Pain Management in the Geriatric Population
advertisement

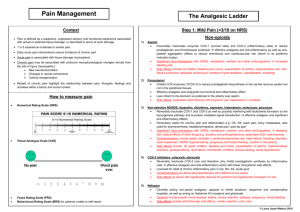
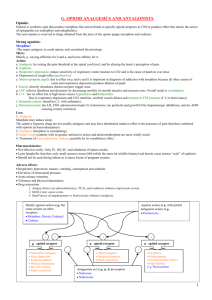
Pain Management in the Geriatric Population Ali R. Rahimi,MD,FACP,AGSF Professor of Medicine Mercer University School of Medicine Clinical Professor University of Georgia School of Pharmacy Pain: Webster: a : usu. localized physical suffering associated with a bodily disorder; also : a basic bodily sensation induced by a noxious stimulus, received by naked nerve endings, characterized by physical discomfort (as pricking, throbbing, or aching), and typically leading to evasive action b : acute mental or emotional distress or suffering Urandictionary.com: What happens when you reach into the blender to dislodge a stuck icecube without unplugging it first. Pain & elderly Pain is what many people say they fear most about dying. Pain is undertreated at the end of life Older patients are likely to have a increased pain threshold but to be less toleant to severe pain. PAIN IS MC REASON FOR INDIVIDUALS TO SEEK MEDICAL CARE Definitions: • Addiction: Psychological dependence on a drug. • Physical Dependence: Development of physical withdrawal reaction upon discontinuation or antagonism of a drug • Tolerance: Need to increase amount of drug to obtain the same effect • Pseudoaddiction: Behavior suggestive of addiction occurring as a result of undertreated pain Pain can be assoc w/: Psychologic and physical disability a source of individual suffering Familial distress Pain in nursing home patients • 30% reported daily pain • 26% of these patients received no analgesia • Only 26% of them received strong opioids What predicted inadequate pain management? 1 2 3 Advanced age: >85 years old Poor cognitive function Minority status Bernabei (1998), N = 13,625 cancer patients Obstacles of geriatric pain management: Accessibility to treatment 2. $$$ 3. SEs 4. Comorbidities 1. 5. 6. 7. 8. 9. Ex- NSAID use in pt w/ HTN or heart disease Ex- Acetominophen use in Liver dz pt Interactions with the current meds Pts with cognitive impairments The assumption that pain is normal party of aging Practitioner’s bias (pain seeker..) fear of legal repercussions… It’s a risk factor! Myofacial deconditioning Decreased activity bc of pain Gait distrubances INJURIES from falls Types of pain: Nociceptive pain- Nerves responding appropriately to a painful stimulus Neuropathic pain- results from NS dysfunction, and may originate centrally or peripherally Somatic pain- originates in the skin, bones, myo, and connective tissue, and usually is located specifically. Visceral pain- originated in internal body structures and organs, and is located more genearlly. Neuropathic pain: • Origin: Nerve damage • Palliates/potentiates: Set off by unusual stimuli, light touch, wind on skin, shaving (trigeminal neuralgia) • Quality: Electric, burning, tingling, pins & needles, shooting (system isn’t working right) • Radiation: Nerve-related pattern Nociceptive Pain: • Origin: Easier to treat than Neuropathic!! Tissue damage • Palliates/potentiates: Worse with stress, pressure Responds better to opioids, NSAIDs • Quality: Sharp, dull, stabbing, pressure, ache, throbbing • Radiation: Occasionally radiates (less well-defined), but not along an obvious nerve distribution Differentiating between somatic, visceral, and neuropathic pain is ESSENTIAL to proper tailoring of pain treatments Specific Goals: 1- 2 3- determining the presence and cause of pain identifying exacerbaing comorbidities reviewing beliefs, attitudes and expectations regarding pain Overall: to decrease pain and increase function and quality of life! Common pain syndromes in elderly MUSCULOSKELETAL CONDITIONS OA Degenerative disk dz Osteoporosis & Fxs Gout RHEUMATOLOGIC CONDITIONS: RA Polymyalgia rheumatics Fibromyalgia NEUROPATHIC CONDITIONS: Biabetic neuropathy Postherpatic neuralgia Trigeminal neuralgia Central poststroke pain Radicular pain secondary to degenerative disc dz Aging takes a toll… In the PNS: Loss of myelinated and unmyelinated fibers Axonal atrophy common Nerve conduction and endoneural blood flow are reduced w/ age Less nerve regeneration observed progressive loss of serotonergic and noradrenergic neurons in the superficial lamina of the spinal dorsal horn, and bc serotonin and norepineph have important roles in the descending inhibitory control pathways, such a loss may upset the natural endogenous pain-suppressing mechanisms. Therefore, pain treatment of the elderly obviously differs from that of young patients! Models of the prevalence of pain 1- Pain increases with age and then decreases at older ages (ie, 70 and beond). They suppose that this pain typically has a mechanical etiologic component and possibly is assoc with the occupational envioroment 2- pain increases with age. This has a mechanical etilogic component but also an assoc with increasing prevalence of degenerative dz, particulary at older ages. 3- age-independent pain that (obviously) lacks a mechanical etiologic component. (ie- risk factors that are constant throughout the life course) 4- A decrease in pain prevalence at older ages. It is not clear whether the trajectory is caused by age-related changes in pain and pain perception, or by changes in pain reportin. Effect of age on human (via clinical observation): Clinical observation examples: increased incidence of silent MI in elderly patients atypical presntation of an inflamed appendix, (absence of RLQ pain) Study example: (pg 208) Yunis compared elderly and young patients with fibromyalgia. They found that chronic head aches, anxiety, tension, mental stress and poor sleep were all less common in the elderly patients w this condition. Lonliness and pain The comorbidity of pain and psychological distress is WELL DOCUMENTED The feeling of lonliness is the single most important predictor of psychologic state of distress in older persons. A study by Eisenberger supported the hypothesis that Pain distress and social distress share neurocognitive substrates Study on page 193 Sleep and pain Multiple studies have demonstrated the comorbidity of pain and sleeplessness Pain is among the best predictors of sleep disturbances among older adults Thus, it appears that improved pain leads to improved sleep, and impoved sleep leads to improved pain! Study =pg 193 HOW TO QUANTIFY THE PAIN? Details! •Onset •Duration •Freq •Intensity •Locaiton •Contributing factors Troubleshooting pain assessment: Demented/Confused patient: Have to look for: Agitation, agressiveness, etc. Pain control vs quality of life OVERALL GOAL: to abolish pain with minimal adverse effects. Ex- Patient with COPD and pain: o Cant treat their pain too vigorously bc we will exacerbate the COPD symptoms Treating the pain: Pharmacologic approaches: Opiods Anti-inflammatory agents (asa, NSAIDS, cyclooxygenase [COX-2] inhinitors, steroids) Acetaminophen Tramadol Myo relaxants Tricyclic antidepressants SRIs Antielileptic drugs (AEDs) Non-pharmocologic approaches: Behavioral therapy Support groups Spiritual counseling Radiation therapy Physical therapy Acupuncture Psychotherapy Hypnosis Splinting Cultural healing rituals Surgical correction Heat packs Cold packs Prayer Meditation Community resources How to choose an analgesic? Severe pain: Opioids Moderate to severe: Use in combo with opioids Mild to Moderate pain: Acetominophen Aspirin NSAIDS Drug Classes Salicylates: Salicylates Analgesic, antipyretic, anti-inflammatory and anti-rheumatic activity. MOA: Inhibits prostaglandin synthesis producing analgesic. antiplatelet effect by inhibiting the production of thromboxane Much higher levels needed for anti-inflammatory effect than for anti-platelet, anti-pyretic and analgesic effects. Metab: Gut & plasma (ASA); liver (salicylate) Excrition: renal Can cause: GI irritation and bleeding. Use w caution in ppl with hx of gastric or peptic ulcercs. CYP450 Acetominophen analgesic and antipyretic agent MOA: Inhibits central prostaglandin synthesis with minimal inhibition of peripheral prostaglandin synthesis Antipyretic effect by direct action on the hypothalamic heat-regulating center Benefits: Absorbed rapidly No gastric mucosa effects No effect on platelet aggregation Metab by liver Excretion: urine (metabolites can accumulate w renal impairment) Hepatotoxic Can take 500-1000mg orally q 6hr Older pts and Pts with liver dz: do not exceed 2g/day NSAIDS Antipyretic, analgesic and anti-inflammatory properties MOA: Reduce central and peripheral prostaglandin synthesis but they do not inhibit the effects of the prostaglandins already present, resulting in analgesia, followed by relatively delayed anti-inflammatory effects. Metab: liver 1.5 times higher risk of GI bleeding Excretion: urine Adverse effects: n/v, bleeding Hepato and nephrotoxicity (more so in the elderly) Concurrent use of PPI for prevention NSAID: 18 available in the US All NSAIDS have similar mechanism of action BUT differ in: Potencies Time to onset Duration Response among patients Common uses: After surgeries Painful chronic conditions (ex- OA) Benefit more notable when used in combo w an opiod. Opiod SEs like sedation, n/v decreased when used w NSAID COX 2 NSAIDS: Purpose in pharmacology unclear Only available: celecoxib Cox2 and NSAIDS are CI in pts with cardiac disease! estimated to be responsible for up to 20 percent of hospital admissions for congestive heart failure. BY INCREASING SYSTEMIC VASCULAR RESISTANCE and REDUCING RENAL PERFUSION OPIOID: a chemical that works by binding to opioid receptors, which are found principally in CNS and the GI. Hence, the GI Ses Effects: decreased perception of pain decreased reaction to pain increased pain tolerance Opioids Cornerstone of the analgesic regimen for mod-sev pain • MC ones: • Morphine • Oxycodone • Hydromorphone • Transdermal fentanyl 3 Main Opioid receptors: Mu, delta and kappa receptors. Mu agonists: produce analgesia affect numerous body systems influence mood & reward behavior Delta agonists produce analgesia not a lot on market Kappa agonists produce analgesia may cause less resp depression and miosis psych effects, can produce dysphoria Opioids LACK the adverse renal, and hematologic effects of NSAIDs MU-receptor agonists are MC used although drugs may interact with more than one type of receptor. Ex- the mu receptor antagonist and kappa receptor agonist drugs were deigned to cause less respiratory depression. Opioids pharmacokinetics Pharmacokinetic properties of an opioid can dictate the circumstance which they are appropriate in: Ex- Lipid-soluble drug such as fentanyl, which diffuse rapidly acros the BBB, are preferable if analgesia is required immediately before a short, painful procedure. Elimination half life very short: So, steady state reached in a day or less! Thus, you can adjust the dose daily knowing we are seeing it’s effect. Adverse effects: Respiratory depression sedation N/V Constipation Urinary retention Itching 1. Respiratory depression Caused by directly acting on respiratory center Naloxone is specifically used to counteract life-threatening depression of the central nervous system and respiratory system Therapeutic doses of morphine can affect: Resp rate, minute volume tidal exchange Although, tolerance to this effect is usually achieved with repeated doses of opioids. Avoid/Monitor in pts with: Imparied resp function Sleep apnea Or bronchial asthma Not common if begin with low dose and titrate upward!! 2. Nausea and vomiting MC SE Likely due to changing blood serum levels , not problem @ steady state The freq of nausea and vomiting is higher in ambulaory patients (vestibular component?) Antiemetics (metoclopramide or droperidol) can be used along with the opioid. 3. Constipation: Acts on receoptors of GI tract and spinal cord to produce decrease in peristalsis and intestinal secretions Tolerance to this effect is not common Result- prescribe prophylactic laxatives … use stood softener AND a stimulant laxative. 4. Urinary retention causes increased smooth muscle tone increases sphincter tone 5. Itching Mechanism not fully known~ Hypot: related to the release of histamine from mast cells. If itching is with rash- consider allergy. Can use an antihistamine to treat this Opioids: Morphine Morphine = standard of opioids BUT if pt doesnt respond well, they may switch to an equianalgesic dosage of: Hydroporphone Oxycodone Fentanyl Oxymorphone Or methadone If pt has diminished renal function, they may benefit from: Oxycodone or hydromorphone (bc these don’t have clinically significant active metaolites) Opioid Combos~ Full opioid agonists: Morphine Hydrocodone Codeine Dextropropoxyphene Typically combined with acetaminophen or an NSAID Acetaminophen con Codeine • Advantages: Low regulatory control Inexpensive Widely available • Disadvantages: 10% cannot convert codeine to morphine Many drugs interfere with conversion Acetaminophen with Oxycodone, Hydrocodone • Oxycodone combination contains 325 mg acetaminophen • Hydrocodone combination contains 500 mg acetaminophen • No clear advantage between the two Three mu=receptor agonist to avoid whenever possible!! .. Meperidine 2. Propoxyphene 3. codeine 1. 1.Meperidine (DEMEROL) Low potency relative to morphine A short duration of action – so have to dose it more frequently And a toxic metabolite (normeperidine) Ex- meperidine 75mg = 5-7.5 mg of morphine can cause irritability and seizures 2. Propoxyphene (DARVOCET) treat mild to mod pain Toxicities assoc with it’s primary metabolite: norpropoxyphene 1. can cause cardiotoxicity and pulmonary edema Half life: 6-12 hour;Metabolite half life 30-36 hours 2. Pts with Dec Renal function or pts getting repeat doses: higher risk Puts geriatric pts at higher risks of falls (d/t CNS effects) 3. 1. 4. [ study found that propoxy users have twofold higher risk for hip frature compared with nonusers of analgesics ALSO, it has no clinical advantage over nonopioid analgesics such as acetominaphen PG 289 ] 3. Codeine Must be converted to morphine by means of the cytochrome P-450 pathway to provide analgesia. Lots of Caucasians are poor metabolizers of this isoenzyme -thus cant make the conversion! So, they do not get any of the codeine’s benefit but still suffer the Side effects. Principles of opioid use: 1. 2. 3. 4. 5. 6. No ceiling effect Dose to pain relief without side effects Give orally when possible Sub-cutaneous administration is basically equivalent to intravenous (and preferable) Treat constipation prophylactically Full opioid agonists are best choice for severe pain.. Where to start? Treating Chronic pain: Basal pain medicine plus a different therapy for spikes: Predictable spikes - Short-acting agent prior to event Unpredictable spikes - Short-acting agent readily available (prn) Treating Neuropathic Pain; Opioids and NSAIDS less effective Classes of Agents 1. Tricyclic for dysesthetic pain 2. Anticonvulsants for shooting pain 3. Steroids to decrease peri-tumor edema Tricyclic for dysesthetic pain Dysesthesia is pain not experienced by a normal nervous system. Eg- neuropathic burning from chemotherapy Considered "Dante-esque" pain. • Amitriptyline • Nortriptyline • Desipramine Anticonvulsants for shooting pain Gabapentin Pregabalin Steroids to decrease compression Nerve infiltration by tumor or spinal cord compresion: Corticosteroids Deamethasone Prednisone *Usu used for pts near end of Life bc of detrimental SE of Long term steroid use. Opioid analgesics available in US Mu agonists Alfentanil Codeine Hydrocodone Ydromorphone Fentanyl Levorphanol Meperidine Methadone Morphine Opium Oxycodone Oxymorphone Remifentanil Sufentanil Tramadol Kappa agonist/mu antagonist Butorphanol Nalbuphine Pentazocine Mu antagonists Nalmefene Naloxone Naltrexone Mu partial agonist/kappa antagonist Buprenorphine When to refer: Pain not respsoning to opoiods at typical doses Neuropathic pain not responding to first line treatments Comples methadone management issues Intolerable side effects from oral opioids Severe pain from bone mets For a surgical or anesthesia-based procedure, intrathecal pump, nerve block, or rhizotomy When to admit: For severe exacerbation of pain that is not responsive to previous stable oral opioid around-the-clock plus breakthrough doses. Pateints whose pain is so severe that they cannont be cased for at home Uncontrollable side effects from opioids, including nausea, vomiting, and altered mental status Good to know.. Older individuals tend to be more sensitive to benzodiazepines and opiods. Pain from bone mets more susceptible to NSAID pain relief than opioids The 1998 guidelines recommended earlier use of narcotics than is typical for treatment of younger patients because of the significant toxicities assoc with NSAIDS. Trigeminal neuralgia Characterized by: severe, unilateral facial pain described as lancinating electrics shock-like jolts in one or more distributions of the trigeminal nerve. Maxillary and Mandibular divisions = MC Careful clinical evaluation and MRI is recommended Postherpetic neuralgia Follows outbreak of Herpes zoster Sensory findings: Allodynia (wind against skin hurts, sheet on area hurts etc) hyperalgesia Post stroke pain An underrecognized consequence following storke May present as shoulder pain in the paretic limb or present as central poststroke pain. Characterized as pain that is severe and persistnet w accompanying sensory abmomalities Ex- the guy from Oceanside. Metastatic bone pain Bone pain that is worse at night, when laying down or not assoc with acute injury Pain that gradually but rapidly increase in intensity or with weight-bearking or activity. Freq sites: Hips, vertebrae, femur, ribs, and skull Temporal Arteritis: More than 95% of TA are ppl >50 Presentation: New onset headache, malaise, scalp tenderness and jaw claudication PE: indurated temporal arterly that is tender with a diminihed or abent pulse Irreversible bliness is consequence of untreted.. So timely assesment and tx is Pain perception in rats: When nociception is tested in mice using an electrical current, it seems that there are age related changes in nociception . The graphic representaion of electical thresholds needed to induce a vocal reponse was of a U-shap pattern. (high pain tolerance in young and old- lower in the middle aged) Effect of age on human experimental pain 50 studies total 21 concluded an increase in pain threshold with advancing age 3 reporeted a decrease 17 noted no change However, Temporal vs Spatial summation: It was fround that temopral summation to a heat pain stimulus, for example, is more pronounced in the elderly as compared with younger subjects. Whereas spatial summation is not significantly influenced by age.