IUD Development: Types, History & Modern Advancements
advertisement

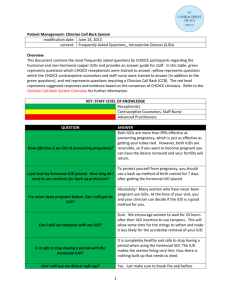
DEVELOPMENT IN INTRAUTERINE DEVICES ( IUD ) Presented BY : AHMAD NOOR, PHARM.D AHMED ALTAYAR, PHARM.D Lecture outlines : What is the IUD ?how does it work ? The types of IUD’s Advantages & disadvantages History & development of IUD’s The most IUD’s used today Insertion of the IUD’s Introduction At the beginning as you know it is a happiness for every parent’s to have a baby , but in the same time it is very important to put in mind all other factors that may effect the family life either : health , economical or even social problems ,which increase in cases of a large and uncontrolled number of family members , from this point of view the need for a way to control the number of birth was established , to improve the population life-style Our responsibility as pharmacists appear in development and searching for different techniques to control pregnancy ,and we will talk today about one of this ways and its development What is an ( IUD ) ? It is a small, flexible, plastic device that contains either metal e.g. copper or hormones e.g. progesterone and is inserted into the uterus to prevent pregnancy. How dose it work ? It may : -Block sperm from reaching or fertilizing the egg -Make the lining of the uterus unsuitable for implantation . -interfere with the ovulation process We do not know which of these actions is most important for preventing pregnancy and most likely all of them work together. Types of ( IUD ) : There are two main categories of IUD’s: 1. Medicated: These forms of IUD use hormones or metals to prevent conception. progesterone and Copper plated IUDs are considered medicated because they have abilities to hinder fertilization. 2. Non Medicated: This category includes all other forms of IUD no matter shape or size. Advantages and the Disadvantages of ( IUD ) Advantages: - Once inserted , remain in place . - Remains effective while in place. - it prevents pregnancy for long period - does not interfere with sexual activity. Disadvantages : - May cause bleeding and cramping . - Increased risk of octopic pregnancy. - Doesn't prevent sexual transmitted diseases. - it is not recommended for women who have heavy or long period What is the history of (IUD) ? - Camel riders in the Middle East are the first recorded users of the IUD or Intrauterine Device. It was common knowledge that if you placed small stones in the uterus of your camel, it would not become pregnant even during its periods of high sexual activity . Hippocrates, the original Greek doctor, also wrote : small piece that could be put into the uterus of a woman with the help of a small tube can prevent pregnancy . In 1909 a German physician named Richard Richter began to build IUDs from small bronze rings and silk thread. Richter, as well as many other doctors versions of the IUD was too large for widespread use and caused painful infections. In 1930, Ernest Grafenberg improved Richter's idea making the contraptions smaller, avoiding most infections and making the device more comfortable. By the early 1960’s many other forms/designs of IUD were invented and were constructed of safer materials . - Since 1998 worldwide, several new intrauterine devices (IUDs) are under development or in the early marketing phase. These new devices contain various modifications designed to improve patient continuation and physician satisfaction. Modifications include those designed to facilitate easier insertion and removal, decrease the rates of accidental expulsion, and reduce complaints of pain or bleeding a. Lippes-Loop b. Saf-T-Coil c. Dana-Super Dana cuprum d. Copper-T e. Copper-7 f. Multiload g. Progesterone IUD What are the most cu ( IUD ) used today ? Today two types of cu IUD are used mostly Multiload (left) and cupper T (right) : What is the hormonal (IUD) used today? Late last year the FDA approved the intrauterine device (IUD) Mirena. Mirena is a Tshaped that releases small amounts of the hormone (levonorgestrel) to block conception, Mirena only needs to be replaced once every five years. The others, in contrast, must be changed yearly. A new IUD available in Europe & US uses a synthetic hormone to achieve a high rate of long-acting contraception. WHAT ARE THE NEW DEVELOPMENT IN ( IUD ) ? Developers are designing devices to address the disadvantages issue by modifying IUD size, shape, and flexibility. At least six new devices are under development, or have recently been introduced, outside the US. These devices include: Cu safe 300 Fincoid350 Soft-T Multiload mark 2 Gynefix ICFD CuSafe 300 The CuSafe 300 is a T-shaped copper IUD with flexible, uniquely shaped arms. Both ends of the device's transverse arms curve inward to reduce uterine tissue irritation. In addition, its mono filament tail is welded into the shaft, instead of knotted, to reduce ectocervical abrasion device's flexible design facilitate easier ,less painful insertion and removal, aslo the curved "fundalseeking" arms resist expulsion. carries a recommended life span of 5 years. Advantages in comparison to copper T 380A IUD: the inserter is about one third smaller than that of the copper T 380A IUD. These improvements should make the CuSafe 300 easy to insert and remove. pain and bleeding occurred significantly less frequently among CuSafe IUD users, also the CuSafe had low and statistically significant decrease rates of pregnancy and expulsion Fincoid-350 The Fincoid-350, devised in Finland, is also designed to resist accidental expulsion. The IUD has a plastic skeleton comprised of two parts: curved horizontal arms, and a copper coated vertical stem. The resultant movable joint easily constricts and expands with uterine contractions, adjusting to variations in uterine size and shape. The Fincoid-350 comes in two sizes: standard and short. Sof-T The Sof-T, manufactured and approved for use only in Switzerland, is a copper IUD with a unique shape to enhance effectiveness. The device has soft, flexible knobs, or occlusion bodies, on each end of its flexible transverse arms. These knobs theoretically block the entrances into the fallopian tubes. Two dimensional ultrasound must be used for insertion , however, to ensure exact placement of the device. The device's potential ability to occlude the fallopian tubes could, in theory, reduce the incidence of tubal infection and ectopic pregnancy.On the other hand, the knobs may incompletely block the fallopian tubes and result in higher rates of ectopic pregnancy. About 1,200 women currently wear the device. Limited data indicate that the annual expulsion rate ranges between 0.3% and 3.5%, removals for pain or bleeding range from 0% to 1.4% Multiload Mark II The Multiload Mark II is an updated version of the original Multiload 375 (ML 375). The original device has a record of dependability, with low patient cessation rates due to pregnancy, expulsion or bleeding and pain. The ML 375 has been associated with problematic insertions, however, because its arms do not fit into the inserter; the arms are open during insertion, making placement more difficult. the new inserter's diameter is smaller than the original model. In addition, the inserter has three other improvements: its design prevents the IUD from getting pushed beyond the inserter; it can function as a uterine sound; and it has a one handed expulsion action. These innovations may help limit the risk of uterine perforation. GyneFix® The GyneFix, a "frameless" IUD, consists of six 5 mm copper sleeves. This device was originally called the Cu-Fix 390, then later the FlexiGard 330®. The device has undergone 10 years of testing and several modifications to its inserter and anchoring mechanisms. The upper and lower copper sleeves are crimped onto the suture thread to prevent slippage. The proximal end of the suture contains a knot that is pierced 1 cm into the fundal myometrium to anchor the device into the uterine muscle. Variations of the device for postpartum use include a larger knot and a cone shaped biodegradable tip that help anchor it securely. Due to its frameless design, flexibility, and minimal presence in the uterine cavity, the GyneFix is associated with few expulsions. In addition, the device has a high continuation rate at 1 year (90%) due to few removals for complaints of bleeding or pain. Effectiveness depends upon proper insertion technique because the device must be securely anchored into the uterine myometrium or it will be expelled.In addition, the device has very low expulsion rates among nulliparous women. Intracervical Fixing Device (ICFD) The intracervical fixing device differs substantially in both construction and placement from other IUDs. The device consists of a rod shaped, copper coated polyethylene frame that is about 4 cm long with a 5 mm projection at the distal end. Through this projection, the ICFD is anchored (fixed) to the inner cervical wall using a modified tenaculum. Investigators believe the ICFD's anchoring mechanism could be improved. Better anchoring mechanisms could help to prevent expulsions. One potential advantage of the device is that the insertion procedure is not blind. In addition, because of the intracervical location, the device will likely be associated with less spotting, bleeding and pain. Conclusion Developers are designing new IUDs with modifications to help enhance patient and physician acceptance. Modifications to the devices aim to decrease removals due to pain and bleeding, make insertion and removal easier, and limit the risk of expulsion and prolong the life span of the device . HOW TO INSERT ( IUD )? THANKS FOR YOUR ATTENTION!! Presented by : AHMAD NOOR, PHARM.D AHMED ALTAYAR, PHARM.D