Endoscopic siunus surgery (ESS)& Complication
advertisement
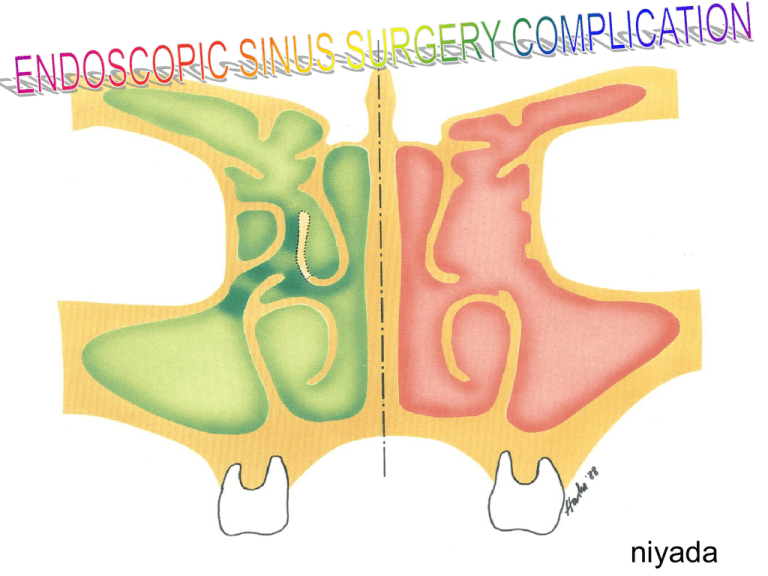
niyada Prevention • Avoid dangerous cases : revision, massive diseases, bleeding tendency • Pre op. CT scan, CT aid ESS • Pre op. preparation • Intra op. observation • Post op. care Intra-operative observation • • • • • • Sedation, Hypotensive anesthesia Draping, Eye observation CT review Bulb press test Be careful ; Microdebrider, Over packing Image-guided ESS Hemorrhage Minor hemorrhage • Common and require minimal intervention • Mucosal cause • Tendency to bleeding in long term local steriod use / Post infection Minor hemorrhage • Treatment – Cotton soaked with epinephrine – Packing – Local Electrocautery Minor hemorrhage • Prevention – Adequate prepare nasal mucosa with vasoconstrictor – Avoid tearing mucosa – Meticulous and careful dissection – Good quality sharp or non-tearing instrument – Gently and non-traumatizing packing Major hemorrhage • Anterior ethmoidal artery – Usually in bony canal but can be dehiscense – Bipolar cauterization and packing Major hemorrhage • Sphenopalatine artery – Posterior septal branch and branch to MT – Related to the MT removal – High pressure Sphenopalatine artery Major hemorrhage • Cauterization or endoscopic ligation Internal carotid artery injury • Rare and high mortality • Risk in surgery of sphenoid sinus and posterior ethmoid air cell • ICA locate on lateral wall of sphenoid sinus • Dehiscence of the bony canal about 23 % Management Prevention • Assess distance with measured probe Prevention • Avoid trauma to intersphenoid septum • Sphenoidotomy should be performed inferomedial • Not blind manipulate in sphenoid sinus Orbital complications Orbital complications • • • • • Orbital hematoma Blindness Diplopia Nasolacrimal duct injury Subcutaneous emphysema Predisposing factors • • • • • • • Dehiscence of LP Revision surgery Distorted anatomy Sphenoethmoidal cell (Onodi cell) Extensive nasal polyp General anesthesia Bony destructive lesion Predisposing factors • • • • DNS Concha bullosa Lateralized paradoxical turbinate Hypoplastic maxillary sinus “ Uncinate process close to LP ” Orbital hematoma • Occur intra-op until postop 10 hr. • High potential to blindness • Cause – Ant. ethmoidal artery injury and retracted into orbit : sudden raise in IOP – Vein lining the LP tearing : slow progress hematoma Orbital hematoma • Hematoma produce pressure on central retina artery • Retinal ischemia persists >90 min. cause blindness Orbital hematoma • Symptoms & signs – Eye pain – Rapid proptosis – Ecchymosis usually at medial first – Subconjunctival hemorrhage • Symptoms & signs – VA drop or blindness – Marcus Gunn’s pupil Orbital hematoma • Treatment – Aim to relieve pressure on arterial supply of optic nerve – Reverse from GA – Ophthalmologist consultation – Conservative treatment – Medical treatment – Surgical treatment Conservative treatment • • • • • Remove nasal packing Stop bleeding in the sinus Head elevation Control Blood pressure IOP measurement q 5-10 min. • Orbital massage (contraindicate in previous eye surgery) Medical treatment • Indicate in elevated IOP and VA drop • 20% Mannitol 0.5-1 mg/kg IV. drip in 20-30 min. – Osmotically drawing fluid out of orbital space – Early onset of action Medical treatment • Azetazolamide 500 mg. IV – Decrease aqueous humor production – Delayed onset of action • Avoid Fimolol or Pilocarpine (masking pupil exam) • Systemic steroid (controversy) – Dexamethasone 1 mg/kg then 0.5 mg/kg q 6 hr Surgical treatment • Indicate in conservative failure • Lateral canthotomy and inferior cantholysis Surgical treatment • Orbital decompression – External ethmoidectomy – Endoscopic approach • Optic nerve decompression (last choice)