Regional HER2 - Northern England Strategic Clinical Networks
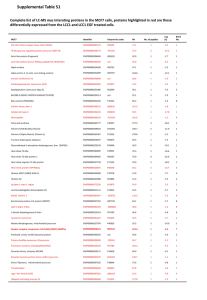
advertisement

North of England Cancer Network HER2 testing Audit Anna Long and Judith Hogarth Cellular Pathology Newcastle upon Tyne Hospitals NHS Foundation Trust We will cover… HER2 testing – an introduction Audit parameters Aims Results Summary Limitations HER2 HER2 is a trans-membrane tyrosine kinase that mediates cell growth and survival HER2 signalling induces cell proliferation Herceptin® binds to HER2 receptors and inhibits proliferation by disrupting HER2 mediated downstream signalling Only those patients that exhibit elevated expression of the HER2 antigen will benefit from treatment Getting the test right is critical! HER2 testing HER2 status is routinely used in breast cancer testing and is recognised as a prognostic and predictive marker. Eligibility for treatment assessed by immunocytochemistry and/or in situ hybridisation IHC 0 1+ Negative 2+ 3+ Equivocal Positive ISH If < 2.0 = Non-amplified If ≥ 2.0 = Amplified NECN HER2 testing At time of audit, undertaken by three centres in the NECN Gateshead Health NHS Foundation Trust (QEH) Newcastle upon Tyne Hospitals NHS Foundation Trust (RVI) North Tees and Hartlepool NHS Foundation Trust (UHNT) Centre Tests referred from IHC method ISH performed? ISH method QEH QEH SRH UHND Dako HercepTest No, referred to RVI N/A RVI RVI CRI NTGH Ventana 4B5 Yes Ventana SISH UHNT UHNT JCUH Ventana 4B5 No, referred to Source BioScience N/A (Vysis FISH at Source BioScience) UKNEQAS All centres performing HER2 testing must participate in the relevant NEQAS HER2 IHC and ISH modules UKNEQAS cite two recommended HER2 testing guidelines: ASCO/CAP (Wolff et al. 2006) UK updated guidelines (Walker et al. 2008) Walker et al. (J Clin Path) Laboratories undertaking tests should be defined by each Cancer Network. UK minimum laboratory workload: 250 IHC cases per annum 100 ISH cases per annum Total HER2 positive cases: 15-17% Total IHC 2+ HER2 cases: average range 18-19% Number of IHC 2+ cases that exhibit HER2 gene amplification: 17-24% Aims of the audit Are centres within the cancer network meeting these standards? Therefore we have established within the NECN: (1) How many tests are performed by each centre (2) The HER2 positivity rate (3) The number of 2+ cases generated by IHC (4) The number of 2+ cases that exhibit HER2 gene amplification Data collected from January 2011-December 2012 inclusive (1) How many tests are performed by each centre Number of IHC tests performed annually 2011 2012 standard 1400 Number of tests 1200 1000 800 600 400 200 0 QE RVI UHNT Centre All centres meet minimum benchmark for IHC tests performed Number of ISH tests performed annually 2011 2012 standard 350 300 Number of tests 250 200 150 100 50 0 QE RVI Source BioScience (UHNT) Centre *Equivocal QE cases stained using SISH at RVI, UHNT cases performed by Source BioScience All centres meet minimum benchmark for ISH tests performed In summary (1) – Minimum number of tests performed All centres satisfy the minimum requirement for number of IHC and ISH tests performed. (2) HER2 positivity rate NECN HER2 profile – positivity 25 20 461/2816 426/2974 % cases 15 10 16.4 14.3 5 0 2011 2012 Year 2011 - Positive vs. negative rates fits within the standard set out by Walker et al (15-17%). 2012 sees this rate drop 0.7% outside this range. Positivity profile for each centre 20.0 18.0 145/794 135/764 145/867 16.0 135/976 181/1185 Quoted range 2006-2007 = 15-17% % cases 14.0 UKNEQAS data 2009-2012= 14.5% 148/1212 12.0 10.0 8.0 17.7 13.7 15.3 12.2 16.7 18.3 2011 2012 2011 2012 2011 2012 6.0 4.0 2.0 0.0 QEH RVI Year by centre UHNT RVI and UHNT fell within the expected positivity range in 2011. QEH rate slightly above expected range in 2011 = 17.7% Both QE and RVI have seen a drop in the positivity rate in 2012 (below 15%) UHNT has shown an increase in positivity rate in 2012 (above 17%). Positivity rates - QEH and RVI QEH 25 60/297 20 48/269 56/362 27/199 60/508 10 5 15.5 11.8 18.1 13.1 20.2 15 5 2011 2012 QEH 2011 2012 2011 SRH Year by referring hospital Positivity rate of cases has dropped across all hospitals (range = 2.4 - 5.0%) 2012 UHND 77/523 53/406 66/495 52/412 30/305 10 17.8 0 51/256 20 % positive cases % positive cases 19/105 15 RVI 25 13.1 12.6 14.7 13.3 19.9 9.8 2011 2012 2011 2012 2011 2012 0 CRI RVI Year by referring hospital NTGH Positivity rate of cases has dropped across all hospitals (range = 0.5 - 10.1%) NTGH positivity rate has more than halved (19.9 – 9.8%) Positivity rates in referring hospitals UHNT 25 63/317 20 % positive cases 63/376 82/477 82/491 15 10 5 16.8 19.9 16.7 17.2 2011 2012 2011 2012 0 JCUH UHNT Year by referring hospital Positivity rate of cases has increased across all hospitals (range = 0.5 - 3.1%) In summary (2) – Positivity rates The NECN as a whole falls below the expected frequency of positive HER2 cases. The audit period spans 2011-2012, however the published literature details HER2 cases from 2006-2007. UKNEQAS data spanning 2009-2012, quotes a positive rate of 14.5%, which means the NECN in fact meets the expected frequency of positive cases. 2/3 referral centres in 2012 fell below 14.5% (QEH and RVI) QEH – all referring hospitals showed a similar decline in positivity rate This would suggest some common factor ?the test itself. RVI - one referral hospital (NTGH) showed a marked decline in positivity rate (19.9-9.8%) This would suggest an upstream factor is responsible for the observed shift. (3) 2+ cases generated by IHC 2+ rate for NECN 22 UKNEQAS data 2009-2012 = 21.7% 20 Av. Quoted range 2006-2007 = 18-19% 18 16 % cases 14 12 10 8 6 15.6 13.9 2011 2012 4 2 0 Year The NECN falls below the quoted range for the whole audit period, and significantly below the UKNEQAS data. 2+ rate for centres UKNEQAS data 2009-2012 = 21.7% 20 209/1230 % 2+ rate 15 112/764 180/1193 10 5 Av. Quoted range 2006-2007 = 18-19% 152/889 123/810 87/986 16.0 8.8 15.1 17.0 17.1 15.2 2011 2012 2011 2012 2011 2012 0 QEH RVI Year by centre UHNT RVI and UHNT have shown <2% variation in 2+ rate. QEH sees a 7.2% decrease % 2+ rates for referring hospitals QEH 18 18/107 16 58/363 14 36/300 % 2+ rate 12 52/518 10 16/199 8 19/269 6 16.0 10.0 16.8 8.0 2011 2012 2011 2012 12.0 7.1 4 2 0 QEH SRH Year by hospital 2011 2012 UHND Fall in 2+ rate observed in all hospitals (range = 4.9 – 8.8%) Most significant decrease seen in SRH cases – more than halved. % 2+ rates for referring hospitals - RVI and UHNT RVI UHNT 25 25 69/312 20 20 88/503 15 63/417 57/409 80/527 64/386 77/501 % 2+ rate % 2+ rate 43/257 10 5 13.9 15.1 15.2 15.4 16.7 49/322 15 74/488 10 22.1 16.6 15.2 17.5 15.2 2011 2012 2011 2012 5 0 2011 2012 CRI 2011 2012 RVI Year by hospital 2011 2012 NTGH Small increase seen in CRI and RVI cases (1.2% and 0.2 % respectively). Significant increase seen in NTGH cases (5.4%) 0 JCUH UHNT Year by hospital Small decrease seen in JCUH and UHNT cases (1.4% and 2.3% respectively). In summary (3) – 2+ rate 2+ rate within NECN falls below the frequency cited in published and UKNEQAS data. RVI and UHNT saw slight (<2%) fluctuations in 2+ rate between 2011 and 2012. QEH showed a 7.2% decrease in 2+ reporting All referring hospitals showed a decrease in 2+ rate (4.9-8.8% fall – SRH rate more than halved). (4) 2+ cases that exhibit HER2 gene amplification Number of 2+ cases that exhibit HER2 gene amplification - NECN 25 Av. Quoted range 2006-2007 = 17-24% 20 70/441 % cases 15 49/406 UKNEQAS data 2009-2012 = 14.7% 10 5 15.9 12.1 0 2011 2012 Year There has been a decline in the number of 2+ cases that exhibit HER2 gene amplification (3.8%). 2+ cases that exhibit HER2 gene amplification by centre 25 % cases 20 53/292 15 16/118 33/288 17/149 18.2 11.5 11.4 13.6 2011 2012 2011 2012 10 5 0 QEH/RVI UHNT Year by centre performing test UHNT HER2 gene amplified cases increased 2.2%. RVI saw a decrease of 6.7% in 2+ cases that demonstrated gene amplification….Why is this? Amplified ISH performed at RVI 40.0 7/19 35.0 13/43 % amplified cases 30.0 25.0 17/80 3/16 20.0 Quoted range 2006-2007 = 17-24% 3/18 9/57 5/36 15.0 11/77 6/58 UKNEQAS data 2009-2012 = 14.7% 8/69 6/63 10.0 0/52 5.0 10.3 0.0 16.7 18.8 13.9 36.8 15.8 9.5 21.3 14.3 30.2 11.6 2011 2012 2011 2012 2011 2012 2011 2012 2011 2012 2011 2012 0.0 QEH SRH UHND CRI Year by referring hospital RVI NTGH There is significant variation in the reporting of HER2 gene amplified cases (range 0-36.8%). Most significant outliers = QEH (decrease of 10.3% to 0% amplified), UHND (increase of 22.1%), NTGH (decrease of 18.6%) Amplified ISH UHNT cases (Source BioScience) 20.0 18.0 11/69 16.0 14.0 12.0 7/64 % 9/85 5/49 10.0 8.0 6.0 4.0 2.0 10.6 15.9 10.9 10.2 2011 2012 2011 2012 0.0 UHNT JCUH Year by referring hospital There is variation in the reporting of HER2 gene amplified cases (range 0.7-5.3%). In summary (4) – 2+ amplified cases There is marked variation in the positivity rate by HER2 gene amplification. Significant outliers QEH (0% amplified 2012) UHND (increase of 22.1% from 2011 to 2012) NTGH (decrease of 18.6% from 2011 to 2012) This may be a symptom of variable 2+ rate by IHC In summary Change in rates 2011 – 2012 by hospital Hospital Change in positivity rate (%) Change in 2+ rate (%) Change in amplified 2+ rate (%) QEH 2.2 6.0 10.3 SRH 5.0 8.8 2.1 UHND 2.4 4.9 22.9 NTGH 10.1 5.4 18.6 RVI 1.4 0.2 7.0 CRI 0.5 1.2 6.3 UHNT 0.5 2.3 5.3 JCUH 3.1 1.4 0.7 Limitations Limiting factors Limitations Pre-analytical Analytical Post-analytical Cold ischaemia time Subjective interpretation Subjective interpretation Core vs excision Chosen HER2 test Staffing Fixation Methodology of test Reporting confidence Processing Staining platforms Decalcification Drying time We need standardisation! Future considerations Look at 2013 data? Thank you Trudy Johnson - QEH Sharron Williams, Jim France – UHNT Merdol Ibrahim - UKNEQAS Immunocytochemistry colleagues, RVI Thank you for listening… Questions? References: Walker et al. HER2 testing in the UK: further update to recommendations. J Clin Path. 2008:61; 818-824. Wolff et al. American Society of Clinical Oncology/college of American Pathologists guideline recommendations for HER2 testing in breast cancer. J Clin Oncol. 2007: 25; 1-28. Ibrahim M. UKNEQAS HER2 audit data. UKNEQAS. 2009-2012. Personal communication.