Surgical Management of the Inguinal Hernia
advertisement

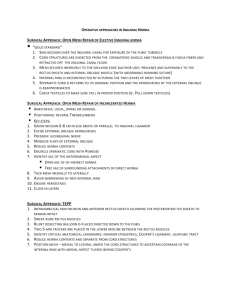
Surgical Management of the Inguinal Hernia Jerry G Gaston DO FACOS Mid-Year Meeting ACOS April 2014 Surgeon Disclaimer The following presentation is made on behalf of Davol Inc., and contains the opinions of, and personal surgical techniques practiced by Dr. Gaston. Any discussion regarding Davol products during the presentation is limited to information that is consistent with the FDA approvals or clearances for those products. The opinions and techniques presented herein are for informational purposes only and the decision of which techniques to use in a particular surgical application should be made by the surgeon based on the individual facts and circumstances of the patient and previous surgical experience. Consult product labels and insert for any indications, contraindications, hazards, warnings, precautions, and instructions for use. Dr. Gsston is a paid consultant for Davol, Takeda, and Myraid. 2 General 770,000 performed in US each year Indirect inguinal hernia most common Tension free Mesh Reoccurrence Chronic pain Anatomy Classification Direct Enters canal through posterior wall Weakening of the abdominal musculature Medial to the inferior epigastric vessels Indirect Enters canal through the deep inguinal ring Congenital – failure of the processus vaginalis to regress and fuse Femoral Inferior to Inguinal ligament Multiple presentations Nerves Iliohypogastric L1-L2 nerve roots Just medially and superior to ASIS Lies beneath the aponeurosis of the external oblique Supplies sensation to the skin of the suprapubic area Ilioinguinal L1 nerve root 2cm medial to the ASIS Lies beneath the aponeurosis of the external oblique Supplies sensation to the skin of the pubic region and the upper part of the scrotum or labia majoria Nerves Genitofemoral Genital branch and femoral branch L2-L3nerves Enters at the deep ring Genital branch-scrotum and medial aspect of the thigh Femoral branch-skin of the proximal anterior thigh Repairs Bassini Marcy Shouldice McVay (Cooper Ligament) Laparoscopic Lichtenstein Mesh Kugel Plug and patch PHS Repairs To fix or not to fix Mesh Approach Fix or not to fix Data confirms that a strategy of watchful waiting is a safe and acceptable option for men with minimally symptomatic or asymptomatic hernias. Fitzgibbons group trial Glasgow group in UK Mesh Cochrane data 2001 – 50-75% reduction in the risk of recurrence with the use of mesh PTFE Mesh plug and patch Prolene hernia system Kugel 3D max Approach Anterior Posterior Anterior Plug and Patch Posterior Kugel Posterior approach No fixation Ring Nerve avoidance Previous repair preperitoneal Laparoscopic 3D Max Laparoscopic TAPP vs TEP Nerve injury Lateral femoral cutaneous Closure of peritoneum Bilateral Complications Reoccurrence Chronic pain Mesh erosion Hemorrhage Nerve injury Vas Deferens injury Complications Reoccurrence Mesh vs no mesh Cochrane data 2001 – 50-75% reduction in the risk of recurrence with the use of mesh Less than 5% Complications Chronic Pain Nerve injury vs non nerve injury Long term Short term Work compensation Complications Mesh Erosion Bowel Bladder omentum Complications Hemorrhage Testicular vessels Inferior epigastric Cremestaric vessels Femoral Complications Nerve Injury Transection Manipulation Triple neurectomy Meshoma Complications Vas Deferens Difficult dissection Previous mesh Informed consent Scrotal hernia Conclusion Multiple different approaches Need a variety of tricks in the bag Do what you feel comfortable and can reproduce Know the surgical history Don’t be afraid to pull the NO CARD