TETANUS
Manvi gupta
rabiezahran@hotmail.com
1
Introduction.
Definition
Tetanus is an acute , often fatal disease caused
by an exotoxin produced by the bacterium
Clostridium tetani. But prevented by
immunization with tetanus toxoid.
It is characterized by generalized rigidity and
convulsive spasms of skeletal muscles . The
muscle stiffness usually involves the jaw
(lockjaw)and neck and then becomes
generalized.
rabiezahran@hotmail.com
2
Introduction (con ).
History:
• Tetanus was first described in Egypt over
3000 years ago(Edwin smith papyrus).
• It was again described by Hippocrates
•Carle and Rattone in 1884 who first noticed
tetanus in animals by injecting them with
pus from a fatal human tetanus case.
•During the same year , Nicolaier produced
tetanus in animals by injecting them with
samples of soil.
rabiezahran@hotmail.com
3
Introduction(con).
History:
•In 1889,Kitasato isolated the organism from a
human victim,showed that it produced disease
when injected into animals,and reported that the
toxin could be neutralized by specific antibodies.
•Nocard demonstrated the protective effect of
passively transferred antitoxin,and passive
immunization in humans
•Passive immunization and prophylaxis for tetanus
during World War I
•Tetanus Toxoid was first widely used during
world war II
rabiezahran@hotmail.com
4
Causative Organism
Clostridium tetani
Acridine orange stain of characteristic C tetani with
endospores wider than the characteristic drumstick shape.
rabiezahran@hotmail.com
5
Clostridium tetani
• C.tetani is :
* a slender gram-positive, anaerobic rod that may
develop a terminal spore giving it a drumstick
appearance.
* It is sensitive to heat and cannot survive in the
presence of oxygen.
• It produces two exotoxins :
1) tetanolysin . its function of is not known
with certainty.
2) tetanospasmin is a neurotoxin and causes
the clinical manifestations of tetanus.
Tetanospasmin estimated Human lethal dose is 2.5
ng/kg ((a nanogram is one billionth of a gram)
rabiezahran@hotmail.com
6
Courtesy : Google Image on tetanus
rabiezahran@hotmail.com
7
Spores:
*very resistant to heat and the usual antiseptics.
•They can not survive autoclaving at (121 °C)for 20
minutes.
• relatively resistant to phenol & other chemical
agents.
• widely distributed in soil and in the intestines
and faces of horses, sheep, cattle , dogs , cats , rats,
guinea pigs , and chickens.
Manure-treated soil may contain large numbers of
spores. Spores may persist for months to years.
rabiezahran@hotmail.com
8
rabiezahran@hotmail.com
9
Epidemiology:
a:Occurrence.
b:Reservoir .
c:Mode of Transmission
d:Communicability
rabiezahran@hotmail.com
Source : CDC.,google pictures
10
Epidemiology:
• Tetanus - Greek Word -- Tetanos -to Contract
• Tetanus Remains a Major Public Health
Problem in the Developing World and Is
Still Encountered in the Developed World.
• There Are about 800 000 : 1 Million Deaths
Due to Tetanus Each Year.80% of These
Deaths Occur in Africa and South East Asia
and It Remains Endemic in 90 Countries
World Wide.
•
1998 - U.K,USA 7 Cases, 41 Cases Including One
Neonate
rabiezahran@hotmail.com
11
Epidemiology(con):
•Occurrence: Tetanus occurs worldwide but is most
frequently encountered in densely populated regions in hot ,
damp climates with soil rich in organic matter.
•Reservoir : Organisms are found primarily in the soil and
intestinal tracts of animals and humans.
•Mode of Transmission: is primarily by:
* contaminated wounds,
*Tissue injury( surgery , burns , deep puncture
wounds , crush wounds , Otitis media ,dental infection ,
animal bites, abortion , and pregnancy).
rabiezahran@hotmail.com
12
Epidemiology (contu ):
•Communicability
Tetanus is not contagious from person
to person .It is the only vaccinepreventable disease that is :
“infectious but not contagious”.
Temporal pattern : Peak in winter and
summer season.
Incubation Period: 8 DAYS ( 3-21 DAYS)
rabiezahran@hotmail.com
Source : CDC.,google pictures
13
Host Factors :
• Age : I t is the disease of active age (5-40 years),
New born baby, female during delivery or abortion
• Sex : males > females
• Occupation : Agricultural workers are at higher
risk
• Rural > Urban areas .
• Immunity : Herd immunity(community immunity)
does not protect the individual.
• Environmental and social factors: Unhygienic
custom habits , Unhygienic delivery practices.
rabiezahran@hotmail.com
14
Pathogenesis .
rabiezahran@hotmail.com
15
Pathogenesis
*C. tetani usually enters the body through a wound.
*In the presence of anaerobic conditions, the spores germinate and
start to produce toxin and disseminated via blood and lymphatics.
*Toxin reaches the CNS . by passing along the motor nerves to the
anterior horn cells of the spinal cord .
(The shortest peripheral nerves are the first to deliver the toxin to the CNS, which leads to
the early symptoms of facial distortion and back and neck stiffness.)
*Toxins act at several sites within the central nervous system,
including :
1) peripheral motor end plates,
2) spinal cord,
3) brain,
4) sympathetic nervous system.
rabiezahran@hotmail.com
16
How tetanospasmin
reaches the CNS .
• Tetanospasmin is
taken up by motor
neurons in the
peripheral nerve
endings through
endocytosis. It then
travels along the axons
until it reaches the
motor neuron cell
bodies in the spinal
cord, by fast
rabiezahran@hotmail.com
retrograde transport.
17
Speed of toxin transport:
The toxin travels via intra
axonal transport at a rate of
75 -250 mm/day .
A process which takes 2 -14
days to reach the CNS.
rabiezahran@hotmail.com
18
Pathogenesis (con )
The typical clinical manifestations of
tetanus are caused when tetanus toxin
interferes with release of neurotransmitters blocking inhibitory impulses.
This leads to unopposed muscle contraction and spasm. Seizures may occur,
and the autonomic nervous system may
also be affected.
rabiezahran@hotmail.com
19
Mechanism of Action of
Tetanus Toxin
rabiezahran@hotmail.com
20
Clinical Features
rabiezahran@hotmail.com
21
Incubation period :
I P. ranges from 3 to 21 days, usually about 8
days. In general :
*The further the injury site is from the CNS, the
longer the I P.
*The shorter the I P, the higher the chance of
death.
* In neonatal tetanus, symptoms usually
appear from 4 to 14 days after birth, averaging
about 7 days.
rabiezahran@hotmail.com
22
Types of tetanus:
(On the basis of clinical findings, three different forms of
tetanus have been described).
1) Local tetanus is an uncommon form of
the disease,in which patients have
persistent contraction of muscles in the
same anatomic area of the injury.
Local tetanus may precede the onset of
generalized tetanus but is generally milder
.Only about 1%of cases are fatal.
rabiezahran@hotmail.com
Source : CDC.
23
Types of tetanus(con)
2)Cephalic tetanus is a rare
form of the disease,
occasionally occurring with
otitis media(ear infections)in
which C. tetani is present in
the flora of the middle ear , or
following injuries to the head .
There is involvement of the
cranial nerves, especially in
the facial area.
rabiezahran@hotmail.com
24
Types of tetanus(contu)
3) generalized tetanus
It is The most common type
(about 80%)of reported tetanus
.The disease usually presents
with a descending pattern.
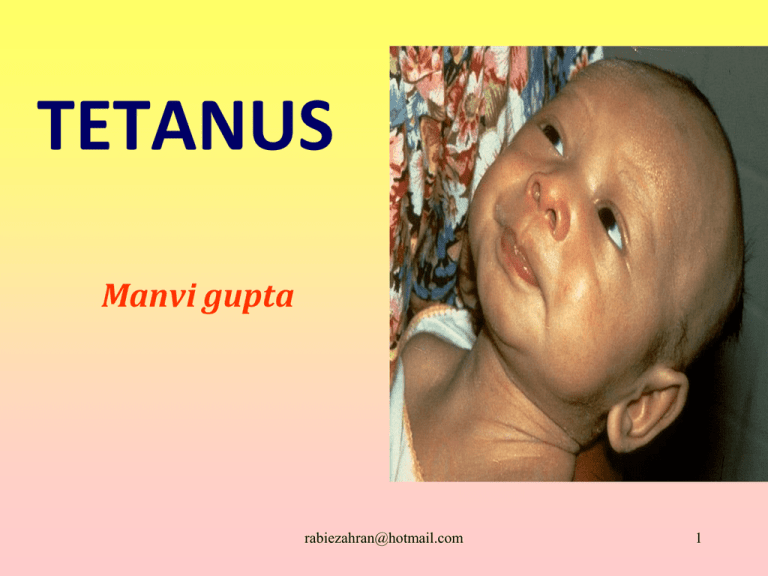
Neonatal tetanus is a form of
generalized tetanus
rabiezahran@hotmail.com
25
Sequence of events
Lock Jaw
Stiff Neck
Difficulty Swallowing
Muscle Rigidity
Spasms
rabiezahran@hotmail.com
26
rabiezahran@hotmail.com
27
Risus Sardonicus in Tetanus Patient
A person suffering from tetanus undergoes convulsive muscle
rabiezahran@hotmail.com
28
contractions of the jaw--called
LOCKJAW
Opisthotonos in Tetanus Patient
The contractions by the muscles of the back and extremities may become so violent
rabiezahran@hotmail.com
29
and strong that bone fractures may occur
Opisthotonos in Tetanus Patient
rabiezahran@hotmail.com
30
Oposotinus postion in tetanus
rabiezahran@hotmail.com
31
Neck rigidity & retraction.
rabiezahran@hotmail.com
32
Unfortunately, the
affected individual is
conscious throughout
the illness,
but cannot stop these
contractions
rabiezahran@hotmail.com
33
Rusty nail may cause prick &
transmit tetanus
rabiezahran@hotmail.com
34
Traumatic T.
Puerperal T.
Type of
Otogenic T.
Tetanus
Idiopathic T.
T. Neonatorum
rabiezahran@hotmail.com
35
Complications .
rabiezahran@hotmail.com
36
rabiezahran@hotmail.com
37
Diagnosis
rabiezahran@hotmail.com
38
Laboratory diagnosis
*There are no laboratory findings characteristic
of tetanus.
*The diagnosis is entirely clinical and does not
depend upon bacteriologic confirmation.
•C. tetani is recovered from the wound in only 30%
of cases and can be isolated from patients who do
not have tetanus.
•Laboratory identification of the organism depends
most importantly on the demonstration of toxin
production in mice.
rabiezahran@hotmail.com
39
Clinically it is confirmed by noticing the
following features:
1. Risus sardonicus or fixed sneer.
2. Lock jaw.
3. Opisthotonos (extension of lower
extremities, flexion of upper extremities
and arching of the back. The examiners
hand can be passed under the back of the
patient when he lies on the bed in supine
position.)
4. Neck rigidity
rabiezahran@hotmail.com
40
Diagnostic tests for tetanus:
Spatula Test :
Apet and Kamad discribe a simple bedside test to diagnose tetanus :
the posterior pharyngeal wall is touched with a
spatula and a reflex spasm of the masseters
indicates a +ve.test.
This test shows 94 % sensitivity . and 100 %
specificity.
The altered whistle :
This explained as an early effect of tone in facial
muscles which causes
the
classic
R
.
sardonicus
rabiezahran@hotmail.com
41
scale for the severity and the prognosis of tetanus:
Score :
One point for each of the following 7 items:
•I P. < 7 days
(period between injury and 1st.symptom.)
•Period of onset < 48 hours
(period between 1st. Symptom and 1st. Spasm. )
•Acquired from burns, surgical wounds, compound
fractures, or septic abortion .
•Addiction (Narcotics)
•Generalized tetanus
•Temperature greater than 104°F (40°C)
•Tachycardia greater than 120 beats per minute (>150
rabiezahran@hotmail.com
42
beats per min in neonates)
Total score indicates the severity
and the prognosis as follows:
Score
Severity
Prognosis
(mortality rate)
0 -1
mild
< 10 %
2 -3
moderate
10 : 20 %
4
severe
20 : 40 %
5:6
very severe
> 50 %
rabiezahran@hotmail.com
43
1) Medical Management .
2) Wound Management .
rabiezahran@hotmail.com
44
Medical Management
Aim of TTT:
(1) provide supportive care (until the tetanospasmin that is fixed in tissue has been
metabolized ) by:
• a: treatment of muscle spasm,
• b: prevention of respiratory complications.
• c: prevention of metabolic complications.
(2)neutralization of circulating toxin to prevent
the continued spread.
(3) elimination of the
source
of
toxin.
rabiezahran@hotmail.com
45
How to treat :
1: Admit patients with severe:
to the (ICU). For risk of reflex spasms .
2: maintain a dark and quiet room for the
patient.
3: Avoid unnecessary procedures .
4: Seriously consider prophylactic intubation
with succinylcholine in all patients with moderateto-severe clinical manifestations. Intubation and
ventilation are required in 67% of patients.
rabiezahran@hotmail.com
46
How to treat :
5:Perform tracheostomy in patients requiring
intubation for more than 10 days. Tracheostomy has
also been recommended after onset of the first
generalized seizure.
7:Tetanus immune globulin (TIG)(passive
immunization) is recommended for treatment
of tetanus. TIG can only help remove unbound tetanus
toxin, but it cannot affect toxin bound to nerve
endings. A single IM. dose of 3000-5000 units is
generally recommended for children and adults, with
part of the dose infiltrated around the wound if it can
be identified.
rabiezahran@hotmail.com
47
How to treat :
Recovered individuals :
do not necessarily develop “natural
Immunity” against the infection--because of extreme potency of the toxin
and very small amount produced during
the infection, It does not elicit a strong ,
protective immune response which would
produce enough antibodies against future
re-infection.
rabiezahran@hotmail.com
48
How to treat :
SO
Active immunization
with tetanus toxoid should
begin or continue as soon as the
person’s condition has stabilized.
rabiezahran@hotmail.com
49
Drugs:
1) Penicillin G:
Adult
10-24 million U/d. ( IV/IM/6h. )
Pediatric
100,000-250,000 U/kg/d. (IV/IM/6h. )
( 10- to 14-d course of treatment is recommended.)
rabiezahran@hotmail.com
50
Drugs:
2) Metronidazole :
*considered as a drug of choice by many.
* has a better safety profile, better tissue penetrability and
negligible CNS excitability.
(penicillin can cause seizures at high doses).
It can also be given rectally
Adult
500 mg orally/6h or 1 g IV /12h;
not to exceed 4 g/d
Pediatric
15-30 mg/kg/d IV divided /8-12h;
not to exceed 2 g/d
rabiezahran@hotmail.com
( 10- to 14-d course of treatment
is recommended.)
51
Drugs:
3)Doxycycline :
Used when there is contraindication to penicillin
or metronidazol.
Adult
100 mg orally/IV /12h
Pediatric
<8 years: Not recommended
<45 kg : 4.4 mg/kg/d) PO/IV divided bid
> 45 kg: Administer as in adults
rabiezahran@hotmail.com
52
Drugs:
Anticonvulsants:
Sedative-hypnotic agents are the mainstays of
tetanus treatment.
1) Diazepam (Valium):
Depresses all levels of CNS, including limbic and reticular
formation, possibly by increasing activity of GABA(γ-Amino-butyric
acid ), a major inhibitory neurotransmitter.
Adult
Mild spasms: 5-10 mg PO /4-6h
Moderate spasms: 5-10 mg IV(diluted in 8 ml glucose 5% or saline )
Severe spasms: Mix 50-100 mg in 500 mL D5W and infuse at 40 mg/h
Pediatric
Mild spasms: 0.1-0.8 mg/kg/d PO divided tid/qid
Moderate or severe spasms: 0.1-0.3 mg/kg IV q4-8h
rabiezahran@hotmail.com
53
2) Phenobarbital:
used to * prolong effects of diazepam.
* treat severe muscle spasms.
Adult
1 mg/kg IM q4-6h;
not to exceed 400 mg/d
Pediatric
5 mg/kg/d IV/IM divided tid/qid
rabiezahran@hotmail.com
54
Skeletal muscle relaxants
These agents can inhibit both monosynaptic and
polysynaptic reflexes at spinal level, possibly by
hyperpolarization of afferent terminals.
* Baclofen (Lioresal) a physiological GABA
agonist
Adult
<55 years: 1000 mcg IT(intrathecal)
>55 years: 800 mcg IT
Pediatric
<16 years: 500 mcg IT
>16 years: Administer as inrabiezahran@hotmail.com
adults
55
Differential Diagnoses
Other Problems to Be Considered
Mandible dislocations,
Stroke ,
Encephalitis
Subarachnoid Hemorrhage
Hypocalcemia
Dystonic Reactions
Meningitis
Peri-tonsillar Abscess
Rabies
Intraoral disease
Odontogenic infections
Globus hystericus
Hepatic encephalopathy
Hysteria
Strychnine poisoning
rabiezahran@hotmail.com
56
Wound Management .
rabiezahran@hotmail.com
57
All wounds should be
cleaned with H2O2&antiseptic.
Necrotic tissue and
foreign material should be
removed.
Passive immunization.
Active immunization. Or Both.
rabiezahran@hotmail.com
58
PREVENTION
rabiezahran@hotmail.com
59
PREVENTION
How to kill spores :
Spores are extremely stable ,but killed by:
• Immersion in boiling water for 15
minutes.
• Autoclaving for 15-20 minutes at 121°c.
• Sterilization by dry heat for 1 -3 hrs at
160 °C.
• Ethylene oxide sterilization is sporocid.
rabiezahran@hotmail.com
60
PREVENTION
Fumigation
• Sterilization of operation theatre by :
* 500 ml of formalin , 200gms of Potpermanganate/30 cu . meters of space
*All windows and doors are closed except one .
*Fissures between the panels of the doors and
windows are closed with adhesive tape
*After 12 hours the doors and windows are
opened and the theatre is aired for 24 hours
before decommissioning it.
rabiezahran@hotmail.com
61
Active Immunization
by using
tetanus toxoid
rabiezahran@hotmail.com
62
TETANUS TOXOID
• Tetanus toxoid was developed by Descombey in 1924,
• Tetanus toxoid immunizations were used extensively
in the armed services during World War II.
• Tetanus toxoid consists of a formaldehyde-treated
toxin.
• There are two types of toxoid available —
1)adsorbed (aluminum salt precipitated)toxoid
2) fluid toxoid.
• Although the rates of seroconversion are about
equal,the adsorbed toxoid is preferred because the
antitoxin response reaches higher titers and is longer
lasting than that following the fluid toxoid.
rabiezahran@hotmail.com
63
rabiezahran@hotmail.com
64
Passive Immunization
rabiezahran@hotmail.com
65
Passive Immunization
1. ATS(equine)I g.
1500 IU/s.c
after sensitivity test
(or)
2. ATS(human)I g. 250-500 IU,
no anaphylactic shock, very
safe and costly.
rabiezahran@hotmail.com
66
Tetanus Neonatorum.
rabiezahran@hotmail.com
67
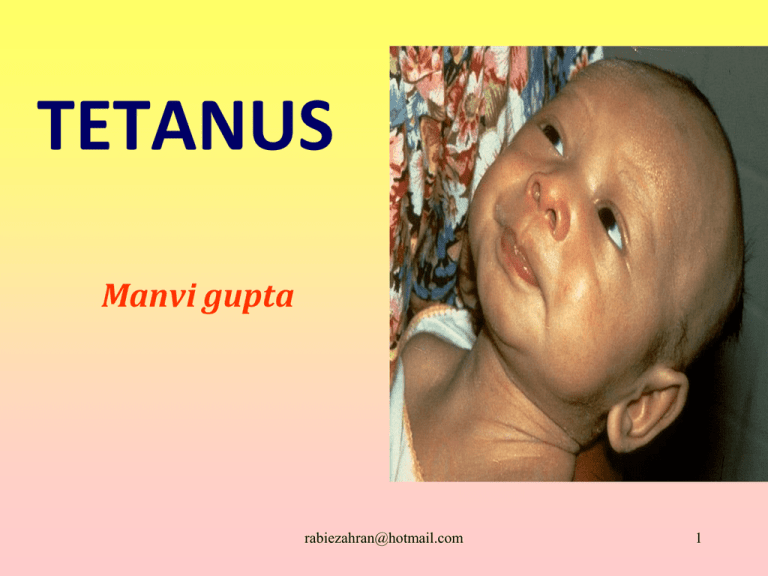
Newborn
showing risus
sardonicus and
generalized
spasticity
rabiezahran@hotmail.com
68
rabiezahran@hotmail.com
69
THANK YOU
rabiezahran@hotmail.com
70