File
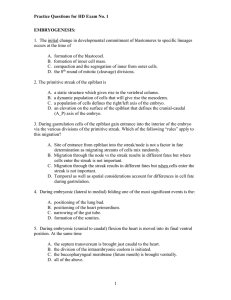
advertisement

Introduction Litigation Indemnity cover: MPS Urologic complications Important to know the normal urinary tract anatomy and various anomalies (3.3-11.1% of the population) encountered in clinical practice To prevent injury and complications and medicolegal problems Causes of oliguria Prerenal Decreased volume Dehydration Blood loss Third space sequestration Circulatory Septic shock Cardiogenic shock Postrenal Acute obstructive uropathy Ureteral obstruction Urethral obstruction Urinary extravasation Intrinsic renal disease Ureteric injury Low incidence (0.4-2.5%) but serious implications of morbidity and litigation 75% occur during gynaecologic surgery Thought to be higher with laparoscopic surgery Only 1/3 detected during surgery Intraop recognition is critical for prompt repair before renal compromise occurs Prevented by routine identification and dissection of the ureter Risk factors for ureteric injury Enlarged uterus Distorted anatomy Previous pelvic surgery Massive bleeding Ovarian neoplasms Endometriosis Pelvic adhesions Types of ureteric injury Ligation Angulation Transection Laceration Crush Ischaemia Resection Sites of ureteric injury Most common site during abdominal hysterectomy or adnexectomy is the pelvic brim where it lies beneath the IFP ligament 2. Over the iliac arteries 3. In the cardinal ligament at the level of the internal cervical os where the uterine artery crosses the ureter 4. At the anterolateral vaginal fornix as the ureter enters the bladder 1. Sites of injury 5. In vaginal hysterectomy: near the internal cervical os and vaginal fornices as it enters the trigone of the bladder 6. At laparoscopy near the USL esp. with endometriosis 7. Trying to control bleeding in broad ligament at caesarean hysterectomy 8. Hypogastric artery ligation Prevention of ureteral injuries Ureteric stenting for difficult cases e.g. Ca ovary Adequate exposure during surgery. Identify the ureter Avoid blind clamping of vessels Caution when using diathermy (laparoscopy) Diagnosing ureteric injury 70% diagnosed postop in gynaecologic procedures Intraoperative diagnosis If ureters can’t be identified, use of IV methylthioninium chloride or indigo carmine can demonstrate patency Intraop transurethral cystoscopy or abdominal telescopy may be used to show ejaculation of dye stained urine from both ureteric orifices Cystoscopy should be considered for complex cases Postoperative diagnosis Symptoms are variable: Flank pain, fever, haematuria, retroperitoneal urinoma (sonar) IVP, CT with IV contrast, retrograde ureterogram, renal u/s, cystoscopy, contrast dye tests Treatment of ureteral injuries: principles Tension free anastomosis Minimal use of fine absorbable suture Use of peritoneum or omentum to surround the anastomosis Drain site with passive drain to prevent urine accumulation Stent with ureteric catheter Case Prolonged labour C section done Post-op abd distension ? Diagnosis Bladder injury 2 layer repair Catheter for 10 days Cardiovascular complications Perioperative cardiac morbidity is the leading cause of death after anaesthesia and surgery Includes: MI, unstable angina, CCF, dysrhythmia Risk factors: Age, previous MI, hypertension, Diabetes Prevention: good preop care, lab tests, ECG, CXR, cardiologist review Haematological complications: risk factors Alcohol abuse Von Willebrand’s disease Liver disease Chronic renal disease Family h/o bleeding SLE tendency Prior need for transfusion Severe menorrhagia Frequent nosebleeds Easy bruising Anticoagulant use Antiplatelet drugs Intraoperative bleeding: risk factors Surgical technique: blood vessels in retroperitoneal space Obesity Large pelvic mass Adhesions Cancer Prior radiotherapy Blood product replacement Red cell transfusion: whole blood, red blood cells, leukocyte-poor red cells, washed red cells Platelet transfusion Plasma derivatives: Cryoprecipitate-rich in Factor VIII and fibrinogen GIT Approached with trepidation by the gynaecologist Important in complicated surgery like Ca ovary Bowel injury during surgery Postop complications: Perforation, ileus, obstruction, reexploration for bowel complications, fistulae Others Retained foreign bodies Lymphoedema Sexual dysfunction Death