Mindfulness Based Stress Reduction and Failed Back Surgery
advertisement
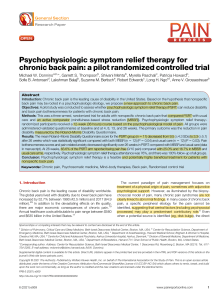
Mindfulness-Based Stress Reduction for Failed Back Surgery Syndrome: A Randomized Clinical Trial SPARC Mind-Body Medicine Greg Esmer DO Staff Physician Osteopathic Advantage 4/16/2011 Disclosures I have no actual or potential conflict of interest in relation to this program/presentation. Learning Objectives Become familiar with the design and implementation of this trial State whether this trial supports the treatment of Failed Back Surgery Syndrome with Mindfulness Based Stress Reduction Mindfulness Based Stress Reduction for Failed Back Surgery Syndrome: A Randomized Clinical Trial Investigators: Greg Esmer DO (co-PI), James Blum Ph.D (co-PI), Joanna Rulf OMS IV, and John Pier MD. A Single-Center, Prospective, Randomized, Single-Blinded, ParallelGroup-Design Clinical Trial Mindfulness Based Stress Reduction for Failed Back Surgery Syndrome: A Randomized Clinical Trial Journal of the American Osteopathic Association 2010;110(11):646-652 Funded by University of New England College of Osteopathic Medicine and the Osteopathic Heritage Fund Mindfulness? QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture. Mindfulness Awareness where thoughts, emotions, and physical sensations are accepted as is Developed within several religious traditions over the past 2500 years Mindfulness-Based Stress Reduction (MBSR) A clinical education treatment approach for chronic illness Mindfulness presented in a secular, healthcare context Developed at UMass Medical Center Over 600 MBSR Instructors worldwide 8 week course Failed Back Surgery Syndrome (FBSS) Back or leg pain that persists or recurs after one or more surgical procedure on the lumbosacral spine Yearly incidence of FBSS is estimated to be between 25,000 and 80,000 Pain from FBSS is often debilitating and recalcitrant to treatment Subject Procurement Subjects with FBSS were recruited from a multidisciplinary spine center in Portland, Maine 220 study invitation letters sent 40 subjects were randomized 19 randomized MBSR 21 randomized to Waitlist Control 15 subjects analyzed in MBSR group 10 subjects analyzed in Waitlist Control 2 Tiered Trial Design 12 week Randomized Clinical Trial MBSR Intervention arm Waitlist/Control arm 40 week Observational No Control group Intervention Reliability Course Instructors completed the UMass Teacher Development Intensive Professional experience in Healthcare, Education, or Social Change Longstanding Meditation and Body Centered (Yoga) Practice Completed a 10 day Silent, teacher led, Meditation Retreat Course Instructors: Sue Young MA & Greg Esmer DO. MBSR and FBSS Outcome Measures Roland-Morris Disability Questionnaire (RMDQ) Chronic Pain Acceptance Questionnaire (CPAQ) Abridged Pittsburgh Sleep Quality Index (PSQI) Analgesic Medication Log Summary Visual Analog Scale (VAS) for Pain MBSR and FBSS Baseline Characteristics No statistically significant differences in age, gender, height, weight, health status No history of workers compensation Relatively low RMDQ (~7) ie. high function for the FBSS population MBSR and FBSS 15/19 (79%) completed the MBSR course 10/21 (48%) completed the Waitlist Control Roland Morris Disability Questionnaire Control MBSR P value MBSR 12 week 12 week 12 week 40 week n=10 n=15 Control n=15 v MBSR -0.1 -3.6 <0.005 -3.4 (1.9) (3.4) (3.5) Standard deviation in parentheses 0=high function, 24=low function Range 0-24 scale RMDQ / function 0 -0.5 -1 -1.5 -2 Control -2.5 MBSR -3 -3.5 -4 12 Weeks 40 Weeks Differences from Baseline at 12 and 40 weeks 0-24 point scale 12 week p<0.005 clinically and statistically significant 0=high function 24=low function Chronic Pain Acceptance Questionnaire Control MBSR P value MBSR 12 week 12 week 12 week 40 week n=10 n=15 Control n=15 v MBSR -6.7 7.0 <0.014 9.0 (11.0) (13.5) (8.4) Range 0-108 scale Standard deviation in parentheses 0=low pain acceptance, 108=high pain acceptance CPAQ / quality of life 10 8 6 4 2 0 -2 -4 -6 -8 Waitlist Control MBSR 12 week 40 week Differences from Baseline at 12 and 40 weeks 0-108 point scale 12 week p<0.014 clinically and statistically significant 0=low pain acceptance 18=high pain Mr Chambers enters a period of self-acceptance Abridged Pittsburgh Sleep Quality Index Control MBSR p value MBSR 12 week 12 week 12 week 40 week n=10 n=15 Control n=15 v MBSR -0.2 2.0 <0.047 1.9 (1.7) (3.5) (3.3) Range 0-5 scale Standard deviation in parentheses 0=low sleep quality, 5=high sleep quality Abridged PSQI / Sleep 2 1.5 1 Waitlist Control 0.5 MBSR 0 -0.5 12 week 40 week Differences from Baseline at 12 and 40 weeks 0-5 point scale 12 week p<0.047 clinically and statistically significant 0=poor sleep quality 4=good sleep Analgesic Medication Log Control MBSR P value MBSR 12 week 12 week 12 week 40 week n=10 n=15 Control v MBSR 0.4 (1.1) -1.5 (1.8) <0.001 No results Range 0-4 scale Standard deviations in parentheses 0=no analgesics, 2=daily non-narcotic analgesics, 4=daily narcotic analgesics Analgesic Medication Log 0.5 0 -0.5 Watilist Control MBSR -1 -1.5 0=no analgesics, 2= daily non-narcotic analgesics, 4= daily narcotics Differences from Baseline at 12 weeks 0-4 point scale 12 week p<0.001 clinically and statistically significant Summary Visual Analog Scale for Pain Control MBSR P value MBSR 12 week 12 week 12 week 40 week n=10 n=15 Control n=15 v MBSR -0.2 -6.9 <0.021 -6.1 (6.0) (6.9) (8.3) Range 0-30 scale Standard deviation in parentheses 0=no pain, 30=worst pain imaginable Summary VAS for Pain 0 -1 -2 -3 Waitlist Control -4 MBSR -5 -6 -7 12 week 40 week Differences from Baseline at 12 and 40 weeks 0-30 point scale 12 week p<0.021 clinically and statistically significant 0=no pain, 30= worst pain imaginable Outcome Measures Statistical and Clinical Significance achieved at 12 weeks for RMDQ, CPAQ, Abridged PSQI, Analgesic Log, and Summary VAS for Pain Gains were maintained at 40 weeks for the uncontrolled portion of the study MBSR in PDX Courses are taught Dr. Esmer at Osteopathic Advantage in Johns Landing Next course begins on April 27 Wednesday nights, 6:30pm-8:00pm 8 week course Call 503.230.2501 for course details gregesmer@yahoo.com Bibliography Kabat-Zinn J, et al: Four–Year Follow-Up of a Meditation –Based Program for the Self_Regulation of Chronic Pain: Treatment Outcomes and Compliance. The Clinical Journal of Pain 1987, 2:159-173 Kabat-Zinn J, et al: The Clinical Use of Mindfulness Meditation for the Self-Regulation of Chronic Pain. Journal of Behavioral Medicine 1985,8:163-190 Bibliography Randolph P, et al: The Long-Term Combined Effects of Medical Treatment and a Mindfulness-Based Behavioral Program for the Multidisciplinary Management of Chronic Pain in West Texas. Pain Digest 1999, 9:103-112 Plews, Ogan M, et al: Brief Report: A Pilot Study Evaluating Mindfulness-Based Stress Reduction and Massage for the Management of Chronic Pain. J Gen Intern Med 2005,20:136138 Bibliography Ragab A, Deshazo RD. Management of back pain in patients with previous back surgery. The American Journal of Medicine 2008;123:272-278. Roland M, Fairbank J: The RolandMorris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine 2000, 25:3115-3124 Bibliography Kelly A: The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain. Emerg Med J 2001,18: 205-207 Buysse D, Reynolds C, Monk T, Berman S, Kupfer D: The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Research, 28: 193-213 Jenson M, et al: Relationship of Pain Beliefs to Chronic Pain Adjustment. Pain 1994, 57:301309