PEEP
advertisement

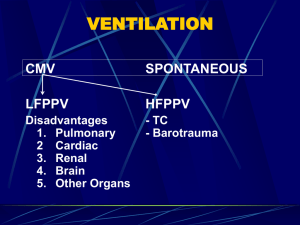
Positive End Expiratory Pressure Dr Muhammad Asim Rana Description • The ventilator applies a positive pressure at end • • • exhalation, thus supra-atmospheric pressure is maintained throughout the breathing cycle. When applied during spontaneous breathing the term CPAP is used When applied to a mechanically ventilated patient the term PEEP is used When applied to end of exhalation the term END-EXPIRATORY POSITIVE AIRWAY PRRESSURE is used • From a physiological point of view PEEP, CPAP & EPAP are identical • Different acronyms are delivered from the controls of the equipment used to provide them. Advantages 1. Recruits & stabilizes the collapsed alveoli 2. Increases the FRC & prevents expiratory collapse 3. Improves oxygenation in conditions associated with 4. 5. diffuse alveolar collapse & hypoxemia Used to decrease inspiratory work of breathing with auto-PEEP Decreases lung injury chances by maintaining minimum lung volume (minimizes shear forces associated with repetitive collapse & recruitment of injured alveoli) • Positive end-expiratory pressure (PEEP) has lung protective effects during mechanical ventilation in isolated lungs, and in intact and open-chest animals. • In intact healthy rats, edema and hemorrhage • • from ventilation with excessive lung volumes were substantially reduced when PEEP was used In a dog lung injury model lung injury was caused by ventilation with large Vt and low PEEP. This injury was reduced in animals ventilated with smaller Vts and higher PEEPs despite similar EILVs. • The effect of end-expiratory atelectasis on lung injury was evaluated in a rabbit surfactant-deficient model. Rabbits ventilated with negative end-expiratory pressure demonstrated greater alveolar capillary permeability, reduced lung compliance, and worse gas exchange than rabbits ventilated with PEEP. • These and other studies provide convincing • • evidence that PEEP has lung protective effects during mechanical ventilation. However, PEEP also can contribute to lung injury by raising EILV unless Vt is simultaneously reduced. Moreover, PEEP may cause circulatory depression from increased pulmonary vascular resistance and decreased venous return. Disadvantages 1. 2. 3. 4. 5. 6. 7. 8. Can impair cardiac output Increases risk of barotrauma esp,>15 cm Increases intracranial pressure Decreases renal & portal blood flow Can complicate data collection in pts of RHF Increases extra vascular lung water increases dead space if excessive May increase inspiratory work of breathing if over distention occurs Indications 1. Hypoxia with FiO2 > 0.5 in pts with diffuse B/L infiltrates (ARDS, Pul edema) 2. Cardiac surgery to prevent post operative mediastinal bleeding 3. Post operative atelactasis Determining the optimal level of PEEP • Determining the optimal level of PEEP in individual patients represents a difficult and tenuous balance between potential lung protective effects and deleterious effects on the lung and other systems. • Some investigators have used static or quasi-static pressure-volume curves of the respiratory system to explain the effects of ventilation at low EELV, to predict the effects of ventilation with higher PEEPs and EELVs, and to identify the best PEEP to apply during Conventional Ventilation to achieve lung protection. • The slope of the pressure-volume relationship represents compliance of the respiratory system. Compliance in the lower portion of the curve increases as airway pressure and volume rise, representing gradual recruitment of atelectatic portions of the lung. • This interpretation is supported by improved arterial oxygenation53 and CT evidence of increased lung aeration in ARDS patients. • The midpoint of the portion of the pressure-volume curve with increasing slope is frequently labeled “Pflex” and may represent the inspiratory airway pressure and volume where many lung units are open. • The mid-portion of the pressure-volume curve appears to be virtually rectilinear. This region of approximately constant compliance has been interpreted to represent a range of airway pressures and lung volumes in which little or no further recruitment occurs. • Some workers have advocated setting PEEP to approximately Pflex plus 2 cm H2O to prevent the closure of unstable lung units during expiration and, thus, to prevent injurious shear forces from ventilation with insufficient EELV. • This recommendation is supported by the results of studies suggesting that CV with PEEP that is less than Pflex may cause VALI. Setting PEEP • TECHNIQUE 1 • Begin at about 5 cm of H2O & increase in steps of 2 cm H2O until optimal PEEP is achieved– i.e, PaO2>60,FiO2<0.5, hemodynamic stability Achieving max static compliance of lungs Intrapulmonary shunt fraction < 15% Maximum VO2 (O2 consumption per unit of time) TECHNIQUE 2 • Sedate/paralyze the patient. Patient should not be making any respiratory excrsions • Suction the respiratory secretions • Ensure tight endotracheal/TT cuff seal • Increase FiO2 to 1.0 • Deliver single breath via ventilator to make patient achieve projected TLC • • • • • • • Disconnect patient from ventilator Allow patient to exhale to FRC Take a super-syringe (filled with 1.0 FiO2) Inflate lungs with 100 ml of O2 at a time pause for 2-3 seconds & measure Pel. Keep inflating with 100 ml of O2 at each step until a volume of 25 ml/kg is injected or airway pressure of 35 cm of H2O is reached or SaO2 starts falling < 87% An inflation curve plotting press & vol is made Best PEEP is slightly above lower inflection point. Thank You