Documentation Presentation
advertisement
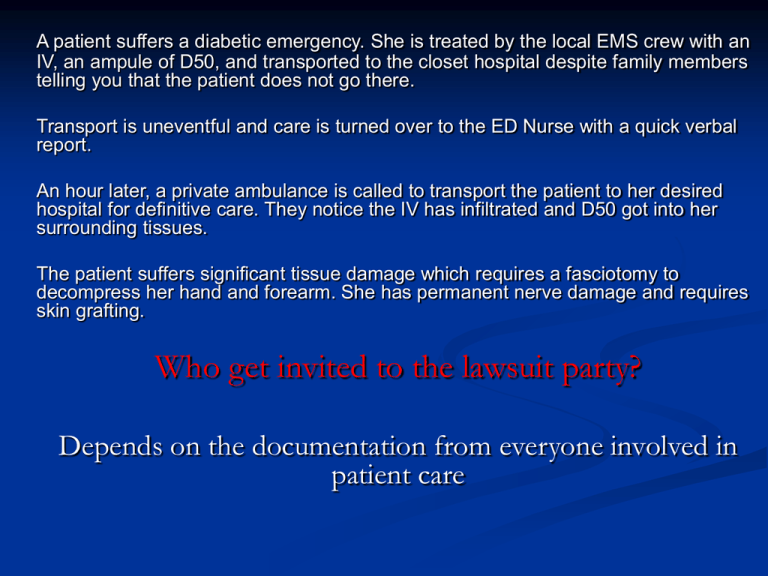
A patient suffers a diabetic emergency. She is treated by the local EMS crew with an IV, an ampule of D50, and transported to the closet hospital despite family members telling you that the patient does not go there. Transport is uneventful and care is turned over to the ED Nurse with a quick verbal report. An hour later, a private ambulance is called to transport the patient to her desired hospital for definitive care. They notice the IV has infiltrated and D50 got into her surrounding tissues. The patient suffers significant tissue damage which requires a fasciotomy to decompress her hand and forearm. She has permanent nerve damage and requires skin grafting. Who get invited to the lawsuit party? Depends on the documentation from everyone involved in patient care Documentation “If you didn’t write it on your patient care report, you didn’t do it.” Objectives Importance of Documentation Identify Data on the PCR Types of Documentation Formats Consequences for Poor Documentation Special Considerations Grammar and Punctuations Electronic Reporting and WARDS Why so Important Permanent part of the patients medical record Written Proof that you did something Written Testimony Quality Assurance Operations Research “The content and completeness of the prehospital care report directly affects the lawyer’s impression of the incident and influences his decision of whether or not to file a lawsuit.” Richard A. Lazar, JD Elements of the PCR Date of the Run Type of call TIMES Received Enroute Scene Patient Contact Transport Destination Medical History Allergies Medications Chief Complaint Trauma Mechanism Safety Equipment Vital signs Blood Pressure Pulse Respirations Lung Sounds Cap refill Blood Glucose Pupils Organization S. O. A. P C.H.A.R.T CHRONOLOGICAL S.O.A.P What happened? What did you find? What do you think? What did you do? (S) (Subjective) What happened? Medic 27 responded emergent on a 39 year old female who had a syncope from the standing position. Patient reports that she was at a party when she began to feel nauseous. Walked into back room and then passed out on floor. Witnesses report patient slumped forward on to a couch and then slid backward to a carpeted floor. Patient also reports that she recalls waking up on floor, feeling cold and shivering. Patient moved to bed with assistance. A bystander called 911 for assistance. (O) (Objective) What did you find? Upon initial contact, patient laying in bed in bedroom. Alert and oriented to name, place, time and event. Skin warm and dry with normal color and tone. Mild muscle tremors (shivers) in arms and legs. Patient does report feeling cold. Head normocephalic without abnormality on visualization or palpation. Neck midline and intact without pain on palpation or movement. Thoracic, lumbar and sacral spine intact without pain on palpation or spontaneous movement. My Way Level of Consciousness Airway, Breathing, Circulation Skin color and temp Head to Toe Exam Pertinent Negative (A) Assessment (What do you think?) Patient transported to Hospital with seizure like activity Not a diagnosis Protocol Followed (P) Plan What did you do? Patient transported non-emergent to Aurora Medical Center emergency room. Patient transported without change in status or level of consciousness. Patients treatment plan included full secondary assessment, detailed neurological examination, vital signs, cardiac monitoring, pulse oximetry and supplemental oxygen. Following hand off report to staff, patient left in hospital bed with rails up and staff in attendance. C. H. A. R. T Chief Complaint History Allergies R/x-Treatment Transport (C) Chief Complaint Medic 27 responded emergent on a 39 year old female who had a syncope from the standing position. (H) History Present Illness HPI (history of present illness/injury) PMH (past medical history) PQRST, AMPLE, MOI, Onset Signs and Symptoms (A) Assessment Include both negative and positive findings Responses the patient has to your assessment such as the presence or lack of pain and/or the presence or lack of sensation. Diagnostic Testing ECG Pulse Oximetry Capnography Blood Glucose Monitoring (R) Rx-Treatment Document your treatment Responses from the Patient to Rx Changes in Patients condition Example “Pain decreased to 5/10 from 7/10 after NTG administered. (T) Transport Where did you go Change in condition during transport Alteration from Protocol Who did you turn care over to (Name if Possible) Ie: RN Robinson Patency of airway and IV fluids CHRONOLOGICAL “Write like your brain thinks it” Dispatched non-emergent to University Hospitals Emergency Educations center for a transport to UW ER. Arrived on floor and met by staff, who advised us that the patient was suffering from severe PES. (Paramedic Education Syndrome). Patient is Mr. D, a 48 yo male with hx of PES and CHF, who presented with chest pain and dyspnea…... Errors and Falsifications Avoid Errors Admit when you made a mistake Revise if necessary Note date and time of revision Keep original document Include purpose of the revision Only the original author can make the correction Errors and Falsifications Always be honest and through in your documentation. Corrections: Add a supplement on electronic reports One line across the error, initial the mistake and make the corrections on written reports Complete reports as soon as possible. Lost reports have HUGE legal implications Don't keep copies of your reports. HIPPA What Happens on the Ambulance stays on the ambulance. Health Insurance Portability Privacy Accountability HIPPA Protects the security and privacy of all medical records and other health information used or shared in any form Protects patients rights by giving access to health information and control over how it is used PHI Protected Heath Information Information that relates to: The health of an individual Health care provided to that individual Payment of heath care provided What can be shared Health Insurance Company my need information to process a claim Caregivers involved with direct care Quality Assurance when necessary Special Considerations Exposure and Injury Mass Casualty Interfacility Transports Refusals Mass Casualty Events Documentation may have to be postponed Follow Local Policy and Procedure Comprehensive run report must be completed for each patient when time permits Refusal of Care Potential for Liability Good Documentation Make it clear. Refusal of Care The litigation rate for EMS has been steadily increasing. According to one study patients evaluated by paramedics but not transported to the hospital account for 50 to 90% of EMS lawsuits”. Documentation is your best defense.” Documentation: Physical Findings. The advice you give the patient about being transported and the associated risks for not being transported Clinical indications that patient is competent to make a rational decision Signatures of the patient and witness Full narrative Advise to call 911 if condition changes What not to say: Do not at any time attempt to talk the patient out of going to the hospital. If you feel strongly that the patient should be seen, make every attempt to convince them they should be seen. Don’t say ‘ I agree you don’t need to go” even if you agree A patient suffers a diabetic emergency. She is treated by the local EMS crew with an IV, an ampule of D50, and transported to the closet hospital despite family members telling you that the patient does not go there. Transport is uneventful and care is turned over to the ED Nurse with a quick verbal report. An hour later, a private ambulance is called to transport the patient to her desired hospital for definitive care. They notice the IV has infiltrated and D50 got into her surrounding tissues. The patient suffers significant tissue damage which requires a fasciotomy to decompress her hand and forearm. She has permanent nerve damage and requires skin grafting. Initial Transport Agency-CFD First Receiving Hospital-St Anthony Hospital Wojcik v. City of Chicago, 702 NE 2d 303 - Ill: Appellate Court, 1st Dist., 2nd Div. 1998 Lets Finish up Be Professional Accurate Consistent Through Clear Brief Paint the Picture Collaborative Legible, spelling correct Tell the Truth Don’t duplicate info Follow Protocols Plain Language Relevant Information “The JURY” Have your partner review