RATIONAL USE OF ANTIBIOTICS
RATIONAL USE OF
ANTIBIOTICS
R. Anita Indriyanti
Pharmacological Department
Bandung Islamic University
References :
1. Lippincott’s Illustrated Reviews :
Pharmacology, 2 nd ed
(Chapter 28)
2. Buku Pedoman Kuliah Farmakoklinik
Farmakologi III
Jilid 1 edisi 2
Prof. DR. Herri S. Sastramihardja, dr.,
SpFK
A medical doctor has to know the definite clinical pharmacology of antibiotics, how to select and use them rationally.
30% of inpatient individuals has been given antibiotics
Side effect
Definition AB
Resistance
Ideal antibiotics
In vitro
Classification
Spectra
Chemical structures
Mechanism of action
DEFINITION
AB are chemical substances obtained from microbes/microorganisms (bacteria, fungi, actinomycetes) that able to inhibit or eradicate the growth of the other microorganisms.
Antimicrobial all antiinfections semisynthetic synthetic nature antibiotics
IDEAL ANTIBIOTICS CRITERIA
1.
Most selective, most effective to infectied microorganisms
2.
More bactericidal effect in the site of action
3.
Antibacterial effect is not interfered by body fluid, exudate, plasma protein or enzymes and persist for a long duration in the blood
4.
Minimal toxicity
5.
Resistance develops slowly
6.
Given by any route
7.
Reachable cost
In vitro
1. Primary bacteriostatic effect inhibit the growth of m.o
Sulfonamide, tetrac, chloramph, erythromycin (low concentration), lincomycin, clindamycin and fusidic acid
2. Primary Bactericidal Effects
Eradicate/kill
Pen, cef, aminoglic, erythromycin (high concentration), cotrimazol. Rifampisin and vankomycin.
Those classification is not absolute but relative
SPECTRUM OF AB EFFECTS
1. Narrow spectrum antibiotics (NSAB)
Main effect : sensitive for gram positive bacteria and bacil e.g. : Pen. G, Pen. Resistent penicillinase semisynthetics, bacitracin, macrolides, lincomycin, vancomycin
2. Broad Spectrum Antibiotics (BSAB)
Main effect : sensitive for gram positive and gram negative bacteriae e.g. : Pen. (ampicillin and amoxycillin), cefalosporins, tetracyclins, chloramphenicol, trimetroprim and sulfonamides
Widely used of BSAB an umbrella in treating the unidentified bacterial infection
resistance
RESISTANCE and
MECHANISM OF ACTION recall in microbiology
SIDE EFFECTS
1.
ALLERGIC REACTION
2.
TOXIC REACTION
Direct effects in unproper dose e.g. : aminoglycosides
3.
SUPERINFECTION : new infection caused by pathogen microbes or fungi during AB therapy to primary infection.
SUPERINFECTION : frequent potentially harmed risk
Causa : Enterobacter, Pseudomonas,
Candida and other fungi. Those agents are difficult to be eradicated by today available antibiotics.
AVOIDING SUPERINFECTION
1.
Stop the giving antibiotics
2.
Treatment according to bacterial identification and sensitivity test
The specimen was taken from feces and secretion of upper respiratory tract, to be analyzed
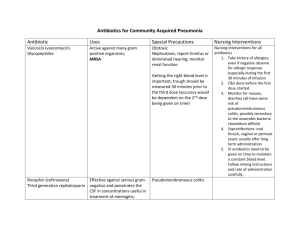
RATIONAL THERAPY OF ANTIBIOTICS
ANTIBIOTICS
HOST
PHARMACOKINETICS
PHARMACODINAMICS
CHARACTERISTIC
OF ANTIBIOTICS
HOST ASPECTS
BIOCHEMICAL &
PHYSIOLOGICAL &
PATHOLOGICAL
CONDITIONS
DEFINITION OF RATIONAL USE OF
ANTIBIOTICS (WHO)
PROPER INDICATION
PROPER DRUG
PROPER DOSAGE
SE MONITORING
RATIONAL USE OF AB
PROCEDURES
STEPS TO PROCEDURES
Define the patient problems specify the therapeutic objectives
Verify the suitable of your personal treatment
Start the treatment
Give information, instruction and warning
Monitoring and stop treatment
Clinical diagnosis
Identification, sensitivity test of bacteria
Pharmacodynamics
Pharmacokinetics
Host factors
RATIONAL USE OF ANTIBIOTICS
PREVENTION IN HIGH
SUSCEPTIBILITY TO
GET INFECTION
PROPHYLAXIS
THERAPY
M.O
ERADICATING
DEFINITIVE THERAPY
EMPIRIC THERAPY
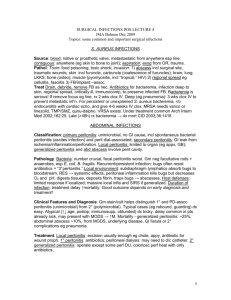
IN NON SURGICAL CONDITIONS
IN SURGICAL CONDITIONS
DEFINITIVE THERAPY
It is the most effective, least toxicity and the narrowest selection
Based on :
* identification of bacteria
* sensitivity test
* interpretation in the content of the overall clinical picture
* the AB of choice directed to M.O
EMPIRIC AB THERAPY
Giving AB directly without identification and sensitivity test of bacteria, but…… obtaining specimen for lab. analysis before giving AB.
Empiric AB therapy based on local epidemiological data :
What is the pathogen M.O potentially infected
AB given based on susceptibility pattern
Initiated after obtaining specimen
Started with AM combination or single
BSAB
SELECTING AB IN EMPIRIC THERAPY
The site of infection
There are barriers inside the body : brain, prostate, bone
Other : foreign bodies local factors
Patient’s history :
PATIENT HISTORY
Age baby, child, adult, old age !
Immune system immunocompromised!
Who?
Renal dysfunction accumulation! How ?
Hepatic dysfunction metabolism! How ?
Genetic factors G6-PD. Attention, contraindication !
Pregnancy teratogenic, embryogenic
Lactation vulnerable AB for new born
INDICATION IN EMPIRIC THERAPY
Infection of unknown origin
Neutropenic patients
Characteristic symptoms of meningitis
MISUSE of AB :
Treatment of untreatable infection
Therapy of fever of unknown origin
Improper dosage
Inappropiate reliance on AB alone
Lack of adequate bacterial information
STRATEGIC FOR EMPIRIC THERAPY
Empiric therapy :
Coverage by a combination of antibiotics such as
Clindamycin plus gentamycin
Effective against gram positive, gram negatives and anaerobes
Or
A single broad spectrum AB
Such as imipenem/cilastatin
Receive culture report
With sensitivities
If gram positive only
↓
Continue gram pos.
Coverage, discontinue
Gram neg. and anaerobic
Coverage if mixed
↓ continue therapy as initiated
If gram negative only
↓
Continue gram neg.
coverage, discontinue
Gram pos. and anaerobic
Coverage
Chapter 28, Fig.28.1 Lippincott’s ed.2
nd
If anaerobic only
↓ continue anaerobic coverage, discontinue gram positive and gram negative coverage
PROPHYLAXIS
SURGICAL
1.
Contaminated op.
2.
Clean – contaminated op
3.
Selected op may suffer post-op.infection
NON SURGICAL
PREVENT :
1. Streptococcal infection in patient with a history of
RHD
2. In pre-dental extraction who have implanted prosthetic devices
3. TB/meningitis in close contact individual
4. Protect fetus from infection in HIV-infected pregnant woman
Common Error in AB prophylaxis
1.
Selection of wrong AB
2.
The initial therapy too early or too late
3.
Excessive duration
4.
Inappropriate use of BSAB
DISADVANTAGES TO PROPHYLACTIC
AB
1.
Toxic/allergic reaction
2.
Superinfection with more resistant flora
3.
The infection may be temporarily masked
4.
Ecology of the hospital flora may be altered
COMMON CAUSES OF FAILURE OF AB
THERAPY
DRUGS : ө inappropriate drug ө inadequate dose ө improper route of administration ө accelerated inactivation ө poor penetration
HOST : ө poor host defence ө undrained pus ө retained infected foreign bodies ө crusta/necrotic tissues
Cont.
- Pathogen ө drug resistence ө superinfection ө dual infection initially
- Laboratory : ө erroneous report of susceptible pathogen
AB – COMBINATION
Synergisme (3) :
1) Blockade of sequential steps in a metabolit sequence
- Trimethoprim - sulfamethoxazol
2) Inhibition of enzymatic inactivation
- Amoxycillin - clavulanat
3) Enhancement - Aminoglycosides
- Penicillins - Aminoglycosides
Antagonism (2) :
1. Inhibition of cidal activity by static agent
- Tetracyclines – Betalactam AB
2. Induction of enzymatic inactivation
- Ampicillin - Piperacillin
CLINICAL INDICATION OF AB
COMBINATION :
► Mixed infection
► Synergism effect
► Risk of developing resistant organism <
► Increase AB coverage or
► Infection of unknown origin
DISADVANTAGES OF AB COMBINATION
- Increase risk of toxicity
- Increase MDR-pathogens
- Increase cost
- Increase antagonism (bacteriostatic
+ bactericide)