Delayed Cord Clamping
advertisement

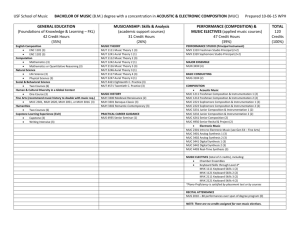
Delayed Cord Clamping T. Flint Porter, MD, MPH Background • Placental transfusion: blood volume transfused to baby after delivery • Umbilical Cord Blood Flow (UCBF) • Factors that influence transfusion − Delayed cord clamping (DCC) − Cord milking (MUC) − Gravity − Uterotonics Purported Advantages • Decreased RDS in preterm neonates • Decrease need for transfusion − (60-80% of < 32 weeks get transfusion) • Less IVH in preterm neonates • Less iron deficiency Mechanisms of DCC and Improved Outcome • Increased neonatal blood volume − Improved perfusion − Reduction in organ injury • Allow spontaneous breathing to begin − Smoother transition of cardiopulmonary and cerebral circulation − Reduce need for resuscitation • Increase iron stores, reduce anemia • Transfusion of blood enriched with stem cells and immunoglobulin Potential Drawbacks • Delayed resuscitation • Increase risk for neonatal hypothermia, polycythemia, hyperbilirubinemia • Increase risk for maternal hemorrhage • Interfere with cord blood collection How long does umbilical cord blood flow continue? • Prospective observational trial of UCBF after delivery in 30 term infants • Protocol − Placed skin-to-skin by CNM − Doppler of straight portion until clamping − Cord clamped at CNM discretion (pulsation) − Pulse cessation determined by researcher − Measurements after 1st breath (30/30) and oxytocin (28/30) Boere et al, Arch Dis Child Fet Neo Ed, 2014 UCBF After Delivery Venous Flow 3/30 (10%) • No venous flow at initial exam 17/30 (57%) • Flow stopped 04:36 (03:03–08:22) • Cord clamped 06:02 (04:47–09:35) 10/30 (33%) • Flow still present when cord clamped 05:13 (02:56–09:15) Boere et al, Arch Dis Child Fet Neo Ed, 2014 UCBF After Delivery Venous Flow Breathing • Flow stopped during deep breaths Crying • Flow stopped • Flow reversed flow with “hard” crying UCBF After Delivery Arterial Flow 5/30 (17%) • No flow at initial exam 12/30 (40%) • Flow stopped 04:22 (02:29–07:17) • Cord clamped 06:15 (05:02–09:30) 13/30 (43%) • Flow still present when cord clamped 05:16 (03:32–10:10) Most flow was toward the placenta UCBF After Delivery Time Differences In 15 infants arterial and venous flow stopped simultaneously 7 infants Arterial stopped first 01:08 (00:51–03:03) 8 infants Venous stopped first 01:43 (00:51–02:45) • Flow to baby • Net flow from baby! UCBF After Delivery Conclusions • UCBF longer than previously described • Complex process affected by − Breathing and crying − Differing arteriovenous flow cessation − Arterial flow toward the placenta • UCBF unrelated to pulsations… reconsider as a time point for cord clamping Term Infants Cochrane 2013 • 15 RCTs of 3911 women > 37 weeks • Clamping Groups 1. < 60 seconds after delivery 2. > 60 seconds after delivery or pulse cessation • Primary outcomes − PP hemorrhage − maternal and neonatal mortality • Secondary outcomes − Maternal blood loss and related morbidity − Neonatal morbidity Term Infants Cochrane 2013 • Severe PPH or mortality • Maternal blood loss • Apgar scores • NICU admission • RDS • Polycythemia Term Infants Cochrane 2013 Hemoglobin (g/dL) Newborn -2.17 g/dL (-4.06 to -0.28) 24 – 48 hours -1.49 g/dL (-1.78 to -1.21) 3 – 6 months No difference Jaundice Phototherapy Clinical jaundice 0.62 (0.41 to 0.96) 0.84 (0.66 to 1.07) ND Term Infants Cochrane 2013 Authors’ Conclusion “Delayed cord clamping is likely to be beneficial as long as access to treatment for jaundice requiring phototherapy is available.” Gravity Vain et al, Lancet, 2014 • RCT in Argentina − All had DCC for 2 mins after NSVD − Introitus vs. Abdomen • Primary outcome was weight − Proxy for volume of placental transfusion • ProcedureDCC − Weighed < 15 secs of delivery − Weighed again at 2 mins after Gravity Vain et al, Lancet, 2014 Introitus (197) Abdomen (194) Mean Weight Change Mean Weight Change Difference P 56 53 3 (–5.8-12.8) NS It doesn’t matter where you hold the baby. Iron and Neuro. Status at 1 Year Andersson, JAMA Ped 2014 • Randomized controlled trial of DCC in full term infants • Groups − Delayed: >180 secs after delivery − Early: < 10 secs after delivery • Outcomes − Ferritin levels at 12 months − Neurodevelopment at 12 months assessed by ASQ (Ages and Stages Questionnaire) Iron and Neuro. Status at 1 Year Andersson, JAMA Ped 2014 Cord Clamping Measure Hb Hematocrit Ferritin DCC (174) ECC (163) P 11.8 12.0 NS 35 35 NS 35.4 33.6 NS Proportion with Iron Status Outside Norm (%) Anemia 16.1 11.6 NS Iron deficiency 3.4 5.4 NS Iron and Neuro. Status at 1 Year Andersson, JAMA Ped 2014 Proportion of infants with low ASQ Scores (%) Cord Clamping ASQ Measure DCC (174) ECC (163) P Communication 3.5 3.6 NS Gross Motor 5.9 4.8 NS Fine Motor 6.5 4.2 NS Problem Solving 4.1 2.4 NS Personal-Social 5.9 4.2 NS DCC in Term Infants • • • • Conclusions Probably not going to hurt… No apparent effect long term Doesn’t matter if you keep the baby below the placenta… Waiting for cord to stop pulsing is as useful as …. Preterm Infants Cochrane 2012 • 15 studies, 738 infants, < 37 weeks • Study Groups − Immediate − Placental transfusion strategies: Delayed (≥ 30 - 120 seconds) Cord milking • Outcomes − Death, severe IVH, PVL, neurodevelopment Preterm Infants Cochrane 2012 • • • • Neonatal death Severe IVH PVL Neurodevelopmental outcome Preterm Infants Cochrane 2012 Secondary Outcomes RR (95% CI) Inotropic support 0.42, (0.23 to 0.77) NEC 0.62, (0.43 to 0.90) Transfusion 0.61 (0.46 to 0.81) Phototherapy 1.21 (0.94 to 1.55) Preterm Infants Cochrane 2012 • • • • • Authors’ Conclusion Less need for transfusion Better circulatory stability Less IVH (all grades) Lower NEC Insufficient data for reliable conclusions about any of the primary outcomes Placental Transfusion in VPN Backes et al, OG 2014 • Systematic review and meta-analysis of DCC and MUC < 32 week neonates (28 wks) • RCTs with the following interventions − Early clamping: < 15 seconds − DCC: at least 20 seconds − MUC: milking at least 3 times • Outcomes − − − − Maternal and obstetric Safety Hematological status Neonatal Outcomes Placental Transfusion in VPN Backes et al, OG 2014 Safety Variables RCT # MD (95% CI) P BP (4 hours) 4 3.24 (1.76, 4.72) <.01 Apgar5 4 -0.07 (-.48, 0.33) NS Temp 3 0.02 (-.18, 0.22) NS Placental Transfusion in VPN Backes et al, OG 2014 Hematologic Outcomes RCT # RR (95% CI) P Transfusion 6 0.75 (0.63, 0.90) <.01 MD (95% CI) Transfusion (#) 6 -1.14 (-2.01, 0.27) <.01 Hematocrit (1st) 10 4.49 (2.48, 6.5) <.01 Bilirubin 8 0.53 (-0.01, 1.07) 0.05 Placental Transfusion in VPN Backes et al, OG 2014 Neonatal Outcomes RCT # Risk Ratio (95% CI) P Total IVH 9 0.62 (0.43,0.91) <.01 Severe IVH 6 0.64 (0.34, 1.21) NS NEC 4 0.55 (0.23, 1.31) NS Sepsis 5 0.73 (0.44, 1.20) NS Mortality 8 0.42 (0.19, 0.95) .04 DCC in Preterm Neonate Elimian et al, OG 2014 • RCT of DCC for neonates 24-34 weeks • Groups − < 5 seconds − > 30 seconds (3-4 passes of milking allowed) • Intention to treat • Primary outcome − Need for transfusion (hb < 10 or symptomatic) • Secondary outcomes − Hematocrit and IVH DCC in Preterm Neonate Elimian et al, OG 2014 Clamping Outcome Delayed (99) Immediate (101) P Transfusion 25 (25.3) 24 (23.7) .80 Anemia 36 (36.4) 48 (47.5) .11 Phototherapy 55 (55.6) 55 (54.5) .89 IVH (grade III) 3 (3.0) 3 (3.0) 1.0 Cord Milking in ELGANs Patel et al, AJOG 2014 • MUC provides benefits of placental transfusion but avoids delay in resuscitation • Cohort study of outcomes < 30 weeks − MUC from 9/2011 – 8/2013 − Historical EGLANs from 1/2010-8/2011 • Composite outcome − IVH, NEC, death before discharge • Improvement in markers of hemodynamic stability MUC in ELGANs Patel et al, AJOG 2014 MUC Procedure • Neonate held 10 cm below level of the placenta • Twisting and nuchal cords released • Milking technique − Pinched close to the placenta − Milked over 2-3 seconds X 3 − Pause for 2-3 seconds between milking − Total procedure < 30 seconds MUC in ELGANs Patel et al, AJOG 2014 Resuscitation Characteristics Variable Historical (160) MUC (158) P Gestation 27.1 27.4 0.10 Birthweight 880 960 0.009 Temp on admit 36.3 36.5 NS 20 (13%) 34 (22%) NS Chest compress. 8 (5%) 10 (6%) NS Intubation (mins) 5 6 NS Surfactant (mins) 29 38 NS Max resuscitation* *blow by oxygen, positive airway pressure, positive pressure MUC in ELGANs Patel et al, AJOG 2014 Neonatal Outcomes < 30 Weeks Variable Control (160) MUC (158) P 45.1 ± 7.4 49.9 ± 5.5 <.01 PRBC 127 (79) 90 (57) <.01 Dopamine <72 51 (32) 28 (18) <.01 NEC* 32 (20) 18 (11 <.05 Severe IVH 27 (17) 15 (10) <.05 Death or IVH 40 (25) 22 (14) <.05 Composite 63 (39) 34 (22) <.01 Hematocrit MUC in ELGANs Patel et al, AJOG 2014 Effect of MUC on Mean BP First Day of Life 45 40 P < 0.01 Control MUC P < 0.01 P < 0.01 35 30 25 20 15 10 5 0 0-6 hours 6-12 hours 12-24 hours DCC with and without MUC Krueger, AJOG 2015 • RCT − DCC: 30 second delay in cord clamping − DCC + MUC (4 times, 4-5 sec. between) • 24 – 31 6/7 weeks − Stratified results by gestational age • Primary outcome: hematocrit • Secondary outcomes − Mortality, days on ventilator, LOS, peak bilirubin, days of phototherapy, “neonatal complications DCC with and without MUC Krueger, AJOG 2015 • No difference in primary outcome − Hematocrit • No difference in secondary outcomes − Bilirubin − Phototherapy − Days on ventilator − Length of stay − Other neonatal morbidities • MUC added nothing to DCC Placental Transfusion Strategies Conclusions for Preterm Babies • Seems to improve short term outcomes − Longer term? • Better for < 30 weeks • Inconsistent findings among latest round of trials − Different protocols • MUC as good as DCC? • “Perinatal medicine is replete with examples of promising interventions the short-term benefits of which did not translate into long-term benefits, including some that caused harm.” Tarnow-Mordi et al, AJOG 2014