status 0−1 (n=444) 2 (n=43) 0.88 (0.70, 1.10) 0.76 (0.41, 1.44) Esophagus (n=20) GE Junction (n=43) Gastric (n=424) 0.87 (0.32, 2.35) 0.90 (0.44, 1.85) 0.89 (0.71, 1.11) Diffuse (n=19) Intestinal (n=436) Other (n=32) 0.64 (0.25, 1.65) 0.93 (0.75, 1.17) 0.58 (0.26, 1.29) Yes (n=373) No (n=114) 0.80 (0.63, 1.01) 1.06 (0.67, 1.68) Prior adjuvant use Primary site Histological type Pylorus intact HER2 status (all FISH+) IHC 0 (n=27) IHC 1+ (n=54) IHC 2+ (n=108) IHC 3+ (n=297) 0.56 (0.24, 1.31) 1.16 (0.61, 2.20) 0.79 (0.50, 1.25) 0.90 (0.69, 1.18) IHC 0−1+ (n=81) IHC 2−3+ (n=405) 0.91 (0.55, 1.51) 0.86 (0.68, 1.09) 0 Favors CapeOx+L 1 2 5 4 3 Hazard Ratio (CapeOx+L / CapeOx+P) Favors CapeOx+P TRIO/LOGIC Vs. ToGA TRIO/LOGIC Chemo Duration ToGA % from Asia Fluoropyrimidine 6 cycles not fixed 40% 50% RR 40 -> 53% 35 -> 47% PFS 5.4 -> 6.0 mo 5.5 -> 6.7 mo OS 10.5 -> 12.2 mo 11.1 -> 13.8 mo HR for HER2 high .86 .65 Conclusions Lapatinib Trial • Lapatinib and capecitabine/oxaliplatin did not lead to a significant survival advantage over capecitabine/oxaliplatin • Impact on RR comparable to trastuzumab • Source of regional differences not clear • Role of markers of resistance – c-MET, EGFR, IL-8 – Can acquired HER2 mutations be identified? • Studies ongoing to assess role of pertuzumab, TDM-1 Stomach Cancer Adjuvant Multi-institutional Trial, SAMIT, Group A phase III randomized clinical trial of adjuvant paclitaxel followed by oral fluorinated pyrimidines for locally advanced gastric cancer –SAMIT StudyK. Yoshida, A. Tsuburaya, M. Kobayashi, S. Yoshino, M. Takahashi, N. Takiguchi, K. Tanabe, N. Takahashi, H. Imamura, N. Tatsumoto, A. Hara, K. Nishikawa, R. Fukushima, A. Kurita, H. Kojima, Y. Miyashita, K. Oba, ME Buyse, S. Morita, J. Sakamoto, Adjuvant Therapy in Gastric Cancer JAMA. 2010;303(17):1729-1737. Adjuvant Systemic Therapy • CA80101 randomized 546 patients to Macdonald (bolus 5-FU/LV, infusional 5-FU RT, bolus 5-FU/LV) vs. ECF-> 5FU/RT -> ECF – ECF did not improve OS [HR 1.03, P = .80] – Toxicity profile favored ECF over bolus 5-FU/LV1 • CLASSIC trial randomized 1035 patients with D2 lymph node dissection to observation or adjuvant capecitabine/oxaliplatin – 3-year DFS 74% on cape/ox vs. 60% for observation 1. Fuchs CS et al. Proc ASCO 2011 [HR 0.56, P<.001] 2. Bang et al. Proc ASCO 2011 Study scheme Randomized phase III, two-by-two factorial design UFT Arm A S-1 Arm B: Control Monotherapy oral FUs 48wks Arm C 48wks Arm D Sequential PTXoral FUs X 3 36wks PTX 80 mg/m2 UFT 267 mg/m2 X 3 36wks S-1 80 mg/m2 DFS: Sequential, CD vs Monotherapy, AB 3yr DFS AB, Mono: 54.0% (95%CI: 50.2-57.6) CD, Seq. : 57.2% (95%CI: 53.4-60.8) Superiority of Sequential HR: 0.92 (95%CI: 0.80-1.07; p=0.273) DFS: UFT base vs S-1 base 3yr DFS AC, UFT base: 53.0% (95%CI: 49.2-56.6) BD, S-1 base : 58.2% (95%CI: 54.4-61.8) Non-inferiority of UFT HR:1.23 (95%CI:1.07-1.43), p = 0.151 Superiority of S-1 HR: 0.81, p = 0.0057 DFS in Each Arms Months SAMIT Conclusions • Sequential taxane -> fluoropyrimidine not superior to fluoropyrimidine monotherapy • 2 x 2 factorial design not optimal for assessing the 2nd component of a sequential regimen – May alter PK, toxicity profile, select for resistance pathways, early progressors are not evaluated • Did not exclude HER2 amplified • Biomarkers of taxane sensitivity should be explored COUGAR-02: Randomised phase III study of docetaxel versus active symptom control in patients with relapsed esophago-gastric adenocarcinoma N Cook, A Marshall, JM Blazeby, JA Bridgewater, J Wadsley, FY Coxon, W Mansoor, S Madhusudan, S Falk, GW Middleton, D Swinson, I Chau, J Thompson, D Cunningham, P Kareclas, JA Dunn, HER Ford On behalf of COUGAR 02 investigators and NCRI Upper GI Clinical Studies Group Trial funded by Cancer Research UK grant CRUK/07/013 EudraCT Number: 2006-005046-37 ISRCTN 13366390 Second Line Therapy of Advanced Gastric Cancer • N=40 compared IRI to BSC1 – PS 0-2 – OS 4 vs. 2.4 m [HR 0.48, p=.012]1 • Phase III of 2nd line chemo (N=133)vs. BSC (N=69)2 – PS 0-1 – OS 5.3 vs. 3.8 m [HR 0.67, p=.007] – No difference between IRI and docetaxel • GRANITE: 439 randomized to everolimus, 217 to placebo3 – Median OS everolimus 5.4 m vs 4.3 m [NS] 1. Thuss-Patience et al. Eu J Cancer 2011; 47:2306 2. Kang et al. J Clin Oncol 2012; 13:1513. 3. Van Cutsem et al. J Clin Oncol 30, 2012 (suppl 4; abstr LBA3) Overall Survival: WJOG n Probability (%) wPTX Median HR (95% CI) 108 p 9.5M CPT-11 111 8.4M 1.13 (0.86-1.49) 0.38 (Months) Number at risk wPTX 108 CPT-11 111 80 75 36 29 10 10 2 3 0 1 0 1 Trial Design Arm A (n=84): Docetaxel 75mg/m2 IV every 3 weeks for up to 6 cycles + ASC Adenocarcinoma of esophagus, esophagus-gastric junction or stomach refractory to platinum and fluoropyrimide Stratified by: Assess every 3 weeks for 18 weeks, then every 6 weeks RANDOMISE 1:1 n=168 Arm B (n=84): Active symptom control May include: Radiotherapy, analgesia, anti-emetics, steroids 1.Disease status (Locally advanced vs metastatic); 2. Site of disease (Esophagus vs GEJ vs Stomach); 3. Time to progression after previous chemotherapy ( 0 vs 0-3 vs 3-6 months); 4. ECOG PS ( 0/1 vs 2) Overall survival 100 Median survival: 5.2 months (95% CI 4.1-5.9) for Docetaxel 3.6 months (95% CI 3.3-4.4) for ASC Hazard ratio 0.67 (95% CI 0.49-0.92), p=0.01 Percentage surviving 75 Docetaxel ASC 50 25 0 0 2 4 6 8 10 12 14 16 10 6 8 2 5 1 18 Months from randomisation No. at Risk: Docetaxel ASC 84 84 69 70 53 38 33 19 25 13 17 9 4 1 Conclusions • Second line therapy extends survival in advanced gastric cancer and is an appropriate standard of care • Docetaxel is an appropriate choice, although toxic in this population • Patient selection based on performance status and peritoneal carcinomatosis may be useful in identifying group of patients in whom this strategy will also be clinically meaningful • Future studies may identify biomarkers to aid selection between taxanes and irinotecan