Original
Article
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
䡲
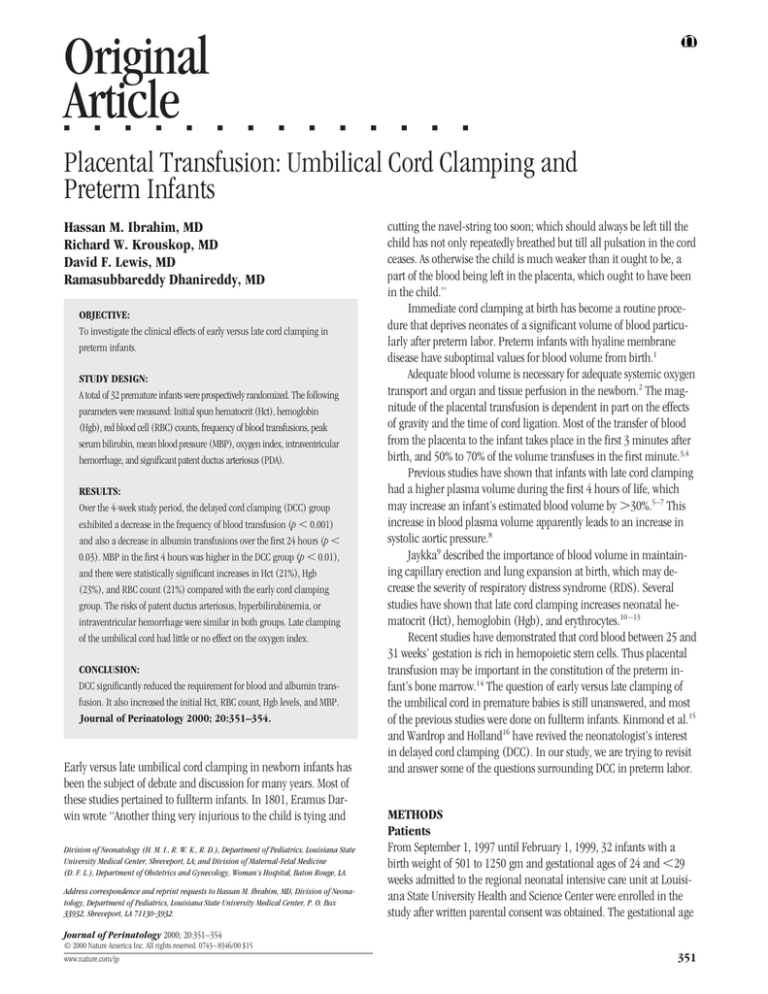
Placental Transfusion: Umbilical Cord Clamping and
Preterm Infants
Hassan M. Ibrahim, MD
Richard W. Krouskop, MD
David F. Lewis, MD
Ramasubbareddy Dhanireddy, MD
OBJECTIVE:
To investigate the clinical effects of early versus late cord clamping in
preterm infants.
STUDY DESIGN:
A total of 32 premature infants were prospectively randomized. The following
parameters were measured: Initial spun hematocrit (Hct), hemoglobin
(Hgb), red blood cell (RBC) counts, frequency of blood transfusions, peak
serum bilirubin, mean blood pressure (MBP), oxygen index, intraventricular
hemorrhage, and significant patent ductus arteriosus (PDA).
RESULTS:
Over the 4-week study period, the delayed cord clamping (DCC) group
exhibited a decrease in the frequency of blood transfusion (p ⬍ 0.001)
and also a decrease in albumin transfusions over the first 24 hours (p ⬍
0.03). MBP in the first 4 hours was higher in the DCC group (p ⬍ 0.01),
and there were statistically significant increases in Hct (21%), Hgb
(23%), and RBC count (21%) compared with the early cord clamping
group. The risks of patent ductus arteriosus, hyperbilirubinemia, or
intraventricular hemorrhage were similar in both groups. Late clamping
of the umbilical cord had little or no effect on the oxygen index.
CONCLUSION:
DCC significantly reduced the requirement for blood and albumin transfusion. It also increased the initial Hct, RBC count, Hgb levels, and MBP.
Journal of Perinatology 2000; 20:351–354.
Early versus late umbilical cord clamping in newborn infants has
been the subject of debate and discussion for many years. Most of
these studies pertained to fullterm infants. In 1801, Eramus Darwin wrote “Another thing very injurious to the child is tying and
Division of Neonatology (H. M. I., R. W. K., R. D.), Department of Pediatrics, Louisiana State
University Medical Center, Shreveport, LA; and Division of Maternal-Fetal Medicine
(D. F. L.), Department of Obstetrics and Gynecology, Woman’s Hospital, Baton Rouge, LA.
Address correspondence and reprint requests to Hassan M. Ibrahim, MD, Division of Neonatology, Department of Pediatrics, Louisiana State University Medical Center, P. O. Box
33932, Shreveport, LA 71130-3932.
cutting the navel-string too soon; which should always be left till the
child has not only repeatedly breathed but till all pulsation in the cord
ceases. As otherwise the child is much weaker than it ought to be, a
part of the blood being left in the placenta, which ought to have been
in the child.”
Immediate cord clamping at birth has become a routine procedure that deprives neonates of a significant volume of blood particularly after preterm labor. Preterm infants with hyaline membrane
disease have suboptimal values for blood volume from birth.1
Adequate blood volume is necessary for adequate systemic oxygen
transport and organ and tissue perfusion in the newborn.2 The magnitude of the placental transfusion is dependent in part on the effects
of gravity and the time of cord ligation. Most of the transfer of blood
from the placenta to the infant takes place in the first 3 minutes after
birth, and 50% to 70% of the volume transfuses in the first minute.3,4
Previous studies have shown that infants with late cord clamping
had a higher plasma volume during the first 4 hours of life, which
may increase an infant’s estimated blood volume by ⬎30%.5–7 This
increase in blood plasma volume apparently leads to an increase in
systolic aortic pressure.8
Jaykka9 described the importance of blood volume in maintaining capillary erection and lung expansion at birth, which may decrease the severity of respiratory distress syndrome (RDS). Several
studies have shown that late cord clamping increases neonatal hematocrit (Hct), hemoglobin (Hgb), and erythrocytes.10 –13
Recent studies have demonstrated that cord blood between 25 and
31 weeks’ gestation is rich in hemopoietic stem cells. Thus placental
transfusion may be important in the constitution of the preterm infant’s bone marrow.14 The question of early versus late clamping of
the umbilical cord in premature babies is still unanswered, and most
of the previous studies were done on fullterm infants. Kinmond et al.15
and Wardrop and Holland16 have revived the neonatologist’s interest
in delayed cord clamping (DCC). In our study, we are trying to revisit
and answer some of the questions surrounding DCC in preterm labor.
METHODS
Patients
From September 1, 1997 until February 1, 1999, 32 infants with a
birth weight of 501 to 1250 gm and gestational ages of 24 and ⬍29
weeks admitted to the regional neonatal intensive care unit at Louisiana State University Health and Science Center were enrolled in the
study after written parental consent was obtained. The gestational age
Journal of Perinatology 2000; 20:351–354
© 2000 Nature America Inc. All rights reserved. 0743– 8346/00 $15
www.nature.com/jp
351
Ibrahim et al.
Delayed V & S Early Cord Clamping in Preterm Infants
Table 1 Neonatal Characteristics
Gestational age (weeks)
Birth weight (grams)
5-minute Apgar score
Sex (F/M)
DCC
(n ⫽ 16)
ECC
(n ⫽ 16)
p value
26.5 ⫾ 0.34
892 ⫾ 5
8 (6–9)†
4/12
26.4 ⫾ 0.4
803 ⫾ 3
6 (5–8)
9/7
0.70ⴱ
0.20ⴱ
0.001
0.07‡
ⴱMean ⫾ SEM.
†The range is shown in parenthesis for 5-minute Apgar score.
‡-squared analysis.
estimate was based on the following: fetal ultrasound scan, dates in
the prenatal record or from maternal interview, and the neonatologist’s examination in the delivery room.
Infants were randomized immediately before the vaginal delivery
to either DCC or early cord clamping (ECC) groups. Infants were
randomized to DCC or ECC groups by numbers placed in sealed envelopes. Cases in which there was an infant with major congenital
anomalies, twin-to-twin transfusion, maternal diabetes, placenta
previa, placenta abruption, or a maternal history of drug abuse were
not eligible for the study.
In the DCC group, a nurse or physician would time 20 seconds by
stopwatch, starting with complete delivery of the infant (the infant is
completely out of the birth canal). During this time the attendant
held the infant supine at the level of the introitus, then immediately
clamped the cord at the 20-second timepoint.
A total of 32 premature infants were eligible for the study (16
babies in each group). The characteristics of these infants are shown
in Table 1.
The primary outcome measure was the total number of corrected
blood transfusions over the 4-week study period; initial spun Hct, Hgb,
and red blood cell (RBC) counts were measured in venous blood
samples obtained at 3 to 4 hours after birth. Other measures included
Apgar score at 5 minutes, maximum serum bilirubin and the day of
its peak, clinically significant patent ductus arteriosus (PDA), intraventricular hemorrhage (IVH), and respiratory impairment assessed
by oxygen index (O.I.) (O.I. ⫽ mean airway pressure ⫻ FIO/postductal PO2) at 4 and 24 hours after birth. The attendant physician, who
was not aware of the grouping of the infants, would order the blood
transfusion (15 ml/kg of packed RBC) if the baby’s spun Hct was
ⱕ40% and required supplemental FIO2. The infant was also transfused if he or she was symptomatic (tachycardia, tachypnea, apnea)
with a Hct of ⱕ30% and breathing room air.
During the 4-week study period, every blood sample withdrawn
for any required laboratory tests was measured and recorded. The total
volume of the blood that was withdrawn was calculated and was used
to correct the number of blood transfusions over the first 4 weeks of
life. The following equation was used: ([total volume of blood transfused ⫺ total volume of blood withdrawn]/average body weight
(kg)) ⫻ 15.
352
Mean blood pressure (MBP) measured by DINAMAP model 18465⫻
(Critikon, Tampa, FL) (vital signs monitor) was obtained at 4 hours
after birth, and an albumin transfusion (15 ml/kg) was given if the
MBP was ⱕ30 mm Hg within the first 24 hours of birth. A head ultrasound was performed on all infants at day 3 and day 7 of life to detect
IVH. An echocardiogram was obtained for infants with clinical signs
of PDA by a staff cardiologist who was unaware of the group assignment of the infants.
Statistical Analysis
Sample sizes of 16 infants in each group were necessary to detect a
decrease in the mean number of blood transfusion by 30% with a
power of 80% and ␣ of 5%. The Student’s t-test for two independent
samples was used to compare the mean values in the DCC and ECC
groups. For nonparametric variables, -squared and Fisher’s exact
tests were used.
RESULTS
A total of 32 premature infants were eligible for the study entry between June of 1997 and February of 1999. There was no statistical
significance in the mortality between the two groups. One infant in
the DCC group died at day 14 due to necrotizing enterocolitis complications. Two infants in the ECC group died at days 9 and 12 of respiratory failure and necrotizing enterocolitis, respectively. The primary
outcome measures of those infants who died during the study were
not included in the data analysis. The mean birth weight, gestational
age, and male to female ratio in both groups were similar, but there
were significant differences between the two groups with regard to
5-minute Apgar scores (Table 1).
A total of 12 infants (75%) in the DCC group and 14 infants
(87%) in the ECC group developed RDS ( p ⬍ 0.36). All infants with
RDS in both groups were intubated and placed on assisted ventilation.
The MBP in the DCC group was higher at 4 hours of life ( p ⬍
0.01). Four infants (25%) required albumin transfusion in the DCC
group to stabilize their blood pressure and to increase tissue perfusion
during the first 24 hours of life compared with 9 infants (56%) in the
ECC group ( p ⬍ 0.03). The O.I. at 4 hours and 24 hours in both
groups was comparable ( p ⬍ 0.74, p ⬍ 0.15). The mean peak serum
bilirubin and the day of maximum concentration were comparable in
both groups (6.6.vs 6.2, p ⬍ 0.56) There were two infants with IVH in
the DCC group compared with four infants in the ECC group ( p ⬍
0.38). In addition, there were four infants with significant PDA in the
DCC group compared with six infants in the ECC group ( p ⬍ 0.44)
(Table 2).
The initial mean spun Hct, Hgb, and RBC counts were higher in
the DCC group compared with the ECC group (21%, 23%, and 21%
higher, respectively). During the 4-week study, all 12 infants in the
ECC group received RBC transfusion compared with 9 in the DCC
group ( p ⬍ 0.03). Of the 12 ventilated infants in the DCC group, 8
required at least one red cell transfusion compared with 12 of the 14
infants ECC group ( p ⫽ 0.36). A total of 4 of 11 infants (36%) in the
Journal of Perinatology 2000; 20:351–354
Delayed V & S Early Cord Clamping in Preterm Infants
Ibrahim et al.
Table 2 Secondary Outcomes in the Study Groups
Ventilated
MBP (4 hours) (mm Hg)
No. of patients receiving albumin
(24 hours)
O.I. (4 hours)
O.I. (24 hours)
IVH (n)
PDA (n)
Table 3 Hematological Results in the Two Groups
DCC
(n ⫽ 16)
ECC
(n ⫽ 16)
p value
12
36 ⫾ 1
4
14
31 ⫾ 1
9
0.36ⴱ
0.01†
0.03ⴱ
5.7 ⫾ 0.9
2.6 ⫾ 0.4
2
4
6.5 ⫾ 1.1
9 ⫾ 0.5
4
6
0.74†
0.15†
0.38‡
0.44‡
ⴱ-squared analysis.
†Mean ⫾ SEM.
‡Fisher’s exact test.
ventilated DCC group required multiple blood transfusions compared
with 10 of 12 (83%) in the ECC ventilated group ( p ⫽ 0.03). The
mean number of blood transfusions in the DCC group was significantly lower (1.2) compared with the ECC group (3.6) (Table 3).
DISCUSSION
The question of early versus late umbilical cord clamping is still a
controversial issue, especially due to the greater emphasis on the
problems of excessive placental transfusion (hyper-bilirubinemia,
polycythemia, and hypervolemia), but most past studies were done on
fullterm infants. Preterm infants with hyaline membrane disease have
low blood volume, and immediate cord ligation may deprive premature infants of a significant blood volume.
Our study has shown that DCC increases placental transfusion.
Our study was small so as to detect differences in the incidence of IVH,
PDA, or hyperbilirubinemia. No infants in the DCC group developed
polycythemia. This increase in placental transfusion led to a significant increase in initial Hct, Hgb, and RBC counts in the DCC group.
The finding that the DCC group had higher Apgar scores at 5 minutes
may be due to an increase in blood volume, an increase in MBP, or
both. Our study showed that DCC not only decreased RBC transfusion
during the study period but also maintained normal MBP and significantly decreased the need for albumin transfusion during the first 24
hours of life.
The decrease in the blood cell transfusion requirements in the
DCC group may be due to the increase in the initial mean Hgb concentration, RBC counts, and the abundance of hemopoietic stem cells
in the cord blood.
Hofmeyr et al. showed that there was a decrease in the incidence
of IVH in infants delivered at ⬍35 weeks’ gestation after 1 minute of
DCC.17 In our study, there was also a trend toward a decrease in the
incidence of IVH in the DCC group (13%) versus the ECC group
(28%), but that difference was not statistically significant.
Although there was a significant increase in the RBC counts
of 21%, we could not find any significant difference in the peak
Journal of Perinatology 2000; 20:351–354
Mean initial RBC (10 l)
Mean initial Hct (%)
Mean Hgb (gm/dl)
Mean no. of blood transfusions
Mean peak serum bilirubin
(mg/dl)
DCC
(n ⫽ 16)
ECC
(n ⫽ 16)
p value
4.4 ⫾ 0.1
50.3 ⫾ 1.3
16.8 ⫾ 0.4
1.2 ⫾ 0.4
6.6 ⫾ 0.4
3.5 ⫾ 0.7
39 ⫾ 1.4
12.9 ⫾ 0.6
3.6 ⫾ 0.5
6.2 ⫾ 0.4
0.003ⴱ
0.01ⴱ
0.0002ⴱ
0.001ⴱ
0.56ⴱ
ⴱStudent’s t-test for two independent samples.
and the day of maximum bilirubin concentration between the two
groups.
Several studies have suggested that DCC decreases the incidence
of RDS, while others failed to reproduce the same results.18 –20 Our
sample size was small enough to detect a difference in the incidence
or the severity of RDS between the DCC and ECC groups.
In summary, a 20-second delay in cord clamping with the infant
held in a supine position at the level of introitus did decrease the
number of blood transfusions during the first 4 weeks of life. It was
also associated with higher Apgar scores, Hgb levels, RBC counts,
more stable blood pressure, and fewer albumin transfusions in the
first 24 hours of life. The reduction in red cell transfusions in the DCC
group lessened the risk of transfusion complications and the cost of
blood transfusion.
References
1. Brown EG, Krouskop RW, McDonnell BS, Sweet AY. Blood volume and blood
pressure in infants with respiratory distress. J Pediatr 1975;87:1133– 8.
2. Jones JG, Holland BM, Hudson IR, Wardrop CA. Total circulating red cells versus
hematocrit as the primary descriptor of oxygen transport by the blood. Br J
Haematol 1990;76:288 –94.
3. Lind J. Physiologic adaptation to the placental transfusion. Can Med Assoc J
1965;93:1091–100.
4. Duckman S, Merk H, Lehmann WX, et al. The importance of gravity in delayed
ligation of umbilical cord. Am J Obstet Gynecol 1953;66:1214 –23.
5. Oh W, Blankenship W, Lind J. Further study of neonatal blood volume in relation
to placental transfusion. Ann Paediatr 1966;207:147–59.
6. Usher R, Shepard M, Lind J. The blood volume of the newborn infant and placental transfusion. Acta Paediatr Scand 1963;52:497–512.
7. Yao AC, Lind J, Tiisala R, Michelsson K. Placental transfusion in the premature
infant with observation of clinical course and outcome. Acta Paediatr Scand
1969;58:561– 6.
8. Buckels LJ, Usher R. Cardiopulmonary effects of placental transfusion. J Pediatr
1965;67:239 – 47.
9. Jaykka S. Capillary erection and lung expansion. Acta Paediatr Scand 1958;47:
484 –500.
10. Lanzkowsky P. Effects of early and late clamping of umbilical cord on infant’s
hemoglobin level. BMJ 1960;273:1777– 87.
353
Ibrahim et al.
Delayed V & S Early Cord Clamping in Preterm Infants
11. Moss AJ, Monset-Couchard M. Placental transfusion: early versus late clamping
of the umbilical cord. Pediatrics 1967;40:109 –26.
16. Wardrop CA, Holland BM. The roles and vital importance of placental blood to
the newborn infant. Acta Paediatr Scand 1966;55:38 – 48.
12. Siddle RS, Richardson RP. Milking or stripping the umbilical cord: effect on
vaginally delivered babies. Obstet Gynecol 1953;1:230 –3.
17. Hofmeyr GJ, Bolton KD, Bowen DC, Govan JJ. Periventricular/intraventricular
hemorrhage and umbilical cord clamping. S Afr Med J 1988;73:104 – 6.
13. Oh W, Lind J. Venous and capillary hematocrit in newborn infants and placental
transfusion. Acta Paediatr Scand 1963;52:497–512.
18. Usher RH, Saigal S, O’Neill A, Surainder Y, Chua L. Estimation of red blood cell
volume in premature infants with and without respiratory distress syndrome. Biol
Neonate 1975;26:241– 8.
14. Clapp DW, Baley JE, Gerson SL. Gestational age-dependent changes in circulating hematopoietic stem cells in newborn infants. J Lab Clin Med
1989;113:422–7.
15. Kinmond S, Aitchison TC, Holland BM, Jones JG, Turner TL, Wardrop CA.
Umbilical cord clamping and preterm infants: a randomized trial. BMJ
1993;306:172–5.
19. Frank DJ, Gabriel M. Timing of cord ligation and newborn respiratory distress.
Am J Obstet Gynecol 1967;87:1142– 4.
20. Taylor PM, Bright NH, Birchard E. Effect of early versus delayed clamping of the
umbilical cord on the clinical condition of the newborn infant. Am J Obstet Gynecol 1963;86:893– 8.
From Drawings from the Newborn by Heather Spears, with permission of Ben-Simon Publications, PO Box 318, Brentwood Bay, BC, Canada V8M 1R3
354
Journal of Perinatology 2000; 20:351–354