GALL BLADDER POLYPS
advertisement

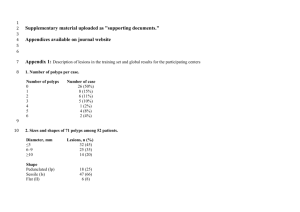
GALL BLADDER POLYPS Dr.Thomas Joseph GB polyp is the term used to describe any mucosal projection into the lumen of Gall bladder Frequency ranges from 1 to 4% Neoplastic or non-neoplastic Non neoplastic lesions account for about 95% of the polyps Pathology Cholesterol polyps Adenomyoma Inflammatory polyps Adenomas Miscellaneous polyps Cholesterol polyps Most common type of GB polyps Variant of cholesterolosis Typically small (<10mm) Pedunculated Usually multiple Adenomyoma Adenomyomatosis of the gall bladder localized to the fundus Hemispheric bulge into the lumen Usually single Adenomas Neoplastic polyps Usually single Can be located anywhere in GB Multiple in one third Sometimes innumerable tiny mucosal polyps-multicentric papillomatosis Co-exists with stones in half the cases Two histologic forms-papillary and non papillary In papillary form there are branching tree like skeleton of connective tissue covered with tall columnar cells In non papillary form there is a proliferation of glands encased by fibrous stroma Adenomas have premalignant potential Frequency of progression from adenoma to carcinoma is much lower than that for colonic polyps Virtually all adenomas with focus of carcinoma are more than 12 mm in diameter Inflammatory polyps Solitary in half the cases Small sessile lesions consisting of granulation and fibrous tissue infiltrated with lymphocytes and plasma cells Miscellaneous Polyps Fibromas Leiomyoma Lipoma Neurofibroma Carcinoids Heterotropic gastric glands Peutz Jegher’s syndrome Usually single Clinical features Usually asymptomatic May detach and behave like a stone Biliary colic Bile duct obstruction Pancreatitis Rarely cause acalculous cholecystitis or hemobilia Diagnosis Usually an incidental finding on USG Lesion inside the gall bladder without acoustic shadow Will not change much with position Size of more than 10mm predicts the risk of malignancy EUS improves diagnostic accuracy 97% accurate in predicting benign nature Tiny echogenic spots or aggregates of echogenic spots suggest Cholesterolosis Multiple microcysts or comet tail artefact suggest Adenomyomatosis 18 flurodeoxyglucose PET scan – uptake predicted the presence of malignancy Colour Doppler Presence of colour signal Diffuse and arborizing pattern Blood flow velocity Resistive index CT/CT biliary cystoscopy Treatment Patients with biliary colic and USG showing both stones and polyps should undergo cholecystectomy If USG shows only polyps – decision depends on severity of symptoms and size of polyps Asymptomatic polyps less than 10mm can be followed up by USG Lesions between 10mm and 18mm should undergo laproscopic cholecystectomy if the patient is an acceptable surgical candidate If poor surgical risk follow up by USG or cholecystography every 6 to 12 months Lesions more than 18 mm should be operated Preferably open cholecystectomy Thank You