Mammography
Introduction and History
• Breast cancer is 2nd only to lung cancer as
cause of death in women
– Very treatable with early detection!
• 1st innovation since radical mastectomy
introduction in 1898
– In 1913, radiographic appearance of breast
cancers was first reported
• Mammography became a reliable diagnostic tool
in 1950s when industrial grade x-ray film
introduced
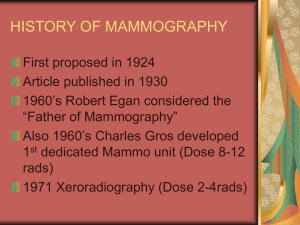
History Of Mammography
(cont’d)
• 1960’s – Xerography introduced – much lower
dose
• Research conducted in 1970s clearly showed
mammography to be essential part of early diagnosis
• 1975 – High speed/resolution film introduced by
DuPont
• 1992 – MQSA implemented (Mammography Quality Standards Act)
Definition of breast cancer:
• Cancer that forms in tissues of breast,
usually ducts (tubes that carry milk to
nipple) and lobules (glands that make
milk).
• Occurs in both men and women (male breast
cancer is rare)
MQSA
• Mammography was 1st and only federally
regulated imaging exam with implementation of
Mammography Quality Standards Act (MQSA)
• Mandated following:
–
–
–
–
Formal training and continuing education
Required regular inspection of equipment
Documentation of quality assurance
Reporting results, follow-up, tracking pts, and
monitoring outcomes
Principles Of Breast Cancer
• Pt.s in early stages respond well to treatment
• Patients with advanced disease do poorly
• Earlier diagnosis, better chance of survival
• Mammography is tool for early detection
Risk v. Benefit
• Breast cancer in United States in 2009 (estimated):
New cases: 192,370 (female); 1,910 (male)
Deaths: 40,170 (female); 440 (male)
•
Us population 306 million in 2007- 133 deaths /million
• Mortality risk from mammography induced radiation is 5 deaths/
million pts. using screen film mammography
• More risky to refuse mammography!
Breast Cancer Screening
• Very 1st Mammogram is Baseline (or first mammo. after
surgery)
• There after: screening mammogram pt.
must be asymptomatic – no known breast
problems
• American Cancer Society and American
College of Radiology recommend
screening annually for women over age 40
Diagnostic Mammogram
• For woman presenting with clinical
evidence of breast disease, palpable mass
or other symptom
• Uses specific projections to
– Rule out cancer
– Demonstrate suspicious area seen on
screening mammogram
Breast Cancer Risk Factors
• Risk increases with age
• Hormonal history
– Risk increases with early menses, late
menopause, pregnancy after age 30, or
nulliparity
• Family history
– Risk increases -daughter, mother, or sister
has breast cancer
Breast Anatomy
• Breast same as mammary gland
• Lobulated, glandular structures located in
superficial fascia of anterolateral wall of
thorax
• Secondary sex characteristic
• Base of breast
overlies pectoralis
major and serratus
anterior muscles
• Part of breast
extends into
axillary fossa
Anatomy (cont’d)
• Breasts vary in
size and shape!
• Consist of
glandular, fat,
and muscle
tissue
Breast Anatomy
• Lobule size affected by age and hormones
• Involution: process of decreasing lobule
size with age and after pregnancy
Anatomy
• The breast tapers anteriorly ending in the nipple
• Encircled by areola: area of pigmented skin
• Breasts are supported by Cooper’s ligament
which determines firmness or lack thereof
• Female breasts are divided into 15 – 20 lobules
Breast Anatomy
• Each lobe divided into many
lobules
• Lobules are basic structural
unit of breast
• Lobules contain
– Several acini
– Draining ducts
– Interlobule stroma (connective
tissue)
Breast Anatomy
• Lymphatic vessels of breast drain into two
sets of nodes
– Axillary lymph nodes, laterally
– Internal mammary lymph nodes, medially
• Axillary nodes are often evaluated on
mammograms
Tissue Variations
• Breasts -glandular and connective
• Ability to visualize depends upon amount
of fat within and around breast lobulesprovides contrast
• Postpuberty breasts contain primarily
dense connective tissue
During pregnancy, breasts undergo
hypertrophy
• Fatty tissue replaces glandular tissue after lactation and
advancing age
• After menopause, glandular tissue begins to atrophy
Typical Mammography Unit
Equipment is
C-arm
SID is fixed
at 24 – 26”
Mammography Equipment
• Dedicated units have high-frequency
generators
• Provide more precise control of kVp, mA,
and exposure time
• Specially designed to produce highcontrast and high-resolution images
Mammography uses
• Low kVp : 25 – 28
• AEC
• Anode material made of molybdenum, with
rhodium target
• Grid with ratio: 4:1, or 5:1 200 lines/inch
Magnification
•
•
•
•
Increases visibility of small structures
Increase OID
Uses air gap
Radiation dose increases with
magnification
Compression Device
• Compression
decreases
thickness of
breast,
magnification
and scatter
• Increases
contrast
• Reduces motion
unsharpness
• Reduces dosage
Compression Device
Made of firm plastic
Amount of compression:
between 25 and 40 pounds
pressure
Compression may be
uncomfortable!
Screen-Film Systems
• Mammography cassettes contain a single
screen
• Film is single emulsion
• Occasionally, extended time processing is
used
– (reduces dose and increases contrast)
Digital Mammography
State of the art!
• No film or chemical processing
• Images easily sent over internet
• Much better definition
Possible downside-if 1st digital compared to
previous film mammo., can give false
positives due to increased sensitivity!
- Slightly higher dosage
Procedure
• Complete, careful history and physical
assessment
– Take notes on location of scars, palpable
masses, skin abnormalities, and nipple
alterations
• Examine previous mammograms for
positioning, compression, and exposure
factors
Procedure (con’t)
• Patients dress in open-front gown
• Breasts must be bared for imaging
– Cloth will cause image artifact
• Remove deodorant and powder from axilla
and breast
– Can mimic calcifications on image
Procedure (cont’d)
• Explain procedure to pt., including
possibility for additional projections
• Consider natural mobility of breast before
positioning
• Support breast firmly so that nipple is
directed forward
• Profile nipple, if possible
Positioning
Procedure
• Apply proper compression to produce
uniform breast thickness
– Essential to high-quality mammograms
• Place ID markers according to standard
convention
Routine mammography projections
Craniocaudal (CC)
Mediolateral oblique
(MLO)
Craniocaudal Projection
Patient position
– Standing or seated facing IR holder
• Part position
– Elevate inframammary fold to maximum
height
– Adjust IR height to inferior surface of breast
– Gently pull breast onto IR holder with both
hands while instructing patient to press chest
to IR holder
Craniocaudal Projection
• Arrange breast on film so
nipple is in profile and
maximum amount of breast
tissue is radiographed
• CR – Perpendicular to base of
breast
• Structures – Central,
subareolar, medial
fibroglandular breast tissue,
pectoral muscle
Craniocaudal Positioning
(cont’d
– Immobilize breast with one hand
– Use other hand to move opposite breast out
of image
– Shoulder relaxed in external rotation
Craniocaudal Projection (cont’d)
– Rotate head away from breast being
examined (watch out for hair!)
– Lean pt. toward machine
– Place hand on shoulder and slide skin over
clavicle
– Compress breast slowly until skin taut
CC Projection
Mediolateral Oblique Projection
• Position
– Center breast with nipple in profile, if possible
– Hold breast up and out
– Compress breast slowly until taut
– Pull down on abdominal tissue to open
inframammary fold
Mediolateral Oblique positioning
– Instruct pt. to hold opposite breast laterally,
out of anatomy of interest
– Exposure on suspended respiration
– Release compression immediately!
Mediolateral Oblique
• Open inframammary fold
• Deep and superficial breast tissues well
separated
• Retroglandular fat well seen
• Uniform tissue exposure
– If compression is adequate
Mediolateral Oblique
• Degree of obliquity is 30° to
60°
• Depends on body habitus
– Tall, thin patients require
steeper angulation
• CR perpendicular to base of
breast
• Structures – lateral aspect of
breast and axillary tail
Mammographer’s Nightmare
Radiography Of Augmented Breast
(implants)
• 8 projections must be obtained (2x4)
• MRI and sonography can help determine
rupture or leakage
• Four standard images with implant
displaced posteriorly into chest wall are
obtained
Breast Implants
Saline vs Silicone
• Some surgeons feel silicone implants have a more natural look and
feel because silicone gel texture similar to breast tissue.
• Silicone implant ruptures are harder to detect. When saline implants
rupture, they deflate -results are seen almost immediately. When
silicone implants rupture, breast often looks and feels same because
silicone gel may leak into surrounding areas of breast without a
visible difference.
• Replacing a ruptured silicone gel implant is more difficult than
repairing saline implant. Silicone implants have higher rate of
capsular contracture (scarring and hardening around implant).
• Saline implants inflated to desired size with saline, then valve is
sealed by surgeon
Implants can be in front of pectoral muscle or
behind
Radiography Of Augmented Breast
(implants)
Complications:
• Increased fibrous tissue surrounding
implant (contracture)
• Shrinking
• Hardening
• Leakage
• Pain
Male Mammography
• Approximately 1000 males develop
breast cancer every year
• Standard CC and MLO are obtained
• Males not screened- mammogram only if
lump discovered
Gynecomastia
Imagine Living without Man boobs!
If someone would've said to
picture my life without
man boobs, I
couldn't. Sad but true.
How do you picture a life
without something you'd
had your entire life? I'd
learned to live with
them... the hiding... the
put-downs...
$100,000 one year
Treatment For Breast Cancer
•
•
•
•
Lumpectomy
Partial or radical mastectomy
Radiation
Chemotherapy
CC view
( lesion)
Needle Localizations
• Used to localize breast lesions before
surgery
• Special, open-hole plate may be used for
ease of localization
– Plate contains grid to plot coordinates
– Operative stereotactic surgery may be used
• Two offset images are obtained to create a 3dimensional image
Needle
Localization
Breast Specimen Radiography
• Performed after surgery once lump has
been excised
• Determines extent of calcifications within
specimen
• Magnification technique may be used
Breast Specimen Radiograph
24 yr. old (has children)
19 yr. old (never pregnant)
Calcified Milk Ducts
Various
abnormal
mammograms
The End