Subclinical hypothyroidism
advertisement
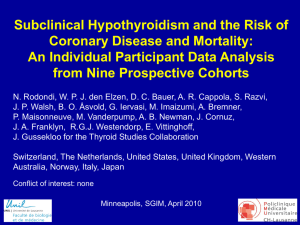
Subclinical thyroid disorders: still a matter of controversy Simon HS Pearce Plan • Background • Subclinical hypothyroidism -Vascular risk • Subclinical hyperthyroidism -Understand the pathophysiology -Approach to Management What is normal? • 16 healthy individuals, having monthly TFTs for 1 year • People stick to their own “reference” interval • Extrapolating to Free T4 values -setpoint +/- ~2.5 pmol/l • “My normal range is different from yours” Andersen et al. JCEM 2002 TSH in centenarians and offspring Δ 232 Ashkenazim, age 97 o 366 of offspring, age 69 177 age-matched controls Atzmon et al. JCEM 2009 Lancet 1971; I: 203 Possible mechanisms • Dyslipidaemia • Cardiac systolic & diastolic dysfunction • Hypertension • Endothelial dysfunction • Hypercoagulability Hard outcomes • Rotterdam Heart Study – Community-based cross sectional survey – 1149 women (mean age 69 +/-7 yrs) – 10.8% had “subclinical hypothyroidism” (TSH>4.0, N FT4) – Odds ratio for MI= 2.3 (CI; 1.3-4.0) – OR for aortic atherosclerosis 1.7 (1.1-2.6) – Population attributable risk of TSH to MI estimated to be 14% • N.B. Diabetes 14%, Smoking 15% Hak et al. Ann Intern Med 2000;132: 270 Meta-summary of meta-analyses • Relative risks (5-95% confidence intervals) Author Number Cardiovascular Cardiovascular All cause events mortality mortality Singh 2008 13,267 1.53 (1.31–1.79) 1.28 (1.02–1.60) 1.12 (0.99-1.26) Ochs 2008 14,449 1.20 (0.97-1.49) 1.18 (0.98-1.42) 1.12 (0.99-1.26) NI NI 1.22 (0.95-1.57) Haentjens 2008 14,619 Razvi 2008 29,022 1.23 (1.02– 1.48) 1.09 (0.84 –1.41) NI Rodondi 2010 55,287 1.18 (0.99- 1.42) 1.14 (0.99- 1.32) 1.09 (0.96-1.24) Thvilum 2012 35,740 NI NI 1.17 (1.00-1.37) Meta-summary of meta-analyses • Relative risks (5-95% confidence intervals) Author Number Cardiovascular Cardiovascular All cause events mortality mortality Singh 2008 13,267 1.53 (1.31–1.79) 1.28 (1.02–1.60) 1.12 (0.99-1.26) Ochs 2008 14,449 1.20 (0.97-1.49) 1.18 (0.98-1.42) 1.12 (0.99-1.26) NI NI 1.22 (0.95-1.57) Haentjens 2008 14,619 Razvi 2008 29,022 1.23 (1.02– 1.48) 1.09 (0.84 –1.41) NI Rodondi 2010 55,287 1.18 (0.99- 1.42) 1.14 (0.99- 1.32) 1.09 (0.96-1.24) Thvilum 2012 35,740 NI NI 1.17 (1.00-1.37) All cause mortality in SCH M Thvilum, F Brandt, TH Brix & L Hegedüs. Nat Rev Endocrinol 2012 Janus response: Age •Thanks to Stefano Mariotti & David Cooper Meta-analysis • Performed by Salman Razvi/ Abdul Shakoor • Longitudinal or cross sectional studies of independent community-based subjects • 14 studies fitted stringent criteria • 2,531 SCH participants • 26,491 euthyroid individuals • Divided studies according to age of inclusion • <65 yr vs 65 and above: median 60 & 74 yr IHD prevalence in cross-sectional studies of SCH & euthyroid controls Younge r Older IHD incidence in longitudinal studies of SCH & euthyroid controls Younger Older Cardiovascular mortality in longitudinal studies of SCH & euthyroid controls Younger Older Summary • Prevalent and incident IHD, and IHD mortality is increased in SCH compared to euthyroid population • Evidence of increased IHD confined to studies that have included people aged less than 65 years Razvi et al. JCEM 2008 Patient-level analysis • 55,287 participants; 3,450 with SCH (6.2%) • Information derived from 11 studies • 9664 deaths; 2168 from CHD • SCH defined as TSH 4.5-19.99 mU/l (N FT4) Rodondi et al. JAMA 2010 Patient-level analysis: TSH Patient-level analysis: TSH Patient-level analysis: Age Interim Summary • Meta-analysis with many thousands of patient events shows vascular death is associated with SCH • Effect is greater at higher TSH levels, reaching significance at TSH of 7.0 mU and above • Effect is attenuated at older ages UK General Practice Research Database • Primary care resource linking ~10 million patient records, labs, prescriptions & death certificates • During 2001 there were 322,291 TSH measurements • Identified 4,735 people >40 yrs with TSH 5.0- 10.0 mU/l, normal FT4 • Excluded individuals on L-T4, ATDs, previous thyroid disease, previous IHD, stroke, other vascular disease Razvi S et al. Arch Intern Med 2012 UK General Practice Research Database • Participants followed until March 2008 (median 7.6 yrs) • People aged 40- 70 yrs (n=3093) and >70 yrs (n=1642) • 52.9% and 49.9% were treated with L-thyroxine during follow up (Primary Care decision) • Analysed outcomes for incident IHD, vascular and all cause mortality over follow up period (Cox regression MVA) L-Thyroxine treated group • 94% of people continued to take L-T4 • Median dose 75μg (12.5-175 μg) daily Untreated group • 1.3% developed overt hypothyroidism -(TSH >10, or FT4) • 58% remained with elevated TSH • 38% reverted to euthyroidism • 2.5% developed low TSH Baseline characteristics 40-70 yrs >70 yrs Untreated L-T4 Rx Untreated L-T4 Rx Number 1459 1634 823 819 Age 55.9 ± 8.3 55.9 ± 8.4 79.9 ± 6.5 79.4 ± 6.2 Females 82.5% 87.4% 75.6% 84.6% Serum TSH (mU/l) 6.3 ± 1.3 6.7 ± 1.4 6.3 ± 1.2 6.8 ± 1.4 Serum FT4 (pM) 13.4 ± 4.4 12.9 ± 3.0 14.6 ± 4.4 13.9 ± 3.4 BMI (Kg/m2) 27.8 ± 5.9 28.1 ± 6.2 25.4 ± 4.6 26.3 ± 5.1 Systolic BP (mmHg) 136.5 ± 20.0 135.2 ± 19.3 149.4 ± 23.5 149.4 ± 22.0 T Cholesterol (mM) 5.86 ± 1.34 5.82 ± 1.21 5.93 ± 1.36 5.95 ± 1.25 Diabetes 18.0% 18.1% 26.9% 26.6% Smokers (current) 18.3% 17.9% 10.9% 10.1% Deprivation index 17.5 16.75 15.86 16.58 GP contacts/yr 1.2 1.3 2.3 2.4 Fatal & non-fatal vascular events 40-70 yrs HR 0.61 (0.39- 0.95); p=0.02 All cause mortality 40-70 yrs HR= 0.36 (0.19 – 0.66) ; p<0.001 Fatal & non-fatal IHD events >70 yrs HR 0.99 (0.59- 1.33); p=0.56 All cause mortality >70 yrs HR= 0.71 (0.56 – 1.08) ; p=0.11 Event rate stratified by age • LT4 vs untreated; Fatal + non fatal CV events Degree of serum TSH elevation • Median serum TSH 6.6 mU/l • Reference group (HR=1) is untreated patients Hazard Ratio for vascular events P value for trend TSH 6.6 or less TSH > 6.6 40-70 yrs 0.62 (0.39-0.96) 0.41(0.26-0.81) 0.007 >70 yrs 1.02 (0.66-1.82) 1.19 (0.74-1.80) NS Razvi et al. Arch Intern Med; 2012 Atrial fibrillation Hazard Ratio for AF/ month 5-95% CI L-T4 exposure 40-70 yrs 0.998 0.995- 1.001 >70 yrs 1.000 0.999- 1.001 Summary • L-T4 treatment of SCH was associated with a lower CV mortality and CV event rate in patients <70 yrs • Importantly, L-T4 treatment was not associated with AF • Not an RCT study, but represents outcome of real-life practice Razvi et al. Arch Intern Med 2012 Who should we treat? • Pregnant patients, or planning pregnancy • Patients with serum TSH > 10.0 mU/l Who should we consider treating? • • • • • Symptoms or signs of hypothyroidism Age less than 70 yrs TSH >7.0 mU/l Goitre High vascular risk including – Ischaemic heart disease – Diabetes – Dyslipidaemia • 380 attendees at ITC 2010 • Electronic voting system • Female, serum TSH 6.8 Pearce, Wemeau, Vaisman. Eur Thyroid J 2012 Subclinical hyperthyroidism What is normal in extreme old age? • Age-related decline in median TSH levels (ill people excluded) Mariotti et al. JCEM 1993 What is normal in extreme old age? • Age related decline in T3 levels (ill people excluded) • FT4 (and TT4) levels remain constant Mariotti et al. JCEM 1993 Magri et al. 2002 Change to function of HPT axis • Reduced hepatic thyroid hormone clearance -glucuronidation, sulfation • Reduced T4 to T3 conversion • Reduced type 1 deiodinase activity • Blunted diurnal TSH secretion • Flattened TSH response to TRH Subclinical Hyperthyroidism Degrees of hyperthyroidism Degrees of hyperthyroidism 12 months follow up 76% returned to normal 87% remained <0.1 Parle JV et al. 1991 Clin Endo Prevalence Both grades • 1-3% of elderly subjects in NHANESIII • 2.1 % in Colorado Health Fair study Suppressed TSH NHANES III • ~0.7% of TFTs from people not on T4 at RVI Evidence Should we be concerned about subclinical hyperthyroidism? Small risk of progression to overt disease • Parle et al. 1991 TSH <0.1 2%/ year • Wiersinga et al. 1995 5%/ year • Pirich et al. 2000 7%/ year TSH <0.1 • Schouten et al. 2011 5-8%/ year • Rosario et al. 2010 TSH 0.1-0.4 1% /year AF in Framingham survey TSH (mU/l) <0.1 0.1- 0.4 >5.0 0.4- 5.0 Sawin et al. NEJM; 1994 Cardiovascular Health Study • 3233 US community dwelling individuals over 65, mean age 73 • AF rate 2.0 (CI 1.3-3.0) in Sub Hyper Cappola et al. JAMA 2006 Overall survival “Circulatory” survival • Community-living >60 year olds; overt thyroid disease excluded Parle et al. Lancet 2001 TSH <0.3mU/l Normal TSH TSH>4.8mU/l • n=558 • Birth cohort design • All 85 yrs at baseline • Leiden, NL • Hazard Ratio per 2.71 mU/l increase in TSH is 0.77 (0.63-0.94) Gussekloo et al. JAMA 2004; 292:2591 CHD (fatal & non-fatal) • 20 yr follow up of population survey, Western Australia; n=2108 • Mean age 51 (17-89); subclin hypER 1.8% • No effect of subclinical hyperthyroidism Busselton Health Study; Arch Intern Med 2005 Meta-analysis of 10 cohort studies • 52,000 participants (2188 with SH) Collet et al. Arch Intern Med 2012 Summary of observational studies • Increased incidence of AF in SH • Increased vascular mortality in SH groups in most, but not all studies • SH sounds like bad news for your heart Functional cardiac effects of subclinical hyperthyroidism • • • • • • • Resting tachycardia LV hypertrophy Increase LV mass index Increase cardiac workload Diastolic dysfunction (impaired relaxation) Increased systolic function at rest Impaired systolic response to excercise Biondi, Kahaly, Klein and others Non-vascular effects of SH Effect Bone mineral density Decreased Reference Mudde 1994, Faber 1998, Tauchmanovà et al. 2004 Fracture Increased x3 & 4.5; hip & vertebral Bauer et al. 2001 Muscle strength Knee extension Decreased by 30% Increased x 3.5 Brennan et al. 2006 Dementia Kalmijn et al. 2000 OK: • Subclinical hyperthyroidism is bad news •Let’s treat everybody and make them better Problem? No evidence that treatment is effective RCTs of radioiodine in SH • Dutch trial: poor recruitment rate, other factors: Trial terminated 2005 • UK Trial: poor recruitment rate (< 10% of SH patients agreed to randomisation). Trial terminated 2009 • French trial: Prof. B Goichot,- ongoing- AF as primary endpoint (target 300 patients) Problem? No evidence that treatment is effective Problems with study designs • Participant cohort defined by a single TSH measurement • AF and mortality followed subsequently • Many subjects (>50%) will have subsequently normalised TSH levels during follow up • How to interpret adverse outcome of low TSH/ Subclinical hyperthyroidism group? Formulation 1 • Low TSH represents true endogenous hyperthyroidism • Adverse cardiac events & AF are an expected consequence of excess thyroid hormones • Need to treat for hyperthyroidism Formulation 2 • Low TSH represents an effect of ageing and reduced turnover of pituitary-thyroid axis (biomarker for age) • Decreased hepatic thyroid hormone clearance, ‘blunted’ diurnal TSH secretion & flattened TSH response to TRH with ageing • Adverse cardiac events & AF (+ OP & dementia) simply are consequences of “biological age” • No need to treat for hyperthyroidism Formulation 1.5 • Both the previous suggestions are true • Adverse cardiac effects are due to excess thyroid hormones in some • In others, low TSH is a biomarker for aging & hence associated with poor outcome • Need to distinguish between these two groups to treat some for hyperthyroidism Cardiovascular Health Study TSH N AF rate/1000 pt yrs mU/l Euthyroid 2502 31 Hazard ratio (5-95% CI) <0.44 47 67 1.98 (1.29-3.03) 0.1-0.44 40 59 1.85 (1.14-3.00) 1.00 (ref) • AF rate little different between grade I and grade II SH Cappola et al. 2006 TEARS study • 2004 patients with SH vs 10,111 controls • 2 TSH measurements 4/12 apart • Median follow up 5.6 yrs Vadiveloo et al. JCEM 2011 What to do? • Observe 3 to 6 months • Look out for drug/ contrast effects -Thyroxine -Opiates -Glucocorticoid -Metformin -L-DOPA -Amiodarone -CT contrast (Iopaque) What to do? Intrinsic thyroid disease Ageing process • TSH <0.1 mU/l TSH 0.1-0.4 mU/l • • Age <75 Age >75 • • Symptoms, goitre No symptoms • • Above median FT3, FT4 Below median FT3, FT4 • • +ve Antibodies, nuclide scan -ve Antibodies, scan • • Complications, AF No complications • Algorithm * Rare causes • Pituitary disease • Tumour hCG † Repeat testing • May need investigations • Maybe yearly re-testing • Maybe never re-test Mitchell & Pearce. Clin Endo 2010 Peer opinion: BTA Survey “There is no reason to treat a patient with subclinical hyperthyroidism for thyrotoxicosis, provided they are in sinus rhythm” Response s Number of responses (%) Strongly agree 7 (2.7) Agree 64 (24.3) Neutral 39 (14.9) Disagree 114 (43.5) Strongly disagree 32 (12.2) Don’t know 6 (2.3) Total 262 (100) 27% agree 55% disagree Vaidya B et al. Clin Endo 2008 Summary • Low serum TSH is common in advanced age • In many, it is transient & in others may be a feature of ageing • The minority will require treatment • Large evidence vacuum remains Dr. Salman Razvi Performed much of the hard work Acknowledgements TRISH Investigators and Steering committee • Amit Allahabadia & Alison Mortimer • Diana Elbourne, Jayne Franklyn, Malcolm Prentice, Graham Williams, Janis Hickey, Murray Stewart, Wilmar Wiersinga Newcastle Co-investigators • Salman Razvi, Anna Mitchell, Joanna Collerton, Andrew Kingston & 85+ Core study team • BTA survey: Bijay Vaidya & Newcastle Healthcare Charity The End