Management of MDRO(multidrug resistant organisms) in health care
advertisement
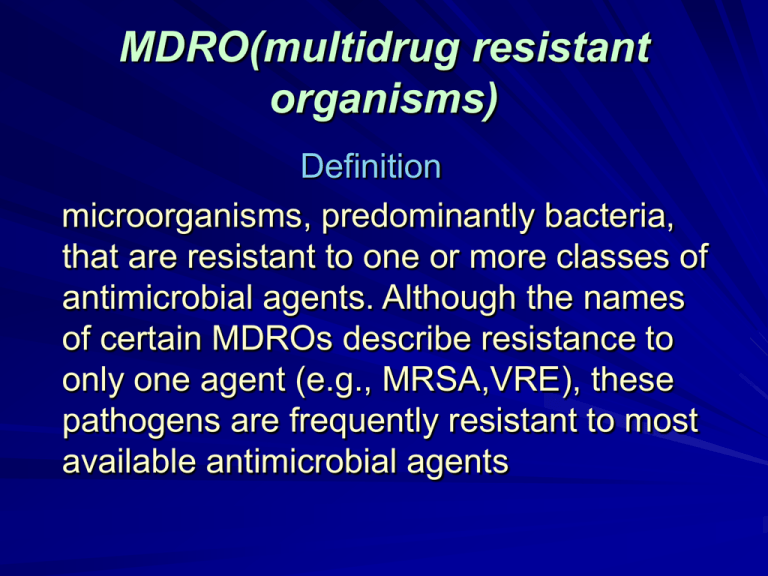
MDRO(multidrug resistant organisms) Definition microorganisms, predominantly bacteria, that are resistant to one or more classes of antimicrobial agents. Although the names of certain MDROs describe resistance to only one agent (e.g., MRSA,VRE), these pathogens are frequently resistant to most available antimicrobial agents MDRO(multidrug resistant organisms In addition to MRSA and VRE, certain gram negative bacteria(GNB), including those producing extended spectrum betalactamases (ESBLs) and others that are resistant to multiple classes of antimicrobial agents, are of particular concern MDRO(multidrug resistant organisms Drug-resistant pathogens are a growing threat to all people, especially in healthcare settings. MDRO(multidrug resistant organisms Each year nearly 2 million patients in the United States get an infection in a hospital. Of those patients, about 90,000 die as a result of their infection. More than 70% of the bacteria that cause hospital-acquired infections are resistant to at least one of the drugs most commonly used to treat them. Persons infected with drug-resistant organisms are more likely to have longer hospital stays and require treatment with second- or third-choice drugs that may be less effective, more toxic, and/or more expensive Clinical importance of MDROs - In most instances, MDRO infections have clinical manifestations that are similar to infections caused by susceptible pathogens. However, options for treating patients with these infections are often extremely limited. Although antimicrobials are now available for treatment of MRSA and VRE infections, resistance to each new agent has already emerged in clinical isolates. - Similarly, therapeutic options are limited for ESBL-producing isolates of gram-negative bacilli Clinical importance of MDROs -These limitations may influence antibiotic usage patterns in ways that suppress normal flora and create a favorable environment for development of colonization when exposed to potential MDR pathogens (i.e., selective advantage). -Increased lengths of stay, costs, and mortality also have been associated with MDROs. Clinical importance of MDROs The type and level of care influence the prevalence of MDROs. ICUs, especially those at tertiary care facilities, may have a higher prevalence of MDRO infections than do non-ICU settings Methicillin Resistant Staph (MRSA) MRSA was first isolated in the United States in 1968. By the early 1990s, MRSA accounted for 20%25% of Staphylococcus aureus isolates from hospitalized patients. In 1999, MRSA accounted for >50% of S. aureus isolates from patients in ICUs in the National Nosocomial Infection Surveillance (NNIS) system; in 2003, 59.5% of S. aureus isolates in NNIS ICUs were MRSA . 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Methicillin-Resistant Staphylococcus aureus (MRSA) Among Intensive Care Unit Patients, 1995-2004 60 50 40 30 20 10 Year 20 04 20 03 20 02 20 01 20 00 19 99 19 98 19 97 19 96 0 19 95 Percent Resistance 70 Source: National Nosocomial Infections Surveillance (NNIS) System Vancomycin-Resistant enterococcus (VRE) A similar rise in prevalence has occurred with VRE . From 1990 to 1997, the prevalence of VRE in enterococcal isolates from hospitalized patients increased from <1% to approximately 15% VRE accounted for almost 25% of enterococcus isolates in NNIS ICUs in 1999 and 28.5% in 2003 . Vancomycin-Resistant Enterococci (VRE) Among Intensive Care Unit Patients,1995-2004 30 25 20 15 10 5 Year 20 04 20 03 20 02 20 01 20 00 19 99 19 98 19 97 19 96 0 19 95 Percent Resistance 35 Gram-negative resistant Bacteria -GNB resistant to ESBLs, fluoroquinolones, carbapenems, and aminoglycosides also have increased in prevalence. *For example, in 1997, the SENTRY Antimicrobial Surveillance Program found that among K. pneumoniae strains isolated in the United States, resistance rates to ceftazidime and other third-generation cephalosporins were 6.6%, 9.7%, 5.4%, and 3.6% for bloodstream, pneumonia, wound, and urinary tract infections, respectively . *In 2003, 20.6% of all K. pneumoniae isolates from NNIS ICUs were resistant to these drugs 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults 3rd Generation Cephalosporin-Resistant Klebsiella pneumoniae Among Intensive Care Unit Patients, 1995-2004 Percent Resistance 30 25 20 15 10 5 Year 20 04 20 03 20 02 20 01 20 00 19 99 19 98 19 97 19 96 19 95 0 Source: National Nosocomial Infections Surveillance (NNIS) System Year 20 04 20 03 20 02 20 01 20 00 19 99 19 98 19 97 19 96 40 35 30 25 20 15 10 5 0 19 95 Percent Resistance Fluoroquinolone-Resistant Pseudomonas aeruginosa Among Intensive Care Unit Patients, 1995-2004 Campaign to Prevent Antimicrobial Resistance Clinicians hold the solution! Risk factors that promote antimicrobial resistance in healthcare settings include Extensive use of antimicrobials Transmission of infection Susceptible hosts Key Prevention Strategies Clinicians hold the solution! " Prevent infection " Diagnose and treat infection effectively “ Use antimicrobials wisely “ Prevent transmission Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Selection for antimicrobialresistant Strains Resistant Strains Rare Antimicrobial Exposure Resistant Strains Dominant Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Emergence of Antimicrobial Resistance Susceptible Bacteria Resistant Bacteria Resistance Gene Transfer New Resistant Bacteria Plasmids •Rings of extra chromosomal DNA •Can be transferred between different species of bacteria •Carry resistance genes •Most common and effective mechanism of spreading resistance from bacteria to bacteria (Bacterial Conjugation) Beta-Lactamases: What are they ? •Enzymes produced by certain bacteria that provide resistance to certain antibiotics •Produced by both gram positive and gram negative bacteria •Found on both chromosomes and plasmids Beta-lactam Antibiotics Examples •Penicillins: –Penicillin, amoxicillin, ampicillin •Cephalosporins: –Cephalexin,Cefuroxime,Ceftriaxone •Carbapenems: –Imipenem, meropenem Beta-Lactamases Mechanism of Action •Hydrolysis of beta-lactam ring of basic penicillin structure •Hydrolysis = adding a molecule of H2O to C-N bond with enzyme action –This opens up the ring, thus making the drug ineffective! ESBL? •Resistance that is produced through the actions of beta lactamases. •Extended spectrum cephalosporins, such as the third generation cephalosporins, were originally thought to be resistant to hydrolysis by beta-lactamases! •Not so! –mid 1980's it became evident that a new type of betalactamase was being produced by Klebsiella & E coli that could hydrolyze the extended spectrum cephalosporins. –These are collectively termed the •'extended spectrum beta-lactamases '( ESBL's ) ESBL? The story is more complicated…. •Multiple antimicrobial resistance is often a characteristic of ESBL producing gram-negative bacteria. •Ceftazidime •Cefotaxime •Ceftriaxone •Aztreonam •Genes encoding for ESBLs are frequently located on plasmids that also carry resistance genes for: •Aminoglycosides •Tetracycline •TMP-SULFA •Chloramphenicol •Fluoroquinolones ESBL? If an ESBL is detected, all penicillins, cephalosporins, and aztreonam should be reported as “resistant”, regardless of in vitro susceptibility test results ESBL? However: ESBL producing organisms are still susceptible to: •Cephamycins: –Cefoxitin –Cefotetan •Carbapenems: –Meropenem –Imipenem Carbapenems are becoming the therapeutic option of choice ESBL? Take home message ESBLs are harbingers of multi-drug resistance Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Antimicrobial Resistance: Key Prevention Strategies Susceptible pathogen Pathogen Prevent Infection Prevent Transmission Infection Antimicrobial Resistance Effective Diagnosis & Treatment Optimize Use Antimicrobial Use 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Use Antimicrobials Wisely Prevent Infection 5. Practice antimicrobial control 6. Use local data 1. Vaccinate 7. Treat infection, not contamination 2. Get the catheters out 8. Treat infection, not colonization 9. Know when to say “no” to vanco 10. Stop treatment when infection is cured or unlikely Diagnose and Treat Infection Effectively Prevent Transmission 3. Target the pathogen 11. Isolate the pathogen 4. Access the experts 12. Break the chain of contagion 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Prevent Infection Step 1: Vaccinate Fact: Pre-discharge influenza and pneumococcal vaccination of at-risk hospital patients and influenza vaccination of healthcare personnel will prevent infections. Actions: give influenza / pneumococcal vaccine to atrisk patients before discharge get influenza vaccine annually 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 1: Vaccinate Need for Healthcare Personnel Immunization Programs: Influenza Vaccination Rates (1996-97) % Vaccinated All adults > 65 yrs. of age 63% Healthcare personnel at high risk* 38% All healthcare personnel** 34% 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 1: Vaccinate Need for Hospital-Based Vaccination: Post-discharge Vaccination Status of Hospitalized Adults Influenza Vaccine Pneumococcal Vaccine Age 18-64 years with medical risk* 17% vaccinated 31% vaccinated Age > 65 years* 45% vaccinated 68% vaccinated Hospitalized for pneumonia during influenza season** 35% vaccinated 20% vaccinated Population 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Prevent Infection Step 2: Get the catheters out Fact: Catheters and other invasive devices are the # 1 exogenous cause of hospital-onset infections. Actions: use catheters only when essential use the correct catheter use proper insertion & catheter-care protocols remove catheters when not essential 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 2: Get the catheters out Biofilm on Intravenous Catheter Connecter 24 hours after Insertion Scanning Electron Micrograph 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Diagnose & Treat Infection Effectively Step 3: Target the pathogen Fact: Appropriate antimicrobial therapy saves lives. Actions: culture the patient target empiric therapy to likely pathogens and local antibiogram target definitive therapy to known pathogens and antimicrobial susceptibility test results 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 3: Target the pathogen Inappropriate Antimicrobial Therapy: Impact on Mortality 600 17.7% mortality 500 Relative Risk = 2.37 (95% C.I. 1.83-3.08; p < .001) 400 300 200 42.0% mortality # Survivors # Deaths 100 0 Inappropriate Therapy Appropriate Therapy 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 3: Target the pathogen Inappropriate Antimicrobial Therapy: Prevalence among Intensive Care Patients 50% 45.2% 40% 34.3% 30% 20% Inappropriate Antimicrobial Therapy (n = 655 ICU patients with infection Community-onset infection 17.1% Hospital-onset infection Hospital-onset infection after initial community-onset infection 10% 0% Patient Group 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Diagnose & Treat Infection Effectively Step 4: Access the experts Fact: Infectious diseases expert input improves the outcome of serious infections. 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 4: Access the experts Infectious Diseases Expert Resources Infectious Diseases Specialists Healthcare Epidemiologists Clinical Pharmacists Infection Control Professionals Optimal Patient Care Clinical Microbiologist s Surgical Infection Experts Clinical Pharmacologists 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Use Antimicrobials Wisely Step 5: Practice antimicrobial control Fact: Programs to improve antimicrobial use are effective. 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Use Antimicrobials Wisely Step 6: Use local data Fact: The prevalence of resistance can vary by time, locale, patient population, hospital unit, and length of stay. 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Use Antimicrobials Wisely Step 7: Treat infection, not contamination Fact: A major cause of antimicrobial overuse is “treatment” of contaminated cultures. Actions: use proper antisepsis for blood & other cultures culture the blood, not the skin or catheter hub use proper methods to obtain & process all cultures Link to: CAP standards for specimen collection and management 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Use Antimicrobials Wisely Step 8: Treat infection, not colonization Fact: A major cause of antimicrobial overuse is treatment of colonization. Actions: treat bacteremia, not the catheter tip or hub treat pneumonia, not the tracheal aspirate treat urinary tract infection, not the indwelling catheter Link to: IDSA guideline for evaluating fever in critically ill adults 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Use Antimicrobials Wisely Step 9: Know when to say “no” to vanco Fact: Vancomycin overuse promotes emergence, selection,and spread of resistant pathogens. 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 9: Know when to say “no” to vanco Evolution of Drug Resistance in S. aureus Penicillin Methicillin MethicillinPenicillin-resistant S. aureus resistant [1950s] [1970s] S. aureus S. aureus (MRSA) [1997] Vancomycin [1990s] Vancomycin- resistant S. aureus [ 2002 ] Vancomycin intermediateresistant S. aureus (VISA) Vancomycin-resistant enterococci (VRE) 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 10: Stop treatment when infection is cured or unlikely Use Antimicrobials Wisely Step 10: Stop antimicrobial treatment Fact: Failure to stop unnecessary antimicrobial treatment contributes to overuse and resistance. Actions: when infection is cured when cultures are negative and infection is unlikely when infection is not diagnosed 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 11: Isolate the pathogen Prevent Transmission Step 11: Isolate the pathogen Fact: Patient-to-patient spread of pathogens can be prevented. Actions: use standard infection control precautions contain infectious body fluids (use approved airborne/droplet/contact isolation precautions) when in doubt, consult infection control experts 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Prevent Transmission Step 12: Break the chain of contagion Fact: Healthcare personnel can spread antimicrobial-resistant pathogens from patient-topatient. 12 Steps to Prevent Antimicrobial Resistance: Hospitalized Adults Step 12: Break the chain of contagion Improved Patient Outcomes associated with Proper Hand Hygiene Chlorinated lime hand antisepsis Ignaz Philipp Semmelweis (1818-65) Prevention and Control of MDRO transmission Successful control of MDROs has been documented using a variety of combined interventions. These include: - Improvements in hand hygiene, - Use of Contact Precautions until patients are culturenegative for a target MDRO, - Active surveillance cultures (ASC), - Education, - Enhanced environmental cleaning, and improvements in communication about patients with MDROs within and between healthcare facilities. Infection control practices and the campaign to prevent multi-drug resistance in Palestine - Problem! Unrestricted use of antibiotics in the community: Role of physicians-evidence based guidelines and protocols Role of pharmacists-policies (antibiotics should not be over the counter drugs!) Role of public-education Role of the ministry of health-rules and regulations Infection control practices and the campaign to prevent multi-drug resistance in Palestine Problem! Lack of National Nosocomial Infection Surveillance (NNIS) system (governmental and non-governmental) Problem! Do we have adequate Infectious Diseases Expert Resources ? - Infectious Diseases Specialists - Infection Control Professionals - Clinical Pharmacologists - Clinical Microbiologists - Health care Epidemiologists Campaign to Prevent Antimicrobial Resistance in Healthcare Settings Prevention IS PRIMARY! Protect patients…protect healthcare personnel… promote quality healthcare! The End! •Bacteria have evolved numerous mechanisms to evade antimicrobial drugs. •Chromosomal mutations are an important source of resistance to some antimicrobials. •Acquisition of resistance genes or gene clusters, via conjugation, transposition, or transformation, accounts for most antimicrobial resistance among bacterial pathogens. •These mechanisms also enhance the possibility of multi-drug resistance.